Public Health Nursing and the Disaster Management Cycle
Objectives
After reading this chapter, the student should be able to do the following:
1. Discuss types of disasters, including natural and human made.
2. Assess how disasters affect people and their communities.
4. Examine the nurse’s role in the disaster management cycle.
5. List sources of competencies for public health nursing practice in disaster.
7. Identify organizations in which nurses can volunteer to work in disasters.
Key Terms
American Red Cross, p. 516
BioSense, p. 520
bioterrorism, p. 509
BioWatch, p. 520
CBRNE threats: chemical, biological, radiological, nuclear, and explosive, p. 512
Cities Readiness Initiative, p. 520
Community Emergency Response Team (CERT), p. 516
community resilience, p. 518
Disaster Medical Assistance Team (DMAT), p. 516
Emergency Support Functions (ESFs), p. 518
general population shelters, p. 526
Homeland Security Act of 2002, p. 510
Homeland Security Exercise and Evaluation Program (HSEEP), p. 518
Homeland Security Presidential Directive-5 (HSPD-5), p. 510
Homeland Security Presidential Directive-8 (HSPD-8), p. 510
Homeland Security Presidential Directive-21 (HSPD-21): Public Health and Medical Preparedness, p. 511
human-made disaster, p. 509
human-made incident, p. 508
Medical Reserve Corps (MRC), p. 516
mitigation, p. 511
mutual aid agreements, p. 516
National Disaster Medical System (NDMS), p. 515
National Health Security Strategy (NHSS), p. 511
National Incident Management System (NIMS), p. 510
National Preparedness Guidelines (NPG), p. 510
National Response Framework (NRF), p. 510
pandemic, p. 509
Pandemic and All-Hazards Preparedness Act (PAHPA), p. 511
personal protective equipment (PPE), p. 514
Point of Dispensing (POD), p. 512
Project BioShield, p. 520
Public Health Nursing Intervention Wheel, p. 514
Public Health Security and Bioterrorism Preparedness and Response Act of 2002, p. 516
public health surge, p. 509
public health triage, p. 524
rapid needs assessment, p. 524
risk communication, p. 525
special needs shelters, p. 526
Strategic National Stockpile (SNS), p. 520
triage, p. 524
vicarious traumatization, p. 526
—See Glossary for definitions
 Susan B. Hassmiller, PhD, RN, FAAN
Susan B. Hassmiller, PhD, RN, FAAN
Dr. Susan Hassmiller is the Senior Advisor for Nursing at the Robert Wood Johnson Foundation in Princeton, New Jersey, and Director of the RWJF Initiative on the Future of Nursing, at the Institute of Medicine in Washington, D.C. The Foundation provides support to improve the health and health care for all Americans. Dr. Hassmiller has taught public health nursing at the university level and has dedicated her career to the care and prevention of disease in vulnerable populations. She is a former member of the National Board of Governors for the American Red Cross, having served as the Chair of Chapter and Disaster Services. She is currently on the board of the Central New Jersey Chapter of the American Red Cross. She is a 2002 recipient of both the national American Red Cross Ann Magnussen Award and the regional American Red Cross Clara Barton Award, both recognizing her outstanding leadership in the field of nursing and disaster services. She is the 2009 recipient of the Florence Nightingale Medal of Honor, the highest award in nursing presented by the International Committee of Red Cross in Geneva, Switzerland. She oversees the annual Susan Hassmiller American Red Cross Award, which provides recognition to a Red Cross chapter that has made outstanding contributions in providing disaster health services involving nurses as leaders.
