Skin Integrity and Wound Care
Objectives
• Discuss the risk factors that contribute to pressure ulcer formation.
• Describe the pressure ulcer staging system.
• Discuss the normal process of wound healing.
• Describe the differences of wound healing by primary and secondary intention.
• Describe complications of wound healing.
• Explain the factors that impede or promote wound healing.
• Describe the differences between nursing care of acute and chronic wounds.
• Complete an assessment for a patient with impaired skin integrity.
• List nursing diagnoses associated with impaired skin integrity.
• Develop a nursing care plan for a patient with impaired skin integrity.
• List appropriate nursing interventions for a patient with impaired skin integrity.
• State evaluation criteria for a patient with impaired skin integrity.
Key Terms
Abnormal reactive hyperemia, p. 1188
Abrasion, p. 1190
Approximated, p. 1181
Blanching, p. 1177
Collagen, p. 1177
Debridement, p. 1199
Dehiscence, p. 1184
Drainage evacuators, p. 1208
Epithelialization, p. 1183
Eschar, p. 1179
Evisceration, p. 1184
Exudate, p. 1181
Fibrin, p. 1182
Friction, p. 1178
Granulation tissue, p. 1179
Hematoma, p. 1183
Hemorrhage, p. 1183
Hemostasis, p. 1182
Induration, p. 1188
Laceration, p. 1190
Normal reactive hyperemia, p. 1197
Pressure ulcer, p. 1177
Primary intention, p. 1181
Puncture, p. 1190
Purulent, p. 1183
Sanguineous, p. 1190
Secondary intention, p. 1181
Serosanguineous, p. 1190
Serous, p. 1190
Shearing force, p. 1196
Slough, p. 1179
Sutures, p. 1207
Tissue ischemia, p. 1177
Vacuum-assisted closure (V.A.C.), p. 1204
Wound, p. 1181
Wound contraction, p. 1222
![]()
Skin, the largest organ in the body, constitutes 15% of the total adult body weight (Wysocki, 2012). It is a protective barrier against disease-causing organisms and a sensory organ for pain, temperature, and touch; and it synthesizes vitamin D. Injury to the skin poses risks to safety and triggers a complex healing response. A nurse’s most important responsibilities include assessing and monitoring skin integrity; identifying problems; and planning, implementing, and evaluating interventions to maintain skin integrity. Once a wound occurs, it is critical to know the process of normal wound healing to identify the appropriate nursing interventions.
Scientific Knowledge Base
Skin
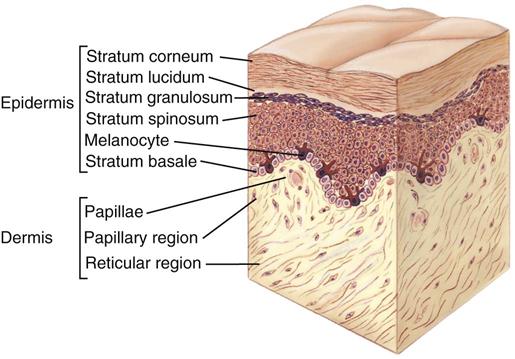
The skin has two layers: the epidermis and the dermis (Fig. 48-1). They are separated by a membrane, often referred to as the dermal-epidermal junction. The epidermis, or the top layer, has several layers. The stratum corneum is the thin, outermost layer of the epidermis. It consists of flattened, dead, keratinized cells. The cells originate from the innermost epidermal layer, commonly called the basal layer. Cells in the basal layer divide, proliferate, and migrate toward the epidermal surface. After they reach the stratum corneum, they flatten and die. This constant movement ensures replacement of surface cells sloughed during normal desquamation or shedding. The thin stratum corneum protects underlying cells and tissues from dehydration and prevents entrance of certain chemical agents. The stratum corneum allows evaporation of water from the skin and permits absorption of certain topical medications.
The dermis, the inner layer of the skin, provides tensile strength, mechanical support, and protection to the underlying muscles, bones, and organs. It differs from the epidermis in that it contains mostly connective tissue and few skin cells. Collagen (a tough, fibrous protein), blood vessels, and nerves are found in the dermal layer. Fibroblasts, which are responsible for collagen formation, are the only distinctive cell type within the dermis.
Understanding skin structure helps you maintain skin integrity and promote wound healing. Intact skin protects the patient from chemical and mechanical injury. When the skin is injured, the epidermis functions to resurface the wound and restore the barrier against invading organisms while the dermis responds to restore the structural integrity (collagen) and the physical properties of the skin. The normal aging process alters skin characteristics and makes skin more vulnerable to damage. Box 48-1 provides a summary of the changes in aging skin.
Pressure Ulcers
Pressure ulcer, pressure sore, decubitus ulcer, and bedsore are terms used to describe impaired skin integrity related to unrelieved, prolonged pressure. The most current terminology is pressure ulcer (Fig. 48-2), which is consistent with the recommendations of the pressure ulcer guidelines written by the Wound, Ostomy and Continence Nurses Society (WOCN, 2010). A pressure ulcer is localized injury to the skin and other underlying tissue, usually over a body prominence, as a result of pressure or pressure in combination with shear and/or friction. A number of contributing factors are also associated with pressure ulcers; the significance of these factors is yet to be elucidated (EPUAP and NPUAP, 2009). Any patient experiencing decreased mobility, decreased sensory perception, fecal or urinary incontinence, and/or poor nutrition is at risk for pressure ulcer development.

Many factors contribute to the formation of a pressure ulcer. Pressure is the major cause. Tissues receive oxygen and nutrients and eliminate metabolic wastes via the blood. Any factor that interferes with blood flow in turn interferes with cellular metabolism and the function or life of the cells. Prolonged, intense pressure affects cellular metabolism by decreasing or obliterating blood flow, resulting in tissue ischemia and ultimately tissue death.
Pathogenesis of Pressure Ulcers
Pressure is the major element in the cause of pressure ulcers. Three pressure-related factors contribute to pressure ulcer development: (1) pressure intensity, (2) pressure duration, and (3) tissue tolerance.
Pressure Intensity
A classic research study identified capillary closing pressure as the minimal amount of pressure required to collapse a capillary (e.g., when the pressure exceeds the normal capillary pressure range of 15 to 32 mm Hg) (Burton and Yamada, 1951). Therefore, if the pressure applied over a capillary exceeds the normal capillary pressure and the vessel is occluded for a prolonged period of time, tissue ischemia can occur. If the patient has reduced sensation and cannot respond to the discomfort of the ischemia, tissue ischemia and tissue death result.
The clinical presentation of obstructed blood flow occurs when evaluating areas of pressure. After a period of tissue ischemia, if the pressure is relieved and the blood flow returns, the skin turns red. The effect of this redness is vasodilation (blood vessel expansion), called hyperemia (redness). Evaluate an area of hyperemia by pressing a finger over the affected area. If it blanches (turns lighter in color) and the erythema returns when you remove your finger, the hyperemia is transient and is an attempt to overcome the ischemic episode, thus called blanching hyperemia (Pieper, 2012). However, if the erythematous area does not blanch (nonblanching erythema) when you apply pressure, deep tissue damage is probable.
Blanching occurs when the normal red tones of the light-skinned patient are absent. It does not occur in patients with darkly pigmented skin. The Task Force on the Implications for Darkly Pigmented Intact Skin in the Prediction and Prevention of Pressure Ulcers (Bennett, 1995) defined darkly pigmented skin as skin that “remains unchanged (does not blanch) when pressure is applied over a bony prominence, irrespective of the patient’s race or ethnicity.” Characteristics of intact dark skin that alert nurses to the potential for pressure ulcers are in Box 48-2.
Pressure Duration
Low pressure over a prolonged period and high-intensity pressure over a short period are two concerns related to duration of pressure. Both types of pressure cause tissue damage. Extended pressure occludes blood flow and nutrients and contributes to cell death (Pieper, 2012). Clinical implications of pressure duration include evaluating the amount of pressure (checking skin for reactive hyperemia) and determining the amount of time that a patient tolerates pressure (checking to be sure after relieving pressure that the affected area blanches).
Tissue Tolerance
The ability of tissue to endure pressure depends on the integrity of the tissue and the supporting structures. The extrinsic factors of shear, friction, and moisture affect the ability of the skin to tolerate pressure: the greater the degree to which the factors of shear, friction, and moisture are present, the more susceptible the skin will be to damage from pressure. The second factor related to tissue tolerance is the ability of the underlying skin structures (blood vessels, collagen) to assist in redistributing pressure. Systemic factors such as poor nutrition, increased aging, hydration status, and low blood pressure affect the tolerance of the tissue to externally applied pressure.
Risk Factors for Pressure Ulcer Development
A variety of factors predispose a patient to pressure ulcer formation. These factors are often directly related to disease such as decreased level of consciousness, the presence of a cast, or secondary to an illness (e.g., decreased sensation following a cerebrovascular accident).
Impaired Sensory Perception
Patients with altered sensory perception for pain and pressure are more at risk for impaired skin integrity than those with normal sensation. Patients with impaired sensory perception of pain and pressure are unable to feel when a portion of their body undergoes increased, prolonged pressure or pain. Thus the patient who can’t feel or sense that there is pain or pressure is at risk for the development of pressure ulcers.
Impaired Mobility
Patients unable to independently change positions are at risk for pressure ulcer development. For example, patients with spinal cord injuries have decreased or absent motor and sensory impairment and are unable to reposition off bony prominences.
Alteration in Level of Consciousness
Patients who are confused or disoriented and those who have expressive aphasia or other inability to verbalize or changing levels of consciousness are unable to protect themselves from pressure ulcer development. Patients who are confused or disoriented are sometimes able to feel pressure but are not always able to understand how to relieve it or communicate their discomfort. Patients in a coma cannot perceive pressure and are unable to move voluntarily to relieve pressure.
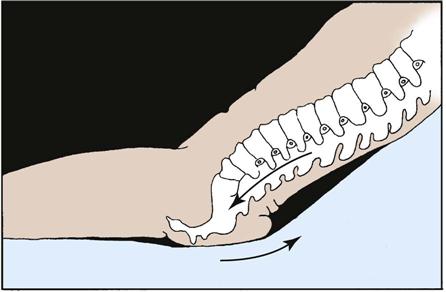
Shear
Shear force is the sliding movement of skin and subcutaneous tissue while the underlying muscle and bone are stationary (Bryant, 2012). For example, shear force occurs when the head of the bed is elevated and the sliding of the skeleton starts but the skin is fixed because of friction with the bed (Fig. 48-3). It also occurs when transferring a patient from bed to stretcher and the patient’s skin is pulled across the bed. When shear is present, the skin and subcutaneous layers adhere to the surface of the bed, and the layers of muscle and the bones slide in the direction of body movement. The underlying tissue capillaries are stretched and angulated by the shear force. As a result, necrosis occurs deep within the tissue layers. The tissue damage occurs deep in the tissues, causing undermining of the dermis.
Friction
The force of two surfaces moving across one another such as the mechanical force exerted when skin is dragged across a coarse surface such as bed linens is called friction (WOCN, 2010). Unlike shear injuries, friction injuries affect the epidermis or top layer of the skin. The denuded skin appears red and painful and is sometimes referred to as a “sheet burn.” A friction injury occurs in patients who are restless, in those who have uncontrollable movements such as spastic conditions, and in those whose skin is dragged rather than lifted from the bed surface during position changes.
Moisture
The presence and duration of moisture on the skin increases the risk of ulcer formation. Moisture reduces the resistance of the skin to other physical factors such as pressure and/or shear force. Prolonged moisture softens skin, making it more susceptible to damage. Immobilized patients who are unable to perform their own hygiene needs depend on the nurse to keep the skin dry and intact. Skin moisture originates from wound drainage, excessive perspiration, and fecal or urinary incontinence.
