Rehabilitation and Restorative Nursing Care
Objectives
• Define the key terms and key abbreviations in this chapter.
• Describe how rehabilitation and restorative care involve the whole person.
• Identify the complications to prevent.
• Identify the common reactions to rehabilitation.
• Explain your role in rehabilitation and restorative care.
• List the common rehabilitation programs and services.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
Disease, injury, and surgery can affect body function. So can birth injuries and birth defects (Chapter 50). Often more than 1 function is lost.
A disability is any lost, absent, or impaired physical or mental function. Causes are acute or chronic (Box 41-1).
• An acute problem has a short course with complete recovery. A fracture (broken bone) is an example.
Disabilities can affect eating, bathing, dressing, walking, and the ability to work. These daily activities and others are hard or seem impossible. The degree of disability affects how much function is possible. The person may depend totally or in part on others for basic needs.
Rehabilitation is the process of restoring the person to his or her highest possible level of physical, psychological, social, and economic function. The goals of rehabilitation are to:
Some persons return home after rehabilitation. The process may continue in home or community settings.
See Focus on Long-Term Care and Home Care: Rehabilitation and Restorative Nursing Care.
Restorative Nursing
Some persons are weak. Many cannot perform daily functions. Restorative nursing care is care that helps persons regain health, strength, and independence. With progressive illnesses, disabilities increase. Restorative nursing:
Restorative nursing measures promote:
Many persons need restorative nursing and rehabilitation. In many agencies, they mean the same thing. Both focus on the whole person.
Restorative Aides
Some agencies have restorative aides. A restorative aide is a nursing assistant with special training in restorative nursing and rehabilitation skills. These aides assist the nursing and health teams as needed. Required training varies among states. If there are no state requirements, the agency provides needed training.
Rehabilitation and the Whole Person
A health problem has physical, psychological, and social effects. So does a disability. Suppose an illness left you paralyzed from the waist down.
• Would you be angry, afraid, or depressed?
• How would you care for yourself and your family?
• How would you worship, shop, or visit friends?
The person needs to adjust physically, psychologically, socially, and economically. Abilities—what the person can do—are stressed. Complications may cause further disability.
See Focus on Children and Older Persons: Rehabilitation and the Whole Person.
Physical Aspects
Rehabilitation starts when the person first seeks health care. Complications are prevented. They can occur from bedrest, a long illness, or recovery from surgery or injury. Bowel and bladder problems are prevented. So are contractures and pressure ulcers. Good alignment, turning and re-positioning, range-of-motion (ROM) exercises, and supportive devices are needed (Chapters 17, 18, and 30). Good skin care also prevents pressure ulcers (Chapters 22 and 37).
Elimination.
Some persons need bladder training (Chapter 24). The method depends on the person’s problems, abilities, and needs. Some need bowel training (Chapter 26). Control of bowel movements and regular elimination are goals. Fecal impaction, constipation, and fecal incontinence are prevented.
Self-Care.
Self-care is a major goal. Activities of daily living (ADL) are the activities usually done during a normal day in a person’s life. ADL include bathing, oral hygiene, dressing, eating, elimination, and moving about. The health team evaluates the person’s ability to perform ADL.
Sometimes the hands, wrists, and arms are affected. Adaptive (assistive) devices are often needed. Equipment is changed, made, or bought to meet the person’s needs.
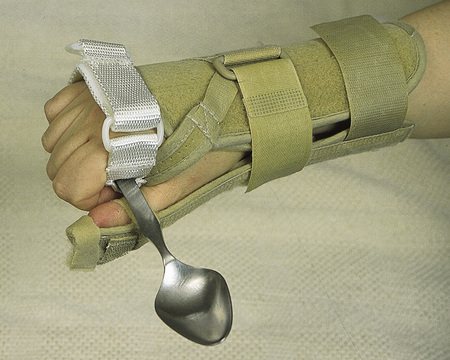
• Eating devices include glass holders, plate guards, and silverware with curved handles or cuffs (Chapter 27). Some devices attach to splints (Fig. 41-1, p. 668).
• Electric toothbrushes have back-and-forth brushing motions for oral hygiene.