 Sharon A. R. Stanley, PhD, RN, RS
Sharon A. R. Stanley, PhD, RN, RS
Dr. Sharon Stanley is the Chief Nurse of the American Red Cross and the Director of Disaster Health Services and Mental Health. She has worked in the public health field for over 30 years, with experience as a county Health Commissioner and faculty member at private and public institutions. Her past positions in public health preparedness include Director of the Ohio Center for Public Health Preparedness, The Ohio State University, and Chief of Disaster Planning, Ohio Department of Health. Colonel Stanley retired from the U.S. Army Reserve in 2007 with 34 years of service, 12 of them active duty. Her military assignments include a three-state Brigade level command and Army Reserve Leadership Campaign Chief, assigned to the Pentagon. She is the recipient of numerous military awards, including the Order of Medical Military Merit. Dr. Stanley is a member of the Institute of Medicine Forum for Medical and Public Health Preparedness for Catastrophic Events, the Working Panel for Integration of Civilian and Military Domestic Disaster Medical Response, and the Federal Nursing Service Council, which includes the Chief Nurses of the Army, Navy, Air Force, Public Health Service, and Veterans Administration. She is a recent graduate of the Center for Homeland Security and Defense, Naval Postgraduate School, where she completed research in the field of mass fatality management.
The authors wish to acknowledge the manuscript review and consultation of a review committee, which included Donna Jensen, PhD, RN, Professor Emeritus, Oregon Health and Science University and Disaster Health Services Manager, Oregon Trail Chapter, American Red Cross; Janice Springer, RN, PHN, MA, Nurse Manager and Recruiter for Concordia Language Villages and Disaster Health Services Advisor and State Nurse Liaison for Minnesota, American Red Cross; and Barbara J. Polivka, PhD, RN, Associate Professor, College of Nursing, The Ohio State University.
“Wherever disaster calls there I shall go. I ask not for whom, but only where I am needed.”
From the Creed of the Red Cross Nurse by Lona L. Trott, RN, 1953
Around the world, people are experiencing unprecedented disasters from natural causes like hurricanes and earthquakes to human-made disasters such as oil spills and terrorism.
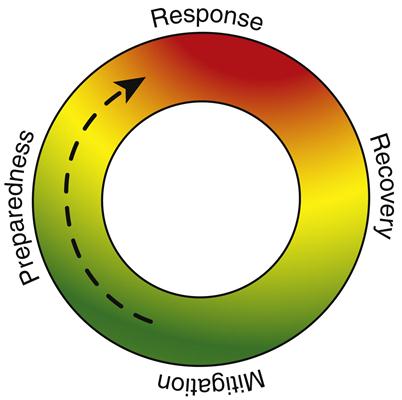
Disasters, whether human-made or natural, are inevitable, but there are ways to help communities prepare for, respond to, and recover from disaster. This chapter describes disaster management approaches including phases of prevention, preparedness, response, and recovery. The public health nurse’s role in these phases is described.
Defining Disasters
A disaster is any natural or human-made incident that causes disruption, destruction, and/or devastation requiring external assistance. Although natural incidents like earthquakes or hurricanes trigger many disasters, predictable and preventable human-made factors can further affect the disaster. On August 30, 2005, the day after Hurricane Katrina hit New Orleans, a breach in the Lake Pontchartrain levees created a disaster within a disaster as 75% of the city filled with up to 20 feet of water (Reagan, 2005). The flooding of New Orleans has been called the largest civil engineering disaster in the history of the United States (Marshall, 2005). Box 23-1 lists examples of natural and human-made disasters.
From a health care standpoint, the disaster event type and timing predict subsequent injuries and illnesses. If there is prior warning (e.g., in hurricanes or slow-rising floods), the impact brings fewer injuries and deaths. Disasters with little or no advance notice such as terrorism events will often have more casualties because those affected have little time to make evacuation preparations. Disasters with warnings also carry their own dangers, because individuals can be injured attempting to prepare for the disaster or while evacuating. Public health disasters create pressing needs across a widespread region. In a pandemic, pressing and competing health needs occur within a close timeframe, producing a public health surge. In the recovery disaster phase, the immediate threat shifts to adjusting to a new normal in the affected community or region.