Classification of Pressure Ulcers
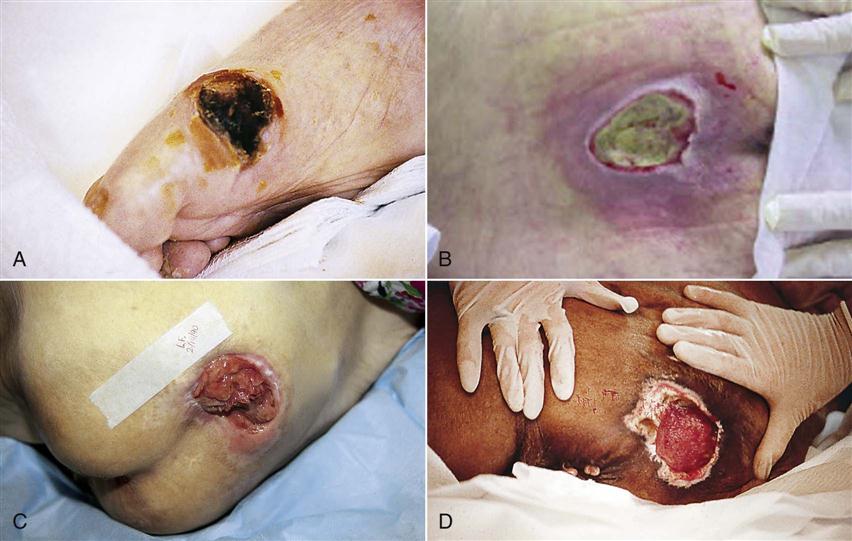
You need to assess pressure ulcers at regular intervals using systematic parameters to evaluate wound healing, plan appropriate interventions, and evaluate progress. Assessment includes depth of tissue involvement (staging), type and approximate percentage of tissue in wound bed, wound dimensions, exudate description, and condition of surrounding skin.
One method for assessment of a pressure ulcer is the use of a staging system. Staging systems for pressure ulcers are based on describing the depth of tissue destroyed. Accurate staging requires knowledge of the skin layers. A major drawback of a staging system is that you cannot stage an ulcer covered with necrotic tissue because the necrotic tissue is covering the depth of the ulcer. The necrotic tissue must be debrided or removed to expose the wound base to allow for assessment.
Pressure ulcer staging describes the pressure ulcer depth at the point of assessment. Thus, once you have staged the pressure ulcer, this stage endures even as it heals. Pressure ulcers do not progress from a stage III to a stage I; rather, a stage III ulcer demonstrating signs of healing is described as a healing stage III pressure ulcer (Pieper, 2012). The EPUAP and NPUAP have developed clinical practice guidelines for pressure ulcers and have advanced the following classification/staging system (EPUAP and NPUAP, 2009):
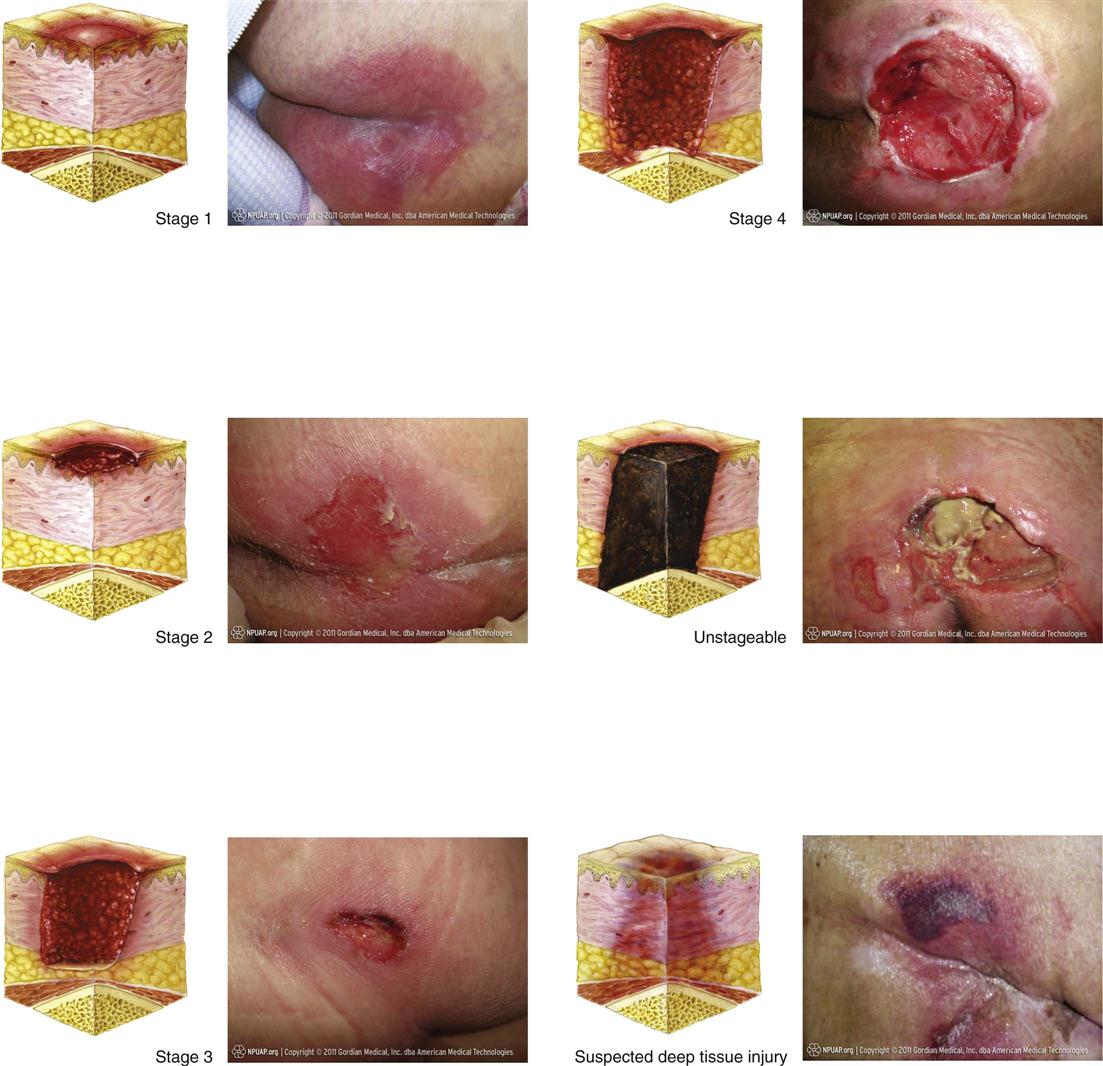
Stage I: Nonblanchable Redness of Intact Skin
Intact skin presents with nonblanchable erythema of a localized area usually over a bony prominence. Discoloration of the skin, warmth, edema, hardness, or pain may also be present. Darkly pigmented skin may not have visible blanching.
Further description: The area may be painful, firm, soft, warmer, or cooler than adjacent tissue. Stage I may be difficult to detect in individuals with dark skin tones. It may indicate “at-risk” persons (Fig. 48-4, A).
Stage II: Partial-thickness Skin Loss or Blister
A partial-thickness loss of dermis presents as a shallow open ulcer with a red-pink wound bed without slough. It may also present as an intact or open/ruptured serum-filled or serosangineous filled blister.
Further description: Stage II presents as a shiny or dry shallow ulcer without slough or bruising. This stage should not be used to describe skin tears, tape burns, incontinence-associated dermatitis, maceration, or excoriation (Fig. 48-4, B).
Stage III: Full-thickness Skin Loss (Fat Visible)
A stage III ulcer is a full-thickness tissue loss. Subcutaneous fat may be visible; but bone, tendon, or muscle is not exposed. Some slough may be present. It may include undermining and tunneling.
Further description: The depth of a stage III pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput, and malleolus do not have (adipose) subcutaneous tissue; and stage III ulcers can be shallow. In contrast, areas of significant adiposity can develop extremely deep stage III pressure ulcers. Bone/tendon is not visible or directly palpable (Fig. 48-4, C).
Stage IV: Full-thickness Tissue Loss (Muscle/Bone Visible)
A stage IV ulcer is a full-thickness tissue loss with exposed bone, tendon, or muscle. Slough or eschar may be present. It often includes undermining and tunneling.
Further description: The depth of a stage IV pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput, and malleolus do not have (adipose) subcutaneous tissue; and these ulcers can be shallow. Stage IV ulcers can extend into muscle and/or supporting structures (e.g., fascia, tendon, or joint capsule), making osteomyelitis or osteitis likely to occur. Exposed bone/muscle is visible or directly palpable (Fig. 48-4, D).
Unstageable/Unclassified: Full-thickness Skin or Tissue Loss—Depth Unknown
The EPUAP and the NPUAP (2009) developed a definition for an ulcer in which the base of the wound cannot be visualized and a definition of tissue injury in which the depth of injury is unknown. An unstageable ulcer is a full-thickness tissue loss in which actual depth of the ulcer is completely obscured by slough (yellow, tan, gray, green, or brown) and/or eschar (tan, brown, or black) in the wound bed (Fig. 48-4, E).
Further description: Until enough slough and/or eschar are removed to expose the base of the wound, the true depth cannot be determined; but it is either a stage III or IV. Stable (dry, adherent, intact without erythema or fluctuance) eschar on the heels serves as “the natural (biological) cover of the body” and should not be removed.
Suspected Deep-Tissue Injury—Depth Unknown
Suspected deep-tissue injury is a purple or maroon localized area of discolored intact skin or blood-filled blister caused by damage of underlying soft tissue from pressure and/or shear (Fig. 48-4, F).
Further description: The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer, or cooler than adjacent tissue. Deep-tissue injury may be difficult to detect in individuals with dark skin tones. Evolution may include a thin blister over a dark wound bed. The wound may further evolve and become covered by thin eschar. Evolution may be rapid, exposing additional layers of tissue even with treatment.
In addition, Bennett (1995) suggests that, when assessing patients with darkly pigmented skin, proper lighting is important to accurately assess the skin (see Box 48-2). Either natural light or a halogen light is recommended. This prevents the blue tones that fluorescent light sources produce on darkly pigmented skin, which interferes with accurate assessment. Additional aspects of assessing dark skin are in Box 48-3.
You need to assess the type of tissue in the wound base; this information is used to plan appropriate interventions. The assessment of tissue type includes the amount (percentage) and appearance (color) of viable and nonviable tissue. Granulation tissue is red, moist tissue composed of new blood vessels, the presence of which indicates progression toward healing. Soft yellow or white tissue is characteristic of slough (stringy substance attached to wound bed), and it must be removed by a skilled clinician before the wound is able to heal. Black or brown necrotic tissue is eschar, which also needs to be removed before healing can proceed.
The measurement of the size of the wound provides overall changes in size, which is an indicator for wound healing progress (Nix, 2012). Use disposable wound-measuring devices to obtain measurement of width and length. Select a uniform, consistent method for measuring wound length and width to facilitate meaningful comparisons of wound measurements across time (EPUAP and NPUAP, 2009). Measure depth by using a cotton-tipped applicator in the wound bed.
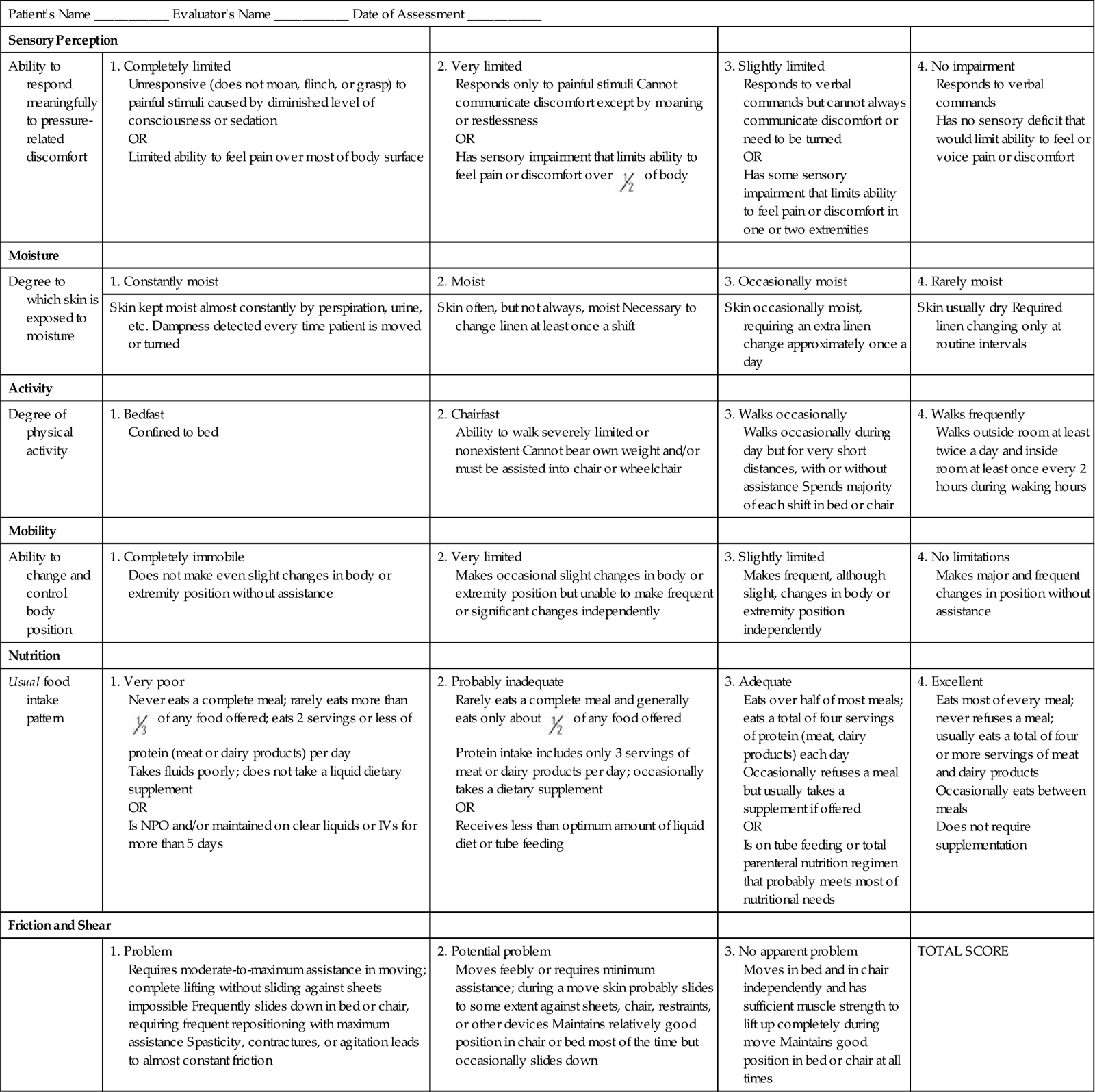
Wound exudate should describe the amount, color, consistency, and odor of wound drainage and is part of the wound assessment. Excessive exudate indicates the presence of infection. Finally, assess the condition of the skin surrounding the wound for redness, warmth, maceration, or edema (swelling). The presence of any of these factors on the skin surrounding the wound indicates wound deterioration.
The skin around the wound (periwound) should be assessed. Examine the periwound area for redness, warmth, and signs of maceration and palpate the area for signs of pain or induration.
Wound Classifications
A wound is a disruption of the integrity and function of tissues in the body (Baharestani, 2008). It is imperative for the nurse to know that all wounds are not created equal. Understanding the etiology of a wound is important because the treatment for it varies, depending on the underlying disease process.
There are many ways to classify wounds. Wound classification systems describe the status of skin integrity, cause of the wound, severity or extent of tissue injury or damage, cleanliness of the wound (Table 48-1), or descriptive qualities of the wound tissue such as color (Fig. 48-5). Wound classifications enable a nurse to understand the risks associated with a wound and implications for healing.
TABLE 48-1
| DESCRIPTION | CAUSES | IMPLICATIONS FOR HEALING |
| Onset and Duration | ||
| Acute | ||
| Wound that proceeds through an orderly and timely reparative process that results in sustained restoration of anatomical and functional integrity | Trauma, a surgical incision | Wounds are usually easily cleaned and repaired. Wound edges are clean and intact. |
| Chronic | ||
| Wound that fails to proceed through an orderly and timely process to produce anatomical and functional integrity | Vascular compromise, chronic inflammation, or repetitive insults to tissue (Doughty and Sparks-Defriese, 2012) | Continued exposure to insult impedes wound healing. |
| Healing Process | ||
| Primary Intention | ||
| Wound that is closed | Surgical incision, wound that is sutured or stapled | Healing occurs by epithelialization; heals quickly with minimal scar formation. |
| Secondary Intention | ||
| Wound edges not approximated | Pressure ulcers, surgical wounds that have tissue loss | Wound heals by granulation tissue formation, wound contraction, and epithelialization. |
| Tertiary Intention | ||
| Wound left open for several days, then wound edges are approximated (see Fig. 48-4,C) | Wounds that are contaminated and require observation for signs of inflammation | Closure of wound is delayed until risk of infection is resolved (Doughty and Sparks-Defriese, 2012). |
Process of Wound Healing
Wound healing involves integrated physiological processes. The tissue layers involved and their capacity for regeneration determine the mechanism for repair for any wound (Doughty and Sparks-Defriese, 2012).
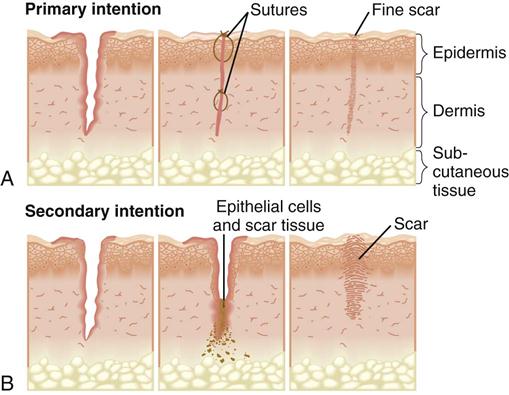
There are two types of wounds: those with loss of tissue and those without. A clean surgical incision is an example of a wound with little tissue loss. The surgical incision heals by primary intention (Fig. 48-6, A). The skin edges are approximated, or closed, and the risk of infection is low. Healing occurs quickly, with minimal scar formation, as long as infection and secondary breakdown are prevented (Doughty and Sparks-Defriese, 2012). In contrast, a wound involving loss of tissue such as a burn, pressure ulcer, or severe laceration heals by secondary intention. The wound is left open until it becomes filled by scar tissue. It takes longer for a wound to heal by secondary intention; thus the chance of infection is greater. If scarring from secondary intention is severe, loss of tissue function is often permanent (Fig. 48-6, B).
Wound Repair
Partial-thickness wounds are shallow wounds involving loss of the epidermis (top layer) and possibly partial loss of the dermis. These wounds heal by regeneration because epidermis regenerates. An example of this is the repair of a clean surgical wound or an abrasion. Full-thickness wounds extending into the dermis (involving both layers of tissue) heal by scar formation because deeper structures do not regenerate. Pressure ulcers are an example of full-thickness wounds.
Partial-Thickness Wound Repair
Three components are involved in the healing process of a partial-thickness wound: inflammatory response, epithelial proliferation (reproduction) and migration, and reestablishment of the epidermal layers.
Tissue trauma causes the inflammatory response, which in turn causes redness and swelling to the area with a moderate amount of serous exudate. This response is generally limited to the first 24 hours after wounding. The epithelial cells begin to regenerate, providing new cells to replace the lost cells. The epithelial proliferation and migration start at both the wound edges and the epidermal cells lining the epidermal appendages, allowing for quick resurfacing. Epithelial cells begin to migrate across the wound bed soon after the wound occurs. A wound left open to air can resurface within 6 to 7 days, whereas one that is kept moist can resurface in 4 days. The difference in the healing rate is related to the fact that epidermal cells only migrate across a moist surface. In a dry wound the cells migrate down into a moist level before migration can occur (Doughty and Sparks-Defriese, 2012). New epithelium is only a few cells thick and must undergo reestablishment of the epidermal layers. The cells slowly reestablish normal thickness and appear as dry, pink tissue.
Full-Thickness Wound Repair
The four phases involved in the healing process of a full-thickness wound are hemostasis, inflammatory, proliferative, and remodeling.
Hemostasis
A series of events designed to control blood loss, establish bacterial control, and seal the defect occurs when there is an injury. During hemostasis injured blood vessels constrict, and platelets gather to stop bleeding. Clots form a fibrin matrix that later provides a framework for cellular repair.
Inflammatory Phase
In the inflammatory stage damaged tissue and mast cells secrete histamine, resulting in vasodilation of surrounding capillaries and exudation of serum and white blood cells into damaged tissues. This results in localized redness, edema, warmth, and throbbing. The inflammatory response is beneficial, and there is no value in attempting to cool the area or reduce the swelling unless the swelling occurs within a closed compartment (e.g., ankle or neck).
Leukocytes (white blood cells) reach the wound within a few hours. The primary-acting white blood cell is the neutrophil, which begins to ingest bacteria and small debris. The second important leukocyte is the monocyte, which transforms into macrophages. The macrophages are the “garbage cells” that clean a wound of bacteria, dead cells, and debris by phagocytosis. Macrophages continue the process of clearing the wound of debris and release growth factors that attract fibroblasts, the cells that synthesize collagen (connective tissue). Collagen appears as early as the second day and is the main component of scar tissue.
In a clean wound the inflammatory phase establishes a clean wound bed. The inflammatory phase is prolonged if too little inflammation occurs, as in a debilitating disease such as cancer or after administration of steroids. Too much inflammation also prolongs healing because arriving cells compete for available nutrients. An example is a wound infection in which the increased metabolic energy requirements present in an infected wound compete for the available calorie intake.
Proliferative Phase
With the appearance of new blood vessels as reconstruction progresses, the proliferative phase begins and lasts from 3 to 24 days. The main activities during this phase are the filling of the wound with granulation tissue, contraction of the wound, and the resurfacing of the wound by epithelialization. Fibroblasts are present in this phase and are the cells that synthesize collagen, providing the matrix for granulation. Collagen mixes with the granulation tissue, and this matrix supports the reepithelialization. Collagen provides strength and structural integrity to a wound. During this period the wound contracts to reduce the area that requires healing. Finally the epithelial cells migrate from the wound edges to resurface. In a clean wound the proliferative phase accomplishes the following: the vascular bed is reestablished (granulation tissue), the area is filled with replacement tissue (collagen, contraction, and granulation tissue), and the surface is repaired (epithelialization). Impairment of healing during this stage usually results from systemic factors such as age, anemia, hypoproteinemia, and zinc deficiency.
Remodeling
Maturation, the final stage of healing, sometimes takes place for more than a year, depending on the depth and extent of the wound. The collagen scar continues to reorganize and gain strength for several months. However, a healed wound usually does not have the tensile strength of the tissue it replaces. Collagen fibers undergo remodeling or reorganization before assuming their normal appearance. Usually scar tissue contains fewer pigmented cells (melanocytes) and has a lighter color than normal skin. In dark-skinned individuals the scar tissue may be more highly pigmented than surrounding skin.
Complications of Wound Healing
Hemorrhage
Hemorrhage, or bleeding from a wound site, is normal during and immediately after initial trauma. Hemostasis occurs within several minutes unless large blood vessels are involved or the patient has poor clotting function. Hemorrhage occurring after hemostasis indicates a slipped surgical suture, a dislodged clot, infection, or erosion of a blood vessel by a foreign object (e.g., a drain). Hemorrhage occurs externally or internally. For example, if a surgical suture slips from a blood vessel, bleeding occurs internally within the tissues, and there are no visible signs of blood unless a surgical drain is present. A surgical drain may be inserted into tissues beneath a wound to remove fluid that collects in underlying tissues.
You detect internal bleeding by looking for distention or swelling of the affected body part, a change in the type and amount of drainage from a surgical drain, or signs of hypovolemic shock. A hematoma is a localized collection of blood underneath the tissues. It appears as a swelling, change in color, sensation, or warmth or mass that often takes on a bluish discoloration. A hematoma near a major artery or vein is dangerous because pressure from the expanding hematoma obstructs blood flow.
External hemorrhaging is obvious. The nurse observes dressings covering the wound for bloody drainage. If bleeding is extensive, the dressing soon becomes saturated, and frequently blood drains from under the dressing and pools beneath the patient. Observe all wounds closely, particularly surgical wounds, in which the risk of hemorrhage is great during the first 24 to 48 hours after surgery or injury.
Infection
Wound infection is the second most common health care–associated infection (nosocomial) (see Chapter 28). According to the Centers for Disease Control and Prevention (CDC) (2001), a wound is infected if purulent material drains from it, even if a culture is not taken or has negative results. A sample of drainage from an infected wound does not always reveal bacteria because of poor culture technique or administration of antibiotics. Positive culture findings do not always indicate an infection because many wounds contain colonies of noninfective resident bacteria. In fact, all chronic dermal wounds are considered contaminated with bacteria. What differentiates contaminated wounds from infected wounds is the amount of bacteria present. It is generally agreed that wounds with more than 100,000 (105) organisms per gram of tissue are infected (Stotts, 2012b). The chances of wound infection are greater when the wound contains dead or necrotic tissue, there are foreign bodies in or near the wound, and the blood supply and local tissue defenses are reduced. Bacterial wound infection inhibits wound healing.
Some contaminated or traumatic wounds show signs of infection early, within 2 to 3 days. A surgical wound infection usually does not develop until the fourth or fifth postoperative day. The patient has a fever, tenderness and pain at the wound site, and an elevated white blood cell count. The edges of the wound appear inflamed. If drainage is present, it is odorous and purulent, which causes a yellow, green, or brown color, depending on the causative organism (Table 48-2).
TABLE 48-2
| TYPE | APPEARANCE |
| Serous | Clear, watery plasma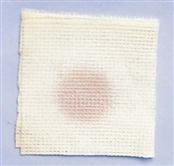 |
| Purulent | Thick, yellow, green, tan, or brown |
| Serosanguineous | Pale, pink, watery; mixture of clear and red fluid |
| Sanguineous | Bright red; indicates active bleeding |
Dehiscence
When a wound fails to heal properly, the layers of skin and tissue separate. This most commonly occurs before collagen formation (3 to 11 days after injury). Dehiscence is the partial or total separation of wound layers. A patient who is at risk for poor wound healing (e.g., poor nutritional status, infection, or obesity) is at risk for dehiscence. However, obese patients have a higher risk because of the constant strain placed on their wounds and the poor healing qualities of fat tissue (Camden, 2012). Dehiscence frequently involves abdominal surgical wounds and occurs after a sudden strain such as coughing, vomiting, or sitting up in bed. Patients often report feeling as though something has given way. When there is an increase in serosanguineous drainage from a wound, be alert for the potential for dehiscence. A strategy to prevent dehiscence is to place a folded thin blanket or pillow over an abdominal wound when the patient is coughing. This provides a splint to the area, supporting the healing tissue when coughing increases the intraabdominal pressure.
Evisceration
With total separation of wound layers, evisceration (protrusion of visceral organs through a wound opening) occurs. The condition is an emergency that requires surgical repair. When evisceration occurs, the nurse places sterile towels soaked in sterile saline over the extruding tissues to reduce chances of bacterial invasion and drying of the tissues. If the organs protrude through the wound, blood supply to the tissues is compromised. The presence of an evisceration is a surgical emergency. Immediately contact the surgical team, do not allow the patient anything by mouth (NPO), observe him or her for signs and symptoms of shock, and prepare him or her for emergency surgery.
Nursing Knowledge Base
Prediction and Prevention of Pressure Ulcers
A major aspect of nursing care is the maintenance of skin integrity. Consistent, planned skin care interventions are critical to ensuring high-quality care. Nurses constantly observe their patients’ skin for breaks or impaired skin integrity. Impaired skin integrity occurs from prolonged pressure, irritation of the skin, and/or immobility, leading to the development of pressure ulcers. A pressure ulcer is a localized injury to the skin and/or underlying tissue, usually over a bony prominence, as a result of pressure or pressure in combination with shear and/or friction (EPUAP and NPUAP, 2009).
Risk Assessment
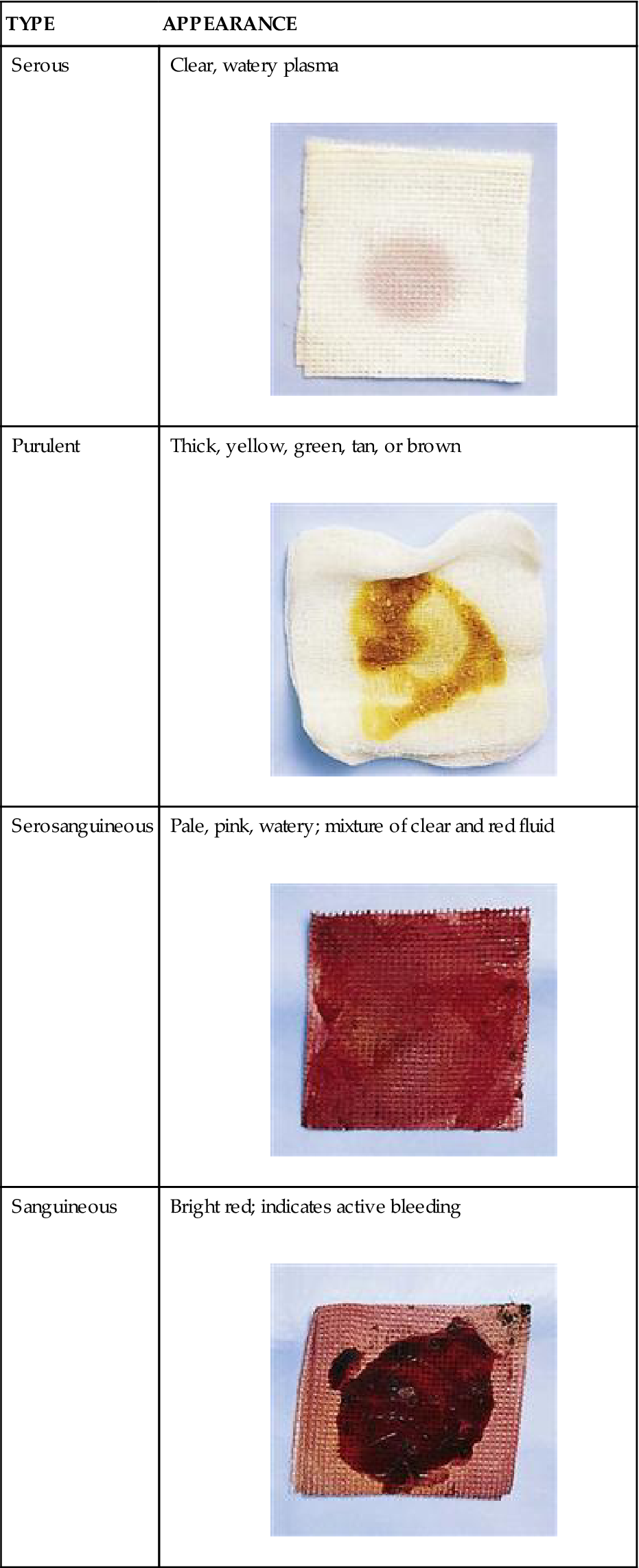
Several instruments are available for assessing patients who are at risk for developing a pressure ulcer. By identifying at-risk patients, you are able to put interventions into place for the at-risk patient and spare patients with little risk for pressure ulcer development the unnecessary and sometimes costly preventive treatment. Prevention and treatment of pressure ulcers are major nursing priorities. The incidence of pressure ulcers in a facility or agency is an important indicator of quality of care. Evidence exists that a program of prevention guided by risk assessment simultaneously reduces the institutional incidence of pressure ulcers by as much as 60% and brings down the costs of prevention at the same time (Braden, 2001). Several risk-assessment scales (Bergstrom et al., 1987; Norton et al., 1962) developed by nurses enable systematic risk assessment of patients. The Braden Scale, a widely used risk-assessment tool, is in the WOCN guidelines (2010) as being a valid tool to use for pressure ulcer risk assessment. The Braden Scale (Table 48-3) was developed based on risk factors in a nursing home population (Bergstrom et al., 1987) and is composed of six subscales: sensory perception, moisture, activity, mobility, nutrition, and friction/shear. The total score ranges from 6 to 23; a lower total score indicates a higher risk for pressure ulcer development (Braden and Bergstrom, 1989). The cutoff score for onset of pressure ulcer risk with the Braden Scale in the general adult population is 18 (Ayello and Braden, 2002). It is highly reliable when used to identify patients at greatest risk for pressure ulcers (Bergstrom et al., 1987; Braden and Bergstrom, 1994). The Braden Scale is the most commonly used assessment scale for pressure ulcer risk.
TABLE 48-3
Braden Scale for Predicting Pressure Ulcer Risk
| Patient’s Name ___________ Evaluator’s Name ___________ Date of Assessment ___________ | ||||
| Sensory Perception | ||||
| Ability to respond meaningfully to pressure-related discomfort | 1. Completely limited Unresponsive (does not moan, flinch, or grasp) to painful stimuli caused by diminished level of consciousness or sedation OR Limited ability to feel pain over most of body surface | 2. Very limited Responds only to painful stimuli Cannot communicate discomfort except by moaning or restlessness OR Has sensory impairment that limits ability to feel pain or discomfort over  of body of body | 3. Slightly limited Responds to verbal commands but cannot always communicate discomfort or need to be turned OR Has some sensory impairment that limits ability to feel pain or discomfort in one or two extremities | 4. No impairment Responds to verbal commands Has no sensory deficit that would limit ability to feel or voice pain or discomfort |
| Moisture | ||||
| Degree to which skin is exposed to moisture | 1. Constantly moist | 2. Moist | 3. Occasionally moist | 4. Rarely moist |
| Skin kept moist almost constantly by perspiration, urine, etc. Dampness detected every time patient is moved or turned | Skin often, but not always, moist Necessary to change linen at least once a shift | Skin occasionally moist, requiring an extra linen change approximately once a day | Skin usually dry Required linen changing only at routine intervals | |
| Activity | ||||
| Degree of physical activity | 1. Bedfast Confined to bed | 2. Chairfast Ability to walk severely limited or nonexistent Cannot bear own weight and/or must be assisted into chair or wheelchair | 3. Walks occasionally Walks occasionally during day but for very short distances, with or without assistance Spends majority of each shift in bed or chair | 4. Walks frequently Walks outside room at least twice a day and inside room at least once every 2 hours during waking hours |
| Mobility | ||||
| Ability to change and control body position | 1. Completely immobile Does not make even slight changes in body or extremity position without assistance | 2. Very limited Makes occasional slight changes in body or extremity position but unable to make frequent or significant changes independently | 3. Slightly limited Makes frequent, although slight, changes in body or extremity position independently | 4. No limitations Makes major and frequent changes in position without assistance |
| Nutrition | ||||
| Usual food intake pattern | 1. Very poor Never eats a complete meal; rarely eats more than  of any food offered; eats 2 servings or less of protein (meat or dairy products) per day of any food offered; eats 2 servings or less of protein (meat or dairy products) per dayTakes fluids poorly; does not take a liquid dietary supplement OR Is NPO and/or maintained on clear liquids or IVs for more than 5 days | 2. Probably inadequate Rarely eats a complete meal and generally eats only about  of any food offered Protein intake includes only 3 servings of meat or dairy products per day; occasionally takes a dietary supplement of any food offered Protein intake includes only 3 servings of meat or dairy products per day; occasionally takes a dietary supplementOR Receives less than optimum amount of liquid diet or tube feeding | 3. Adequate Eats over half of most meals; eats a total of four servings of protein (meat, dairy products) each day Occasionally refuses a meal but usually takes a supplement if offered OR Is on tube feeding or total parenteral nutrition regimen that probably meets most of nutritional needs | 4. Excellent Eats most of every meal; never refuses a meal; usually eats a total of four or more servings of meat and dairy products Occasionally eats between meals Does not require supplementation |
| Friction and Shear | ||||
| 1. Problem Requires moderate-to-maximum assistance in moving; complete lifting without sliding against sheets impossible Frequently slides down in bed or chair, requiring frequent repositioning with maximum assistance Spasticity, contractures, or agitation leads to almost constant friction | 2. Potential problem Moves feebly or requires minimum assistance; during a move skin probably slides to some extent against sheets, chair, restraints, or other devices Maintains relatively good position in chair or bed most of the time but occasionally slides down | 3. No apparent problem Moves in bed and in chair independently and has sufficient muscle strength to lift up completely during move Maintains good position in bed or chair at all times | TOTAL SCORE | |
Copyright 1988. Used with permission of Barbara Braden, PhD, RN, Professor, Creighton University School of Nursing, Omaha, Nebraska, and Nancy Bergstrom, Professor, University of Texas-Houston, School of Nursing, Houston, Texas, http://www.bradenscale.com.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree