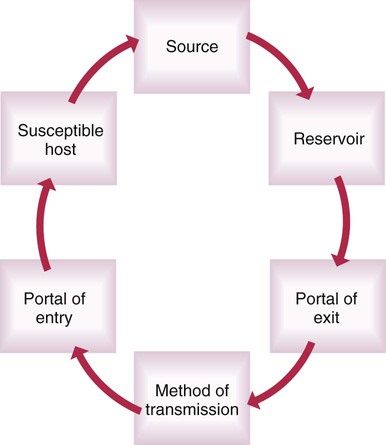
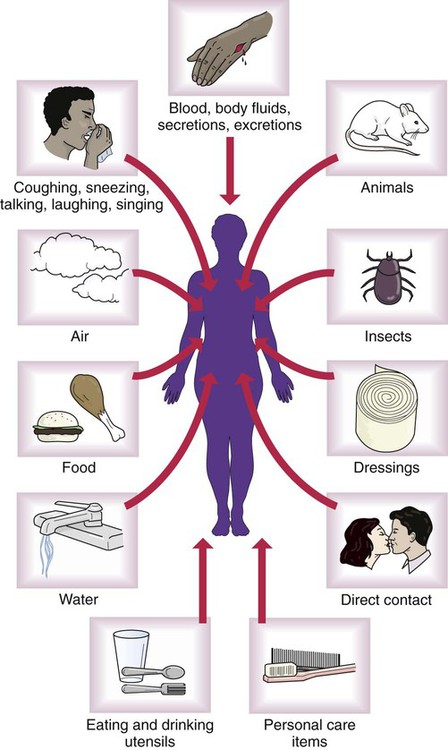
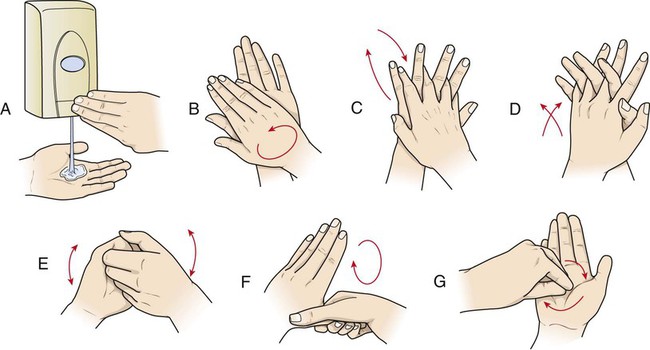
AIIR Airborne infection isolation room CDC Centers for Disease Control and Prevention HAI Healthcare-associated infection HIV Human immunodeficiency virus MDRO Multidrug-resistant organism MRSA Methicillin-resistant Staphylococcus aureus OPIM Other potentially infectious materials OSHA Occupational Safety and Health Administration PPE Personal protective equipment SARS Severe acute respiratory syndrome • Define the key terms and key abbreviations listed in this chapter. • Identify what microbes need to live and grow. • List the signs and symptoms of infection. • Explain the chain of infection. • Describe healthcare-associated infections and the persons at risk. • Describe the principles of medical asepsis. • Explain how to care for equipment and supplies. • Describe disinfection and sterilization methods. • Describe Standard Precautions and Transmission-Based Precautions. • Explain the Bloodborne Pathogen Standard. • Perform the procedures described in this chapter. • Explain how to promote PRIDE in the person, the family, and yourself. • Methicillin-resistant Staphylococcus aureus (MRSA). Staphylococcus aureus (“staph”) is a bacterium normally found in the nose and on the skin. MRSA is resistant to antibiotics often used for “staph” infections. MRSA can cause pneumonia and serious wound and bloodstream infections. • Vancomycin-resistant Enterococci (VRE). Enterococcus is a bacterium normally found in the intestines and in feces. It can be transmitted to others by contaminated hands, toilet seats, care equipment, and other items that the hands touch. When not in their natural site (the intestines), enterococci can cause urinary tract, wound, pelvic, and other infections. Enterococci resistant to the antibiotic vancomycin are called vancomycin-resistant Enterococci (VRE). A local infection is in a body part. A systemic infection involves the whole body. (Systemic means entire.) The person has some or all of the signs and symptoms listed in Box 12-1. See Focus on Older Persons: Infection. See Focus on Surveys: Infection. The chain of infection (Fig. 12-1) begins with a source—a pathogen. It must have a reservoir where it can grow and multiply. Humans, animals, and objects are reservoirs. A carrier is a human or animal that is a reservoir for microbes but does not develop the infection. Carriers can pass pathogens to others. To leave the reservoir, the pathogen needs a portal of exit. Exits are the respiratory, gastro-intestinal (GI), urinary, and reproductive tracts; breaks in the skin; and blood. After leaving the reservoir, the pathogen must be transmitted to another host (Fig. 12-2). The pathogen enters the body through a portal of entry. Portals of entry and exit are the same. A susceptible host is needed for the microbe to grow and multiply. Susceptible hosts are at risk for infection. They include persons who: • Are very young or who are older. • Were exposed to the pathogen. • Do not follow practices to prevent infection. • Are burn patients. When burns destroy the skin, the wound is a portal of entry for microbes. • Are transplant patients. A transplant involves transferring an organ or tissue from 1 person to another person or from 1 body part to another body part. The body’s normal immune response is to attack (reject) the new organ or tissue. Therefore, drugs are given to prevent rejection. Such drugs suppress (prevent) the immune system from producing the antibodies needed to fight infection. • Are chemotherapy patients (Chapter 28). Some types of chemotherapy affect the bone marrow’s ability to produce white blood cells (WBCs). WBCs are needed to fight infection. • Remove or destroy pathogens. The number of pathogens is reduced. • Prevent pathogens from spreading from 1 person or place to another person or place. Aseptic practices break the chain of infection. To prevent the spread of microbes, wash your hands: • After changing tampons or sanitary pads. • After contact with your own or another person’s blood, body fluids, secretions, or excretions. This includes saliva, vomitus, urine, feces, vaginal discharge, mucus, semen, wound drainage, pus, and respiratory secretions. • After coughing, sneezing, or blowing your nose. • Before and after handling, preparing, or eating food. • Provide all persons with their own linens and personal care items. • Cover your nose and mouth when coughing, sneezing, or blowing your nose. If without tissues, cough or sneeze into your upper arm (Fig. 12-3). Do not cough or sneeze into your hands. • Bathe, wash hair, and brush your teeth regularly. • Wash fruits and raw vegetables before eating or serving them. • Wash cooking and eating utensils with soap and water after use. See Focus on Older Persons: Common Aseptic Practices. Hand hygiene is the easiest and most important way to prevent the spread of infection. You use your hands for almost everything. They are easily contaminated. They can spread microbes to other persons or items. Practice hand hygiene before and after giving care. See Box 12-2 for the rules of hand hygiene. See Focus on Surveys: Hand Hygiene. See Promoting Safety and Comfort: Hand Hygiene. See procedure: Hand Washing, p. 145. See procedure: Using an Alcohol-Based Hand Rub, p. 145. Non-disposable items are cleaned and then disinfected. Then they are sterilized. • Wear personal protective equipment (PPE) when cleaning items contaminated with blood, body fluids, secretions, or excretions. PPE includes gloves, a mask, a gown, and goggles or a face shield. • Work from clean to dirty areas. If you work from a dirty to a clean area, the clean area becomes contaminated (dirty). • Rinse the item to remove organic matter. Use cold water. Heat makes organic matter thick, sticky, and hard to remove. • Wash the item with soap and hot water. • Scrub thoroughly. Use a brush if necessary. • Rinse the item in warm water. • Disinfect or sterilize the item. • Disinfect equipment and the sink used in the cleaning procedure. Boiling water, radiation, liquid or gas chemicals, dry heat, and steam under pressure are sterilization methods. An autoclave (Fig. 12-11) is a pressure steam sterilizer. Glass, surgical items, and metal objects are autoclaved. High temperatures destroy plastic and rubber items. They are not autoclaved.
Preventing Infection
Key Abbreviations
Microorganisms
Multidrug-Resistant Organisms
Infection
The Chain of Infection
Susceptible Hosts.
Medical Asepsis
Common Aseptic Practices
![]() Hand Hygiene
Hand Hygiene

Supplies and Equipment
Cleaning.
Sterilization.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Preventing Infection
Get Clinical Tree app for offline access