Disaster Facts
Disasters can affect one family at a time, as in a house fire, or they can kill thousands and result in economic losses in the millions, as with floods, earthquakes, tornadoes, hurricanes, tsunamis, and bioterrorism. The American Red Cross reports that it responds to a disaster in the United States every 8 minutes, resulting in response to over 70,000 incidents each year (American Red Cross, 2009).
The number of reported natural and human-made disasters continues to rise worldwide. Although the number of lives lost declined over the past 20 years—800,000 people died from natural disasters in the 1990s, compared with 2 million in the 1970s—the number of people affected increased. In one decade, the number affected tripled to 2 billion (UN Office for the Coordination of Humanitarian Affairs, 2005). The increase in the number of lives saved may be explained by better forecasting and early warning systems (International Federation of Red Cross and Red Crescent Societies, 2009). Within a 1-week period in the fall of 2009, three disasters—a tsunami in the Samoa Islands, an earthquake in Indonesia, and a typhoon in the Philippines and Vietnam—collectively left over 1000 dead, hundreds of thousands homeless, and caused millions of dollars in damages (Thomson Reuters Foundation, 2009). Two disasters in 2008 accounted for 93% of all people dead or missing in disasters: Cyclone Nargis in Myanmar and the Sichuan earthquake in China took over 225,000 lives (International Federation of Red Cross and Red Crescent Societies, 2009). The Centers for Disease Control and Prevention (CDC) estimates that between 41 million and 84 million cases of H1N1 occurred between April 2009 and January 16, 2010 in the United States, with 17,000 deaths, 1800 of them children (Fox, 2010). The 2010 Haiti earthquake (Figure 23-1) claimed an estimated 230,000 lives, left 1.5 million Haitians homeless, and destroyed the nation’s capital (American Red Cross, 2010d).

Disaster disproportionably strikes at-risk individuals, whether their day-to-day risk is physical, emotional, or economic. Disasters can also wipe out decades of progress in a matter of hours, in a manner that rarely happens in more developed countries. The poor, elderly, women, and children in developing communities are excessively affected and least able to rebound (Duque, 2005). Unfortunately by 2050, the percentages of population areas more vulnerable to disasters will increase. Eighty percent of the world’s population will live in developing countries, while 46% will live in tornado and earthquake zones, near rivers, and on coastlines (United Nations Development Programme, 2001; NASA, 2005).
The monetary cost of disaster recovery efforts also rose sharply. The cost in more developed countries is higher because of the extent of material possessions and complex infrastructure, including technology. In the United States, increases in population and development in areas vulnerable to natural disasters, especially coastal areas, have led to major increases in insurance payouts (see Table 23-1).
TABLE 23–1
| 2009 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | Total | |
| Africa | 173 | 1,243 | 805 | 436 | 6,455 | 1,908 | 38 | 244 | 782 | 863 | 12,947 |
| Americas | 13,337 | 6,800 | 15,946 | 15,386 | 25,085 | 74,679 | 189,370 | 7,226 | 16,625 | 64,162 | 428,616 |
| Asia | 15,449 | 27,108 | 15,687 | 15,855 | 27,630 | 75,332 | 30,494 | 24,873 | 35,747 | 117,927 | 386,102 |
| Europe | 10,789 | 22,176 | 2,395 | 40,283 | 21,415 | 2,072 | 17,261 | 2,584 | 22,796 | 4,644 | 146,414 |
| Oceania | 1,726 | 668 | 696 | 2,601 | 691 | 627 | 241 | 1,368 | 1,488 | 2,506 | 12,612 |
| Very high development | 24,655 | 39,272 | 16,087 | 60,332 | 50,959 | 122,083 | 192,144 | 11,694 | 46,461 | 64,178 | 627,865 |
| High human development | 2,412 | 2,259 | 3,952 | 3,328 | 2,907 | 7,058 | 14,607 | 2,041 | 11,564 | 6,360 | 56,488 |
| Medium human development | 14,234 | 8,370 | 15,421 | 10,842 | 27,178 | 24,878 | 30,641 | 22,557 | 18,922 | 119,537 | 292,579 |
| Low human development | 173 | 8,094 | 69 | 60 | 233 | 600 | 12 | 3 | 489 | 27 | 9,760 |
| Total | 41,474 | 57,995 | 35,528 | 74,561 | 81,277 | 154,619 | 237,404 | 36,295 | 77,436 | 190,102 | 986,691 |
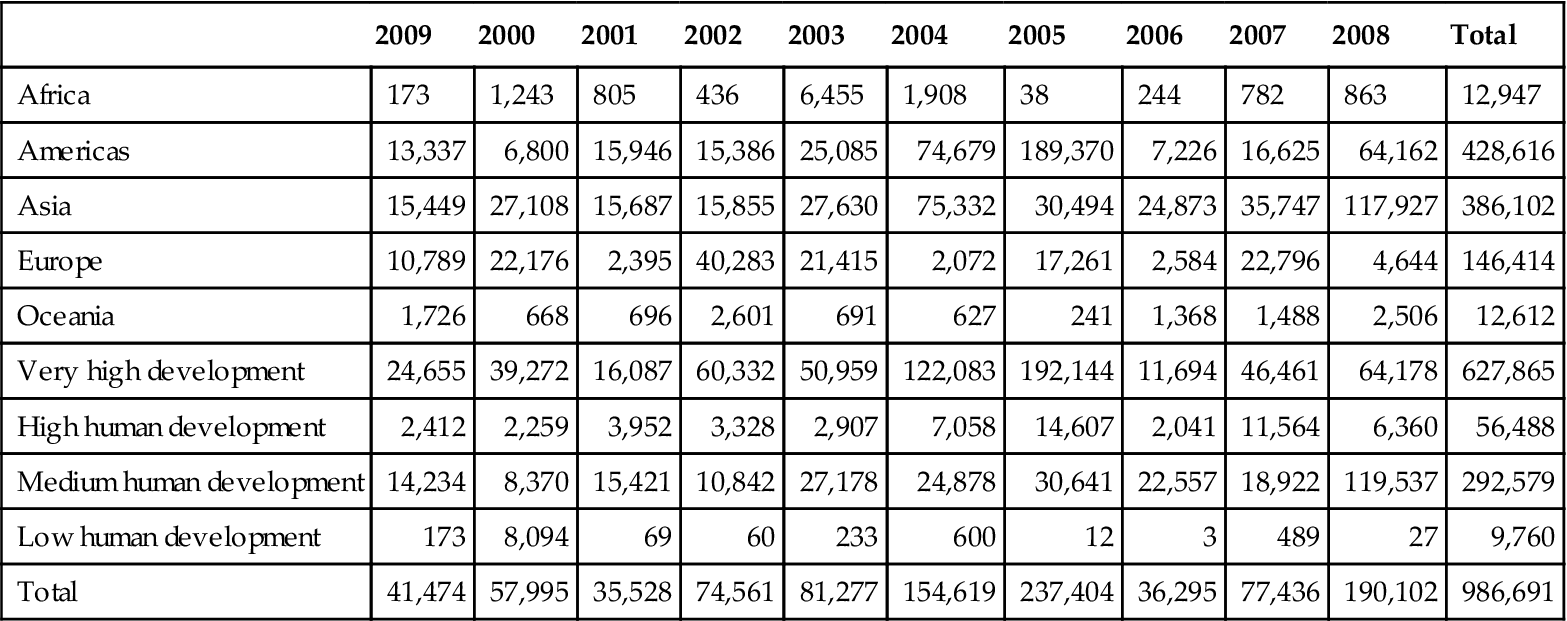
n.a., no data available. For more information, see section on caveats in introductory text.
Damage assessment is often unreliable. Even for existing data, the methodologies are not standardized and the financial coverage can vary significantly. Depending on where the disaster occurred and who reports it, estimations may vary from zero to billions of U.S. dollars. The total amount of damage reported in 2009 is the third lowest of the decade.
From International Federation of Red Cross and Red Crescent Societies: World disasters report 2010: Focus on urban risk, Geneva, Switzerland, 2010, ATAR Roto Presse, p 167.
Homeland Security: A Health-Focused Overview
There is a concerted national effort to provide guidance to state and local planning regions to assist with the coordinated and successful responses and recovery efforts in all-hazard disasters and catastrophes. Many documents have been written at the national level, some of which will be reviewed in this overview and chapter.
The reader may ask: “Isn’t this all beyond what an individual nurse should have to know?” Actually, it matters greatly how the nation dials 911, and it matters to individuals as well as communities, regions, and the country as a whole. It also matters globally, beyond our own borders. Our national response is not just about the United States, but our international ability to assist other nations in their times of need.
As the single largest profession within the health care network, nurses must understand the national disaster management cycle. Without nursing integration at every phase, communities and clients lose a critical part of the prevention network, and the multidisciplinary response team loses a first-rate partner.
The U.S. Department of Homeland Security was created through the Homeland Security Act of 2002 (DHS, 2008b), consolidating more than 20 separate agencies into one unified organization.
Homeland Security Presidential Directive-8 (HSPD-8) was issued in December of 2003. It established national policies to strengthen the preparedness of the United States to prevent, protect against, respond to, and recover from threatened or actual terrorist attacks and major disasters, and it included a goal for national preparedness (DHS, 2008c). The national preparedness goal resulted in the National Preparedness Guidelines (NPG) and The National Response Plan (NRP), a national doctrine for preparedness to include Emergency Support Function (ESF) 8: Public Health and Medical (DHS, 2008a). ESF 8 provides coordinated federal assistance to supplement state, local, and tribal resources in response to public health and medical care needs. The 2004 NRP, an all-discipline, all-hazards comprehensive framework for managing domestic incidents, was updated to the National Response Framework (NRF) in January 2008. The NRF remains a guide for conducting a nationwide all-hazards response, “built upon scalable, flexible, and adaptable coordinating structures to align key roles and responsibilities across the Nation, linking all levels of government, nongovernmental organizations, and the private sector” (DHS, 2008d, p i).
Homeland Security Presidential Directive-5 (HSPD-5) directed the Secretary of Homeland Security to develop and administer the National Incident Management System (NIMS), a unified, all-discipline, and all-hazards approach to domestic incident management (DHS, 2008c). The NIMS was established to provide a common language and structure enabling all those involved in disaster response the ability to communicate together more effectively and efficiently.
Two national preparedness documents specifically guide disaster health preparedness, response, and recovery: HSPD 21: Public Health and Medical Preparedness and the National Health Security Strategy (NHSS). HSPD 21 established a national strategy that enables a level of public health and medical preparedness sufficient to address a range of possible disasters. It does so through four critical components of public health and medical preparedness: (1) biosurveillance, (2) countermeasure distribution, (3) mass casualty care, and (4) community resilience (DHS, 2008c). The NHSS focuses specifically on the national goals for protecting people’s health in the case of disaster in any setting. National health security is achieved when “the Nation and its people are prepared for, protected from, respond effectively to, and able to recover from incidents with potentially negative health consequences” (USDHHS, 2009, p 2). The NHSS was directed by the Pandemic and All-Hazards Preparedness Act (PAHPA), which was enacted in 2006 to improve the nation’s ability to detect, prepare for, and respond to a variety of public health emergencies (Hodge, Gostin, and Vernick, 2007).
In discussing community resiliency and impact of health care reform on public health preparedness, Vinter, Lieberman, and Levi (2010) state: “Comprehensive health reform presents a rare opportunity to further strengthen our nation. However, even with health reform, there are still major gaps in our public health preparedness. Addressing these underlying weaknesses in our health system will not be easy or cheap, but failure to address these concerns could prove extremely costly” (p 340).
It should be apparent by this point that our national system of homeland security includes public health preparedness and response as a core part of its national strategies. Some of the strategy documents introduced in this section are covered in greater detail throughout the chapter. Every aspect of disaster management involves public health nursing.
Healthy People 2020 Objectives
Because disaster affects the health of people in many ways, disaster incidents have an effect on almost every Healthy People 2020 objective. For example, although Access to Health Services and Public Health Infrastructure comprise two important Healthy People 2020 topic areas with subsequent objectives, they become even more significant when individual and community needs escalate in disaster (USDHHS, 2010). Disasters also play a direct role in the objectives related to environmental health, food safety, immunization and infectious disease, and mental health and mental disorders. Public health professionals, such as those who work at the CDC, study the effect that disasters have on population health and continuously develop new prevention strategies. Other organizations, such as the American Psychological Association and the American Red Cross, work with communities in the preparedness, response, and recovery phases of a disaster and to revise and align the Healthy People 2020 objectives related to mental health.
The Disaster Management Cycle and Nursing Role
Disaster management includes four stages: prevention (or mitigation), preparedness, response, and recovery. Figure 23-2 shows the disaster emergency management cycle. Nurses have unique skills for all aspects of disaster to include assessment, priority setting, collaboration, and addressing of both preventive and acute care needs. In addition, public health nurses have a skill set that serves their community well in disaster to include health education and disease screening, mass clinic expertise, an ability to provide essential public health services, community resource referral and liaison work, population advocacy, psychological first aid, public health triage, and rapid needs assessment. Nurses have been serving in disasters for more than a century, and to this day, provide a significant resource to both the employee and the volunteer disaster management workforce, unmatched by any other profession.
The World Association for Disaster and Emergency Medicine (WADEM) includes a nursing section. The Nursing Section of WADEM serves to welcome and represent nurses from all countries with an intent and desire to strengthen and improve the practice and knowledge of disaster nursing. The Nursing Section purposes are as follows (WADEM, 2010):
• Define nursing issues for public health care and disaster health care
• Exchange scientific and professional information relevant to the practice of disaster nursing
• Encourage collaborative efforts enhancing and expanding the field of nursing disaster research
• Encourage collaboration with other nursing organizations
• Inform and advise WADEM of matters related to disaster nursing
WADEM sponsored a text entitled International Disaster Nursing that was edited in 2010 by Robert Powers and Elaine Daily and is available from Cambridge University Press.
Prevention (Mitigation)
All-hazards mitigation (prevention) is an emergency management term for reducing risks to people and property from natural hazards before they occur. Prevention can include structural measures, such as protecting buildings and infrastructure from the forces of wind and water, and non-structural measures, such as land development restrictions. These primary prevention measures implemented at the local government level achieve effectiveness, in an all-hazards approach to threats. Of course, prevention also includes human-made hazards and the ability to deter potential terrorists, detect terrorists before they strike, and take decisive action to eliminate the threat (DHS, 2007b). Prevention activities may include heightened inspections; improved surveillance and security operations; public health and agricultural surveillance; and testing, immunizations, isolation, or quarantine and halting of CBRNE threats: chemical, biological, radiological, nuclear, and explosive (DHS, 2007b).
Within the community, the nurse may be involved in many roles in prevention of disaster. As community advocates, nurses partner for environmental health by identifying environmental hazards and serving on the public health team for mitigation purposes. Public health nurses in particular will be involved with organizing and participating in mass prophylaxis and vaccination campaigns to prevent, treat, or contain a disease. The nurse should be familiar with the region’s local cache of pharmaceuticals and how the Strategic National Stockpile (SNS) (described later in the chapter) will be distributed. Once federal and local authorities agree that the SNS is needed, medicine delivery to any state in the United States occurs within 12 hours (CDC, 2009b). Then state and local emergency planners ensure Points of Dispensing (POD), to provide prophylaxis to the entire population within 48 hours (CDC, 2007).
In terms of human-made disaster prevention, the nurse should be aware of high-risk targets and current vulnerabilities and what can be done to eliminate or mitigate the vulnerability. Targets may include military and civilian government facilities, health care facilities, international airports and other transportation systems, large cities, and high-profile landmarks. Terrorists might also target large public gatherings, water and food supplies, banking and finance, information technology, postal and shipping services, utilities, and corporate centers.
Preparedness
Role of the Public Health Nurse in Personal and Professional Preparedness
Public health nurses play a key role in community preparedness, but they must accomplish the critical elements of personal and professional preparedness first.
Personal Preparedness
Disasters by their nature require nurses to respond quickly. Public health nurses without plans in place to address their own needs, to include family and pets, will be unable to fully participate in their disaster obligations at work or in volunteer efforts (Figure 23-3). Many first responders left their jobs to care for their homes and their families when Hurricane Katrina occurred. In addition, the nurse assisting in disaster relief efforts must be as healthy as possible, both physically and mentally. A disaster worker who does not practice self-health is of little service to their family, clients, and community (see the How To box titled Be Red Cross Ready). Disaster kits should be made for the home, workplace, and car. The Nursing Tip lists emergency supplies specific to nursing that should be prepared and stored in a sturdy, easy-to-carry container. Important documents should always be in waterproof containers. Nurses should consider several contingencies for children and older adults with a plan to seek help from neighbors in the event of being called to a disaster. Many public shelters do not allow pets inside and other arrangements must be made. Currently, local emergency management agencies include pet management in the local disaster plans (FEMA, 2009d). During Hurricane Katrina, in Hattiesburg, MS, 2385 pets were rescued and subsequently sheltered (Reagan, 2005).
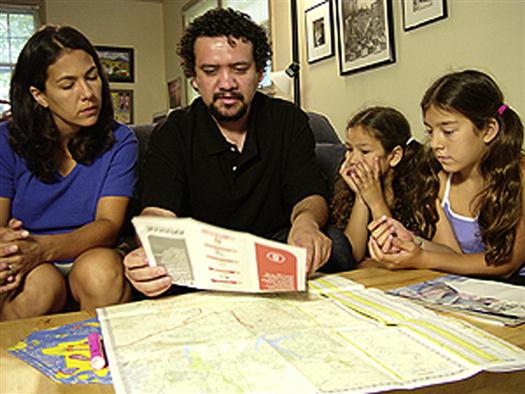
One way a nurse can feel assured about family member protection is by working with them to develop the skills and knowledge necessary for coping in disaster. For example, long-term benefits will occur by involving children and adolescents in activities such as writing preparedness plans, exercising the plan, preparing disaster kits, becoming familiar with their school emergency procedures and family reunification sites, and learning about the range of potential hazards in their vicinity to include evacuation routes. This strategy also offers children and adolescents an opportunity to express their feelings.
Professional Preparedness
Every state needs a qualified workforce of public health nurses for solutions for today’s public health problems to include natural disasters and the threat of terrorism. Public health nurses, in turn, need “dedicated, resourceful, and visionary leaders” (ASTDN, 2008, p 4). Chief public health nurse officers at the state level develop and maintain a strong public health nursing workforce (ASTDN, 2008). Disaster management in the community is about population health: The core public health functions of assessment, policy development, and assurance hold as true in disaster as in day-to-day operations. Operating in the chaos of disaster surge, however, demands a flexible and proficient practice base in each of the core functions and 10 essential services.
Just like the mission of public health and its core functions and essential services does not change in disaster, neither does the practice of public health nursing. The public health nurse must be prepared to advocate for the community in terms of a focus on population-based practice. The number of public health nurses available to get the job done is small compared with those with generic or other specialty nurse preparation. Also, disaster produces conditions that demand an aggregate care approach, increasing the need for public health nursing involvement in community service during disaster and catastrophe.
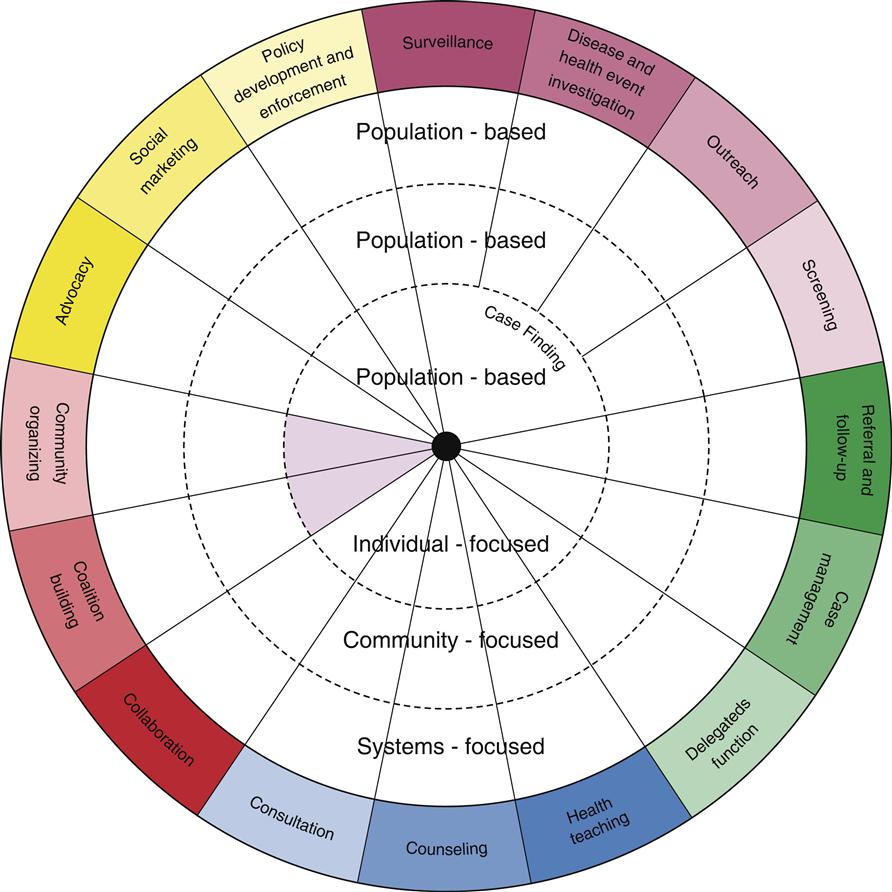
The Public Health Nursing Intervention Wheel (Figure 23-4) is explained in detail in Chapter 9 and is a population-based practice model that encompasses three levels of practice (community, systems, and individual/family) and 16 public health interventions. Each intervention and practice level contributes to improving population health, providing a practice foundation. This Wheel holds true to public health nursing interventions whether the nurse is working in day-to-day or in disaster operations.
Disaster response teams need nurses with disaster and emergency management training, especially those who have served previously in disaster. Although the majority of disaster work is not high tech, the knowledge one needs for CBRNE disasters must be developed to include access to a ready cache of information related to nursing care. The following sites provide useful information:
• CDC: Emergency preparedness and response A to Z index (http://www.bt.cdc.gov/agent)
• National Library of Medicine: Disaster information management research center (http://disaster.nlm.nih.gov/)
• Unbound Medicine: Relief Central (http://relief.unboundmedicine.com/relief/ub/)
• National Library of Medicine: WISER-Wireless information system for emergency responders (http://wiser.nlm.nih.gov/) (See Box 23-2 for further information.)