• Adaptive (assistive) devices for hygiene promote independence.
Adaptive (assistive) devices are useful for cooking, dressing, writing, phone calls, and other tasks. Some are shown in Figure 41-2, p. 668. Also see Chapters 22 and 23.
See Focus on Surveys: Self-Care, p. 668.
Mobility.
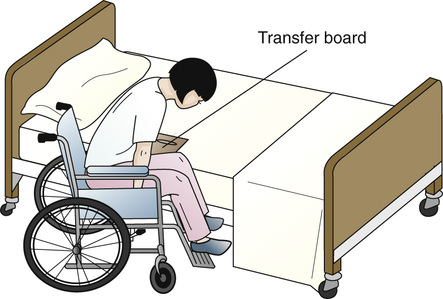
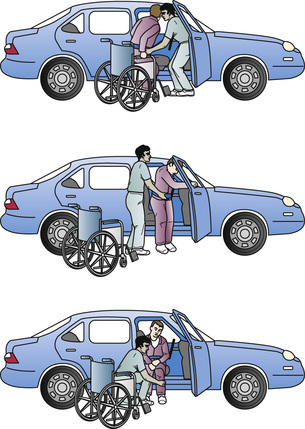
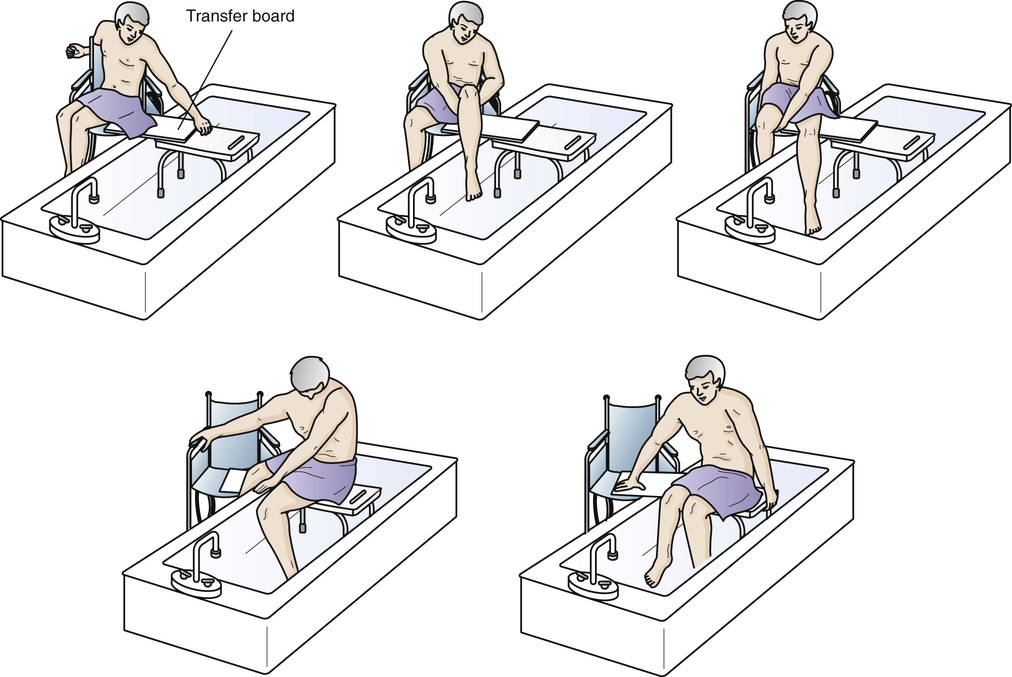
The person may need crutches or a walker, cane, or brace (Chapter 30). Physical and occupational therapies are common for musculo-skeletal and nervous system problems (Fig. 41-3). Some people need wheelchairs. If possible, they learn wheelchair transfers. Such transfers include to and from the bed, toilet, bathtub, sofa, and chair and in and out of vehicles (Figs. 41-4, 41-5, and 41-6, p. 670).
A prosthesis is an artificial replacement for a missing body part. The person learns how to use the artificial arm or leg (Chapter 44). The goal is for the device to be like the missing body part in function and appearance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree