Chapter 27. Respiratory illness in children
Janet Kelsey and Gill McEwing
LEARNING OUTCOMES
• Demonstrate an understanding of the anatomy and physiology of the respiratory tract.
• Gain an overview of the nature of respiratory illness in children.
• Appreciate the role of the nurse in caring for children with respiratory illness.
• Identify the signs of respiratory distress.
• Use relevant literature and research to inform the nursing care of children with respiratory illness.
Introduction
The most common illnesses in infants and children in the UK are disorders of the respiratory system. Respiratory tract infections in children, although common, are not usually serious. Frequent infections occur in children because the immune system has not been exposed to common pathogens and therefore infections tend to develop with each new exposure. The risk of infection is also increased in children because the respiratory tract is relatively short. Most of these infections do not cause a serious problem to the child; however children are particularly vulnerable to respiratory problems because of their relatively high oxygen requirements and the immaturity of their respiratory system (Carter 1995). Respiratory disease in early childhood can interfere with the development of the lungs and cause permanent lung damage. Acute respiratory failure can result from any airway, pulmonary or neuromuscular disease that impairs oxygen exchange or elimination of carbon dioxide.
Some respiratory problems are more common at specific ages. The same organism can cause different illnesses at different ages. For example, the respiratory syncytial virus (RSV) frequently causes bronchiolitis in infants but causes only a sore throat and cold symptoms in older children (Meadow & Newell 2002).
The majority of infections (80%) are restricted to the upper respiratory tract and approximately 20% of these will become severe and require medical intervention. These include conditions such as bronchiolitis, laryngotracheobronchitis, epiglottitus, pneumonia and acute asthma (Morton & Phillips 1992, Thompson 1990). These are major causes of morbidity in children and a common reason for admission to hospital (Meadow & Newell 2002).
Respiratory illness accounts for 30–40% of acute medical admissions to hospital of children and over 450 deaths in England and Wales each year. The Child Health Committee (1997) reported that the principal cause for admission to hospital (30.9%) of children aged 0–4 years in England between 1993 and 1994 was a respiratory problem.
Anatomy and physiology of the respiratory tract
The human body requires a constant supply of oxygen. Children have a higher metabolic rate than adults, and thus an increased need for oxygen, which demands that their respiratory system functions effectively. The respiratory system consists of the lungs, the airways, the chest wall and the pulmonary circulation. The lungs (Fig. 27.1) are situated in the thorax, the sides of the thorax are bounded by the rib cage; linking the ribs are the intercostal muscles. At the base of the thorax is a flexible sheet of muscle known as the diaphragm.
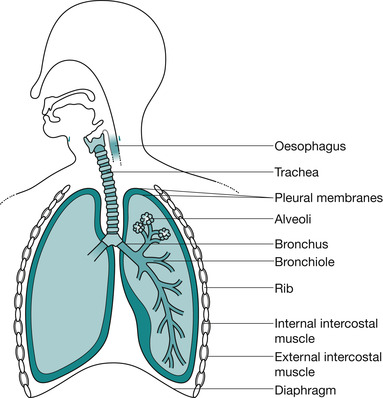 |
| Fig. 27.1 Basic structure of the lungs. |
The primary function of the respiratory system is the exchange of gases between the environmental air and the blood. There are three steps in this process: the movement of air in and out of the lungs, the movement of gases between air spaces in the lungs and the blood, and the movement of blood from the capillaries surrounding the lungs to the body’s organs and tissues. The first two processes are functions of the respiratory system, the third is performed by the cardiovascular system (McChance & Heuther 2002).
The respiratory system can be divided into the upper and lower airways. The upper airways consist of the nasopharynx and the oropharynx. These structures are lined with highly vascular, ciliated epithelium. This warms and moistens the inspired air and removes foreign particles from it as it passes into the lungs. During quiet respiration, air passes through the nose, nasopharynx and oropharynx to the lower airways. During exercise or when the nose is obstructed the mouth and oropharynx are used for ventilation, however by this route the air is not filtered or humidified as efficiently as via the nasopharynx. The larynx connects the upper and lower airways; it is a cartilaginous structure that prevents collapse of the airways during inspiration. Air then flows into the trachea, which is supported by U-shaped cartilage. The trachea divides into the two main bronchi, which in turn divide into bronchioles; there are 16 divisions in total, ending in the terminal bronchioles. This multiple subdivision causes a decrease in the velocity of the air flow into the lungs, which allows for maximum gaseous exchange to take place. The bronchioles have cartilage within their walls until the tenth division. The terminal bronchioles continue to divide into smaller respiratory bronchioles, and then into the alveolar ducts. These lead to the alveolar sacs, which are made up of numerous alveoli. The alveoli (Fig. 27.2) are the primary gas-exchange units of the lungs; it is here that oxygen enters the blood and carbon dioxide is removed (McChance & Heuther 2002).
 PowerPoint
PowerPoint
 PowerPoint
PowerPointAccess the companion PowerPoint presentation.
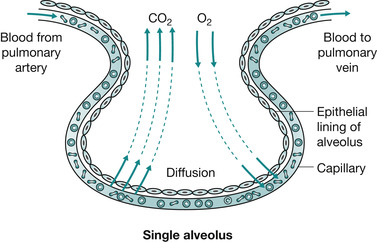 |
| Fig. 27.2 A single alveolus. |
There are 20 million alveoli at birth, increasing to 300 million alveoli in the fully formed lungs of the adult (Meadow & Newell 2002). This means that infants and young children have a relatively small alveolar surface area for gaseous exchange. Each alveolus has a network of capillaries wrapped around it. The walls of the alveoli and the capillaries are only one cell thick. A thin layer of liquid covers their surface, which aids gaseous exchange between the inhaled air and the circulating blood.
Inhalation involves the diaphragm contracting and flattening and the external intercostal muscles contracting, pulling the ribcage upwards and outwards. This increases the volume inside the thorax, decreases the pressure inside the lungs, and air is sucked in. When the diaphragm relaxes it domes up into the thorax and, as the external intercostal muscles relax, the rib cage drops down and moves inwards. This increases the pressure inside the lungs and forces air out. The internal intercostal muscles contract during strenuous breathing to pull the rib cage down to produce a forced expiration. There are two main considerations in infants and children. First, in the newborn, the diaphragm is not able to contract as effectively as in an older infant or child because it is attached higher at the front and is therefore longer. Second, infants and children have a relatively round thoracic cavity due to the horizontal position of the ribs, this places increased dependence on the diaphragm and abdomen as the primary means of ventilation.
 PowerPoint
PowerPoint
 www
www
 PowerPoint
PowerPointAccess the companion PowerPoint presentation.
 www
wwwSee respiratory movements online at:
Lung volumes
The total capacity of a child’s lungs increases from 1.4 L in the 5-year-old child to 4.5 L at the time of puberty (MacGregor 2000):
• At the end of quiet respiration, the air that remains in the lungs is termed the functional residual capacity.
• Following forced expiration, between 0.5 and 1.5 L (depending on age) of air remains trapped in the alveoli; this minimal volume is called the residual volume.
• The additional volume of air forced out of the lungs during a forced expiration of between 0.5 and 1.5 L is known as the expiratory reserve volume.
• During quiet respiration, the amount of air in the lungs increases from 0.7 L at 5 years (or 2.25 L at puberty) at the end of expiration to 0.8 L at 5 years (or 2.55 L at puberty) at the end of inspiration; this 0.1 L (0.3 L at puberty) of air moving in and out of the lungs is called the tidal volume.
• The vital capacity of the lungs is the amount of air moving when the patient is performing forced inspiration and forced expiration, which will be the sum of the inspiratory reserve volume, the expiratory reserve volume and the tidal volume. This volume is related to the size of the patient; at age 5 years it is approximately 1 L and this increases to 3 L at puberty (MacGregor 2000). The vital capacity can be increased if the patient stands up because the volume of blood in the lungs is reduced.
• The peak flow is the maximum velocity of air flow produced in a forced respiration. When this value is low it suggests that expiratory respiratory muscle activity is weak or that there is an obstruction to expiratory air flow due to some form of bronchoconstriction such as asthma.
Nervous control of breathing
The respiratory centre is situated at the base of the brain and is made up of the medulla oblongata and the pons. The control of breathing has both automatic and voluntary components. Voluntary control allows for breathing to be integrated with voluntary actions such as blowing, singing and speaking. Automatic control involves input from two types of receptors; those that monitor the pH, carbon dioxide and oxygen levels in the blood, and those that monitor breathing patterns and lung function.
Chemoreceptors assess the level of carbon dioxide and oxygen in the blood, messages are transmitted to the respiratory centre and ventilation is adjusted to maintain arterial blood gases within a normal range (Table 27.1). How much oxygen is in the blood depends on the:
• haemoglobin concentration in the blood (Hb g/dL)
• oxygen saturation of the haemoglobin (SaO 2)
• partial pressure of oxygen (PaO 2).
| pH | 7.32–7.42 | 7.35–7.45 |
|---|---|---|
| PaCO 2 | 30–40 mm Hg | 35–45 mmHg |
| HCO 3 | 20–26 mEq/L | 22–28 mEq/L |
| PaO 2 | 60–80 mmHg | 80–100 mmHg |
The central chemoreceptors located in the medulla oblongata monitor the carbon dioxide level in the blood by assessing the number of free hydrogen ions in the cerebrospinal fluid circulating around the medulla. This is important because the carbon dioxide level in the blood affects the pH level of the extracellular fluid of the brain. These receptors are extremely sensitive in the short term but long-term elevation of carbon dioxide levels, such as can occur in chronic respiratory disease, causes desensitisation of these receptors.
The carotid and aortic bodies are chemoreceptors that are sensitive to oxygen levels in the carotid artery and aorta, respectively. They are less responsive than the central chemoreceptors and are activated only when the oxygen level falls below 60 mmHg. Therefore hypoxia is the main stimulus for ventilation in persons with chronic hypercarbia (Porth 1994).
 Reflect on your practice
Reflect on your practice
 PowerPoint
PowerPoint
 Reflect on your practice
Reflect on your practiceHow would you explain to a junior nurse the importance of the correct level of oxygen administration when assisting a child with a chronic respiratory condition experiencing an acute respiratory illness?
 PowerPoint
PowerPointAccess the companion PowerPoint presentation.
The anatomy and physiology of the respiratory and cardiovascular systems of children differs from that of adults. This influences the care given to children and hence must be considered when assessing and managing children with respiratory problems.
It is important to remember that anatomical differences influence the degree to which children respond to respiratory illness because of the smaller diameter of the airways (Fig. 27.3 and Table 27.2). Poiseuille’s law states that:


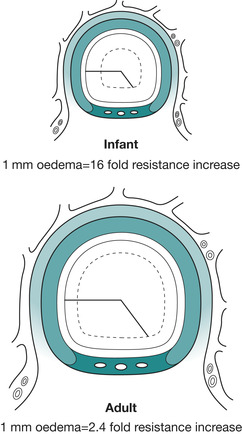 |
| Fig. 27.3 Anatomical differences between the airways of an infant and of an adult. |
| Factor | Nursing considerations |
|---|---|
| Airway | |
| Large head, short neck, inability to support head | Assistance required to maintain position of comfort |
| Large tongue | Airway is easily obstructed by tongue; proper positioning is often all that is necessary to open the airway |
| The floor of the mouth is easily compressible | Care is required when positioning of the fingers when holding the jaw |
| Infants less than 6 months old are obligate nose breathers | Obstruction of the nasal passages by mucus can compromise the infant’s airway |
| Smaller diameter of all airways in a 1-year-old child. Tracheal diameter is less than the child’s little finger | Small amounts of mucous or swelling easily obstruct the airways; child normally has increased airway resistance |
| The epiglottis is horseshoe shaped and projects posteriorly at 45%. The larynx is high and anterior | Tracheal intubation can be more difficult. A straight blade laryngoscope is used, cricoid pressure may be necessary to facilitate intubation |
| The trachea is short and soft. The cricoid cartilage is the narrowest portion of neck | Airway of infant can be compressed if neck is flexed or hyperextended. Tube displacement is more likely. Provides a natural seal for endotracheal tube |
| The cricoid ring is lined by pseudostratifed ciliated epithelium loosely bound to areolar tissue | Particularly susceptible to oedema. Uncuffed tubes are preferred in pre-pubertal children |
| Breathing | |
| Infants rely mainly on diaphragmatic breathing. The ribs lie more horizontally in infants and contribute less to chest expansion. Their muscles are more likely to fatigue compared with adults | Children are more prone to respiratory failure. Anything that impedes diaphragm contraction or movement, e.g. abdominal distension can contribute to the development of respiratory failure |
| Sternum and ribs are cartilaginous; chest wall is soft; intercostal muscles are poorly developed | Infant’s chest wall may move inwards instead of outwards during inspiration (retractions) when lung compliance is decreased; greater intrathoracic pressure is generated during inspiration. The compliant chest wall may allow serious parenchymal injuries to occur without rib fracture |
| Increased metabolic rate (about twice that of an adult); increased respiratory demand for oxygen consumption and carbon dioxide elimination | Respiratory distress increases oxygen demand, as does any condition that increases metabolic rate, e.g. fever |
| Lung compliance and high chest wall compliance in the neonate | Respiratory function inefficient during episodes of respiratory distress |
| Smaller amount of elastic and collagen tissue in the paediatric lung | May contribute to the increased incidence of pulmonary oedema, pneumomediastinum and pneumothorax in infants |
| Circulation | |
Child’s circulating blood volume is larger per unit of body weight (70–80 mL/kg) but absolute volume is relatively small; 70–80% of newborn’s body weight is water, compared with 50–60% of an adult body weight; about half of this volume is extracellular Stroke volume is small and relatively fixed in infants. Cardiac output is directly related to heart rate | Blood loss considered minor in an adult may lead to shock in a child; decreased fluid intake or increased fluid loss quickly leads to dehydration Acute blood loss produces symptoms when 20–25% of circulating volume has been lost Dehydration will compromise peripheral perfusion when 7–10% of the infant or child’s body weight and 5–7% of the adolescent or adult body weight is lost Stroke volume cannot increase to improve cardiac output. Response to volume therapy is therefore blunted |
| By the age of 2 years the myocardial function and response to fluid is similar to that of an adult | Tachycardia is the child’s most efficient method of increasing cardiac output. However ventricular rates of > 180–220 beats/min compromise diastolic filling time and coronary artery perfusion |
| Systemic vascular resistance rises after birth and continues to do so until adulthood | Children’s normal values for blood pressure increase with age |
That is, resistance to airflow is inversely proportional to the fourth power of the radius. In other words, a small amount of mucous or oedema in the airways will significantly increase resistance to airflow and therefore increase the work of breathing.
Respiratory assessment and examination of the chest
A calm manner should always be adopted when assessing any child with respiratory problems. The ‘hands-off approach’ can generate a lot of useful information gained through careful observation and this is particularly useful in very young children, who may resist physical examination. It is always important to leave the child with his or her carer in an upright position. Although observations focus on the respiratory status of the child, it is important to note the child’s general appearance, level of engagement with carer, colour, hydration status and temperature. In addition, the ability of infants to feed should be noted. If at any time you feel the child needs immediate intervention, for example they are having difficulties breathing, then the assessment should be stopped and emergency care given to stabilise the child.
Assessment follows the ABC criteria for assessment in conjunction with neurological observations and provides a framework for rapid and effective nursing assessment of the child with respiratory problems. The survey should therefore include assessment of the following:
A. Airway
Patency of the airway is assessed, observing for spontaneous ventilation, and look, listen and feel. Note any presence of inspiratory noises. If the child is able to speak or is crying this indicates that the airway is patent. If there is no evidence of air movement then chin-lift or jaw-thrust should be carried out and the basic life support algorithm commenced.
B. Breathing
To assess the adequacy of breathing the chest should be examined and the following assessed:
• The effort of breathing including respiratory rate, recession, grunting, use of accessory muscles and nasal flaring.
• The efficacy of breathing including breath sounds and chest expansion/abdominal excursion.
• The effects of inadequate respiration including heart rate, oxygen saturation, skin colour and mental status.
Assessment of breathing therefore involves examination of the chest for the following:
• Respiratory movements
• Number rhythm, depth and quality of respirations
• Character of breath sounds utilising the skills of palpation, auscultation and percussion.
Chest wall movement should be symmetric bilaterally and coordinated with breathing.
On inspiration, the chest rises and expands (Fig. 27.4 A); on expiration, the chest descends and decreases in size (Fig. 27.4 B). In children less than 6–7 years of age, respiratory movement will be mainly abdominal or diaphragmatic; in older children respirations are mainly thoracic.
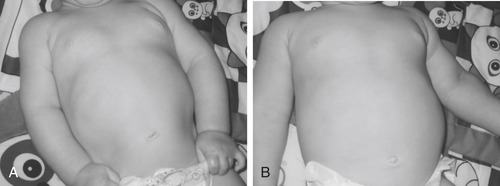 |
| Fig. 27.4 Chest expansion. |
To observe for chest expansion, stand at the child’s head or feet and, looking down the midline, note any asymmetry of movement. Decreased movement on one side may be the result of foreign body obstruction, pneumonia, pneumothorax or atelectasis.
Respiratory movements can be felt by placing each hand flat against the chest or back with thumbs in the midline along the lower costal margin (Fig. 27.5). The hands move with the chest wall during respiration. The amount of respiratory excursion is evaluated and asymmetry is noted.
 PowerPoint
PowerPoint
 PowerPoint
PowerPointAccess the companion PowerPoint presentation.
 |
| Fig. 27.5 Respiratory movements. |
Palpation is carried out for voice conduction (vocal fremitus). Place the palmar surface of the hand on the child’s chest and feel for vibrations as the child speaks. At the same time, move the hand symmetrically on either side of the sternum and vertebral column. Vocal fremitus is usually most prominent at the apex and least prominent at the base of the lungs. Absent or diminished vocal fremitus in the upper airway may indicate asthma or foreign body obstruction. Increased vocal fremitus may indicate pneumonia or atelectasis.
During palpation other abnormal vibrations that indicate pathological conditions are noted. These include pleural rub, which is felt as a grating sensation and is synchronous with respiration and crepitation, which can be felt as a coarse crackly sensation and is the result of air escaping from the lungs to the subcutaneous tissue. This may be caused by injury or surgical intervention. Both crepitation and pleural rub can often be heard as well as felt.
The sinking-in of soft tissues relative to the cartilaginous and bony thorax may be noted in some respiratory disorders. This is recession, it is described as intercostal, subcostal, substernal, clavicular and suprasternal and it demonstrates increased work of breathing:
• Intercostal, subcostal or sternal recession show increased work of breathing.
• Recession is more easily seen in younger children whose chest wall is more compliant.
• In children over 6 or 7 years, recession suggests severe respiratory problems.
• The degree of recession gives an indication of the severity of the breathing difficulty.
Nasal flaring is also an indication of increased work of breathing. The enlargement of the nostrils helps to reduce nasal resistance and maintain airway patency; it is usually described as either minimal or marked. Head bobbing in the infant is a sign of dyspnoea.
Respiratory rates should be measured over a full minute (Table 27.3). It should be remembered that young children breathe diaphragmatically and therefore are observed by watching abdominal movement rather than the movement of the chest. A decreasing rate or rhythm may indicate deterioration rather than improvement in the child’s condition (Mackway-Jones et al 1997). A resting rate of >60 breaths/minute is a sign of respiratory distress in a child irrespective of age (Cosby 1998 cited by Dolan & Holt 2000). Tachypnoea at rest indicates a need for increased ventilation.
| Age (years) | Breaths/min |
|---|---|
| <1 | 30–40 |
| 2–5 | 20–30 |
| 5–12 | 15–20 |
| >12 | 12–16 |
Respiratory rate
Further information about the severity of the child’s illness may be gained by measurement of oxygen saturation (SaO 2) levels with a pulse oximeter (Fig. 27.6). A saturation of less than 92% while breathing air, or less than 95% when breathing oxygen, is low. Rajesh et al (2000) evaluated respiratory rate as an indicator of hypoxia in infants <2 months of age and concluded that a respiratory rate of >60/minute is a good predictor of hypoxia and that the infants should be treated with oxygen should the facility to measure SaO 2 not be available. It should be remembered that pulse oximetry is less accurate when the SaO 2 is less than 70%, when shock is present, and in the presence of carboxyhaemoglobin. If there is evidence of respiratory or circulatory failure then arterial blood gases are needed.
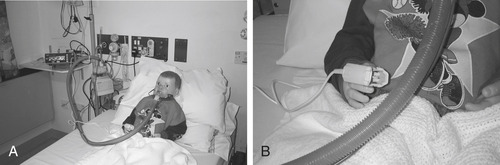 |
| Fig. 27.6 Measurement of oxygen saturation levels. |
The effectiveness of breathing is also assessed by observing breath sounds. Auscultation allows assessment of breath sounds for pitch, intensity, quality, location and duration. Breath sounds are best heard if the child inspires deeply. Normal breath sounds are vesicular, soft and low pitched on inspiration followed by shorter sound on expiration; bronchial or tubular are similar to the sounds heard upon auscultation over the larynx during respiration; and bronchovesicular is a mixture of bronchial and vesicular sounds. Vesicular are heard over most of the chest, except over the larynx and trachea, and, in infants, over the upper chest. Infants’ breath sounds are bronchovesicular in the upper chest because of increased transmission (Thompson 1990). Fluid, air or solid masses in the pleural space all interfere with the conduction of breath sounds.
Consolidation or solidification of a portion of the lung caused by, for example, pneumonia will result in tubular or bronchial breathing being heard over the posterior chest due to increased transmission between the trachea and the periphery of the chest (Thompson 1990).
Alert, diminished or absent breath sounds are always abnormal.
Percussion or tapping of the lungs (Fig. 27.7) is carried out to determine the presence and location of air, liquid and solid material in the lung and to evaluate the densities, position and landmarks of the underlying organs. Normally, the percussion note in a lung full of air is resonant. When there is fluid in the chest, e.g. pleural effusion, the note becomes flat. With pneumonia where there is an increased amount of fluid but not in the chest the note becomes dull. With excess air, e.g. asthma, the note is hyper-resonant. It is normal to find dullness over the liver and heart.
 Activity
Activity
 Activity
ActivityTo help discriminate between hollow and flat sounds
Try tapping various parts of an internal wall, see if you can distinguish between the hollow sound of the unsupported plaster board and the flat sound of the solid wood or concrete support.
 |
| Fig. 27.7 Percussion |
Voice sounds are also part of auscultation of the lung. Normally, vocal resonance or voice sounds are heard but the sounds are muffled and indistinct. Hearing clear distinct sounds is an abnormal finding and is caused by the same conditions causing abnormal vocal fremitus.
Various respiratory illnesses produce adventitious sounds that are not normally heard over the chest; these are not alterations in normal breath sounds but are additional abnormal sounds.
The effects of inadequate respiration can be seen by examining heart rate, skin colour and mental status. These are linked to the examination of circulation and disability.
C. Circulation
Adequacy of circulation is assessed by examining the cardiovascular status and looking for the effects of circulatory inadequacy on other organs.
Vital signs
The child’s vital signs should be appropriate for the child’s age and clinical condition. A child normally has a faster heart rate (Table 27.4) and respiratory rate and a lower arterial pressure than an adult. The child’s heart rate and pulse volume should be assessed by palpating both central and peripheral pulses. It is important to note that normal vital signs are not always appropriate when a child is seriously ill, indeed a normal heart rate and respiratory rate may indicate cardiopulmonary arrest is imminent. Hypoxia produces tachycardia and is to be expected; bradycardia is a sign of respiratory failure and a preterminal sign. Absent peripheral and weak central pulses are signs of advanced shock and hypotension in children.
| Age (years) | Beats/min |
|---|---|
| <1 | 110–160 |
| 2–5 | 95–140 |
| 5–12 | 80–120 |
| <12 | 60–100 |
An accurate pulse should be measured for a full minute and be consistent with the apex beat. If measuring the heart rate of children less than 2 years of age, a stethoscope should be placed over the apex of the heart and the beats counted for a full minute. Sinus tachycardia is common in the unwell anxious child and further assessment should be carried out to identify the cause.
Blood pressure (Table 27.5)

The size of the child’s limb must be taken into consideration when taking blood pressure. Make sure the width of the blood pressure (BP) cuff is about two-thirds the length of the child’s upper arm (Fig. 27.8). A cuff that is too large may produce a reading that is too low; a cuff that is too small may give a false high reading (Brown 2007).
| Age (years) | Systolic blood pressure |
|---|---|
| <1 | 70–90 |
| 2–5 | 80–100 |
| 5–12 | 90–110 |
| >12 | 100–120 |
 |
| Fig. 27.8 Observation of a child’s blood pressure. |
Children in early shock may have a normal blood pressure reading initially, hypotension is often a late sign and preterminal sign of circulatory failure. Small quantitative changes in the child’s blood pressure may indicate significant qualitative changes in the child’s clinical condition. It is therefore imperative that accurate and current observations are taken into account when assessing the child’s circulatory status.
Skin perfusion and body temperature
The skin colour and temperature should be consistent over the trunk and limbs. Clinical signs of poor perfusion include peripherally cool skin, pallor, mottling, peripheral cyanosis and capillary refill >2 seconds. By the time central cyanosis is visible in acute respiratory distress respiratory arrest is very close. Capillary refill is a quick and easy method for determining the efficacy of respiratory function. A raised digit is pressed for 5 seconds and the time taken for blood to return to the area is estimated in seconds. A capillary refill time of greater than 2 seconds in a child and 3 seconds in a neonate is a sign of poor oxygenation. Ambient temperature should always be considered in the interpretation of capillary refill.
The normal circadian range of infant’s temperatures over the 24-hour period has been described as ranging from 36°C at night to 37.8°C during active periods in the day (Table 27.6). In addition, there is now recognised to be a variable fluctuation between individuals of 0.5°C (Mackowiak et al 1992). Therefore we should accept individual variations in normal body temperature, recognising that time of day and age of child may affect expected normal values.
| Age (years) | Temperature (°C) |
|---|---|
| <1 | 37.5–37.7 |
| 2–5 | 37.0–37.2 |
| 5–12 | 36.7–36.8 |
| >12 | 36.6 |
D. Disability
Parents are usually the first to recognise any changes in their child’s level of consciousness and it is therefore important to listen to what they say. A hypoxic child may be irritable or agitated early on but increasingly lethargic later. He or she might fail to recognise or interact, e.g. maintain eye contact, with the parents or might not respond to stimuli, e.g. unfamiliar nurses. A progressive drop in level of consciousness is a late sign of hypoxia and may be an indication of impending respiratory distress. Other factors that may lead to a decreasing level of consciousness are shock, sepsis, ingestion of depressants, metabolic abnormalities, hypothermia and head injuries. The level of consciousness should be assessed using the AVPU scale:
Any problem with ABC must be addressed before assuming that a decrease in conscious level is due to a primary neurological problem.
The final but integral part of the child’s assessment is their medical history. Factors to be taken into consideration include the following symptoms:
• Is the child breathless:
• When? At rest, walking, talking, sleeping, feeding?
• Does the child have a cough?
• What type?
• How long has the child had this?
• When do the symptoms occur – daytime, night-time?
• Are the symptoms improving or worsening?
• Are there any aggravating or precipitating factors? Does anything relieve the symptoms?
• Are the symptoms associated with anything, e.g. feeding? Is the child able to take feeds?
• How long has the child been unwell, has this happened suddenly, did it occur over time?
• Does the child have a sore throat?
• Is there any nasal discharge, has the child a cough, is the cough productive, what colour is the sputum, how long have these been present?
• Has the child’s sleep been affected?
• Is the child’s breathing noisy, in what way? Ask the parents to describe any noises they have heard.
• What has the child’s activity level been like?
Less specific symptoms to observe for include:




• pyrexia
• urinary output
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access

