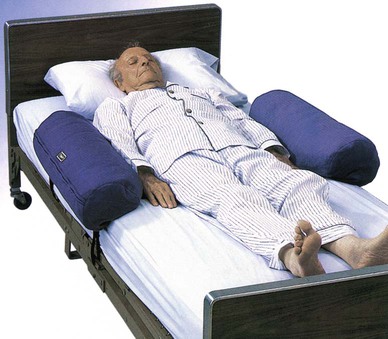
CMS Centers for Medicare & Medicaid Services FDA Food and Drug Administration OBRA Omnibus Budget Reconciliation Act of 1987 • Define the key terms and key abbreviations listed in this chapter. • Describe the purpose of restraints. • Identify restraint alternatives. • Identify the risk factors related to restraint use. • Explain the legal aspects of restraint use. • Explain how to use restraints safely. • Perform the procedure described in this chapter. • Explain how to promote PRIDE in the person, the family, and yourself. Chapters 9 and 10 have many safety measures. However, some persons need extra protection. They may present dangers to themselves or others (including staff). • Physical restraint—any manual method or physical or mechanical device, material, or equipment attached to or near the person’s body that he or she cannot remove easily and that restricts freedom of movement or normal access to one’s body. • Chemical restraint—any drug used for discipline or convenience and not required to treat medical symptoms. The drug or dosage is not a standard treatment for the person’s condition. • Freedom of movement—any change in place or position of the body or any part of the body that the person is able to control. • Remove easily—the manual method, device, material, or equipment used to restrain the person that can be removed intentionally by the person in the same manner it was applied by the staff. For example, the person can put bed rails down, untie a knot, or unclasp a buckle. Restraints also were used to prevent wandering or interfering with treatment. They were often used for confusion, poor judgment, or behavior problems. Older persons were restrained more often than younger persons were. Restraints were viewed as necessary devices to protect a person. However, they can cause serious harm, even death. See “Risks From Restraint Use” on p. 127. • Is the person in pain, ill, or injured? • Is the person short of breath? Are cells getting enough oxygen (Chapter 26)? • Is the person afraid in a new setting? • Does the person need to use the bathroom? • Is clothing or a dressing (Chapter 24) tight or causing other discomfort? • Is the person’s position uncomfortable? • Are body fluids, secretions, or excretions causing skin irritation? • Is the person too hot or too cold? Hungry or thirsty? • What are the person’s life-long habits at this time of day? • Does the person have problems communicating? • Is the person seeing, hearing, or feeling things that are not real (Chapter 29)? • Is the person confused or disoriented (Chapter 30)? Restraint alternatives for the person are identified (Box 11-1). They become part of the care plan. The care plan is changed as needed. Restraint alternatives may not protect the person. The doctor may need to order restraints. See Focus on Surveys: Safe Restraint Use. According to the CMS, physical restraints include these points. • May be any manual method, physical or mechanical device, material, or equipment. • Are attached to or next to the person’s body. • Cannot be easily removed by the person. • Restrict freedom of movement or normal access to one’s body. • A device used with a chair that the person cannot remove easily. The device prevents the person from rising. Trays, tables, bars, and belts are examples (Fig. 11-3). • Any chair that prevents the person from rising. • Any bed or chair placed so close to the wall that the person cannot get out of the bed or chair. • Bed rails (Chapter 10) that prevent the person from getting out of bed. For example, 4 half-length bed rails are raised. They are restraints if the person cannot lower them. • Tucking in or using Velcro to hold a sheet, fabric, or clothing so tightly that freedom of movement is restricted. Drugs or drug dosages are chemical restraints if they: • A chair or wheelchair with a lap-top tray is used for meals, writing, and so on (see Fig. 11-3). The chair is an enabler. If used to limit freedom of movement, the chair is a restraint. • A person chooses to have raised bed rails. The bed rails are used to move in bed and to prevent falling out of bed. The bed rails are enablers, not restraints. Box 11-2 lists the risks from restraints. Injuries can occur as the person tries to get free of the restraint. Injuries also can occur from using the wrong restraint, applying it wrong, or keeping it on too long. Cuts, bruises, and fractures are common. The most serious risk is death from strangulation. Laws applying to restraint use are followed. Remember: • Restraints must protect the person. They are not used for staff convenience or to discipline a person. Using restraints is not easier than properly supervising and observing the person. A restrained person requires more staff time for care, supervision, and observation. • A doctor’s order is required. The doctor gives the reason for the restraint, what body part to restrain, what to use, and how long to use it. This information is on the care plan and your assignment sheet. In an emergency, the nurse can decide to apply restraints before getting a doctor’s order. • The least restrictive method is used. It allows the greatest amount of movement or body access possible. Some restraints attach to the person’s body and to a fixed (non-movable) object. They restrict freedom of movement or body access. Vest, jacket, ankle, wrist, hand, and some belt restraints are examples. Other restraints are near but not directly attached to the person’s body (bed rails or wedge cushions). They do not totally restrict freedom of movement and are less restrictive. • Restraints are used only after other measures fail to protect the person (see Box 11-1). Some people can harm themselves or others. The care plan must include measures to protect the person and prevent harm to others. Many fall prevention measures are restraint alternatives (Chapter 10). • Unnecessary restraint is false imprisonment (Chapter 3). You must clearly understand the reason for the restraint and its risks. If not, politely ask about its use. If you apply an unneeded restraint, you could face false imprisonment charges. • Informed consent is required. The person must understand the reason for the restraint. The person is told how the restraint will help the planned medical treatment. The person is told about the risks of restraint use. If the person cannot give consent, his or her legal representative is given the information. Consent must be given before a restraint can be used. The doctor or nurse provides needed information and obtains the consent. See Focus on Communication: Legal Aspects.
Restraint Alternatives and Safe Restraint Use
Key Abbreviations
History of Restraint Use
Restraint Alternatives
Safe Restraint Use
Physical and Chemical Restraints

Enablers.
Risks From Restraint Use
Legal Aspects