Chapter 59 Multiple pregnancy
The Incidence of Multiple Births
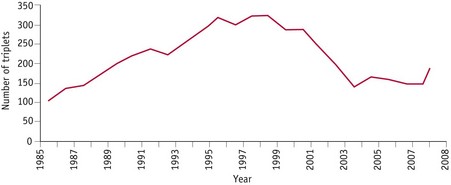
The incidence of multiple births continues to rise, mainly because of the increased availability of treatments for infertility (Kurinczuk 2006). A decline in the 1970s was followed by a rise from the early 1980s onwards (Fig. 59.1) (MacFarlane & Mugford 2000). In the UK, the multiple birth rate in 2008 was 15.48 per thousand maternities (Fig. 59.2). A total of 11,573 sets of twins and 149 sets of triplets were born (Fig. 59.3).
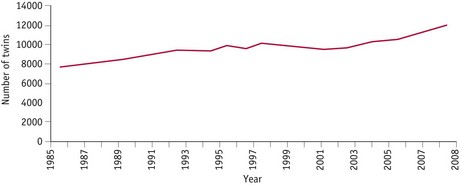
Figure 59.1 Twinning rate in UK 1985–2008.
(Source: ONS London, GRO Northern Ireland and GRO Scotland.)
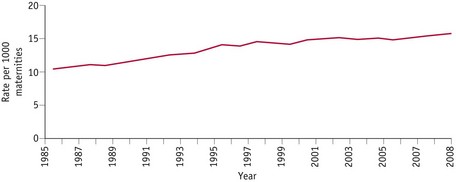
Figure 59.2 Multiple births in England and Wales, 1985–2008.
(Source: ONS, Birth Statistics, Series FM1.)
Multiple pregnancies carry higher risks for the mothers and babies, and can impose a greater burden practically, financially and emotionally on the parents (Botting et al 1990) and also on neonatal services (Collins & Graves 2000).
If a dead fetus is delivered with a live birth after 24 weeks’ gestation, it should be registered as a stillbirth even if death occurred much earlier in the pregnancy (MacFarlane & Mugford 2000).
Facts about multiples
How twins arise
There are two types of twins: monozygotic and dizygotic.
Causes of twinning
The cause of monozygotic twinning is unknown, but recent reports suggest that slightly more are born after the use of drugs to stimulate ovulation and assisted conception procedures. The incidence of MZ twins throughout the world was approximately 3.5–4 per 1000 until the recent slight rise which may be associated with fertility treatments (Derom et al 2001).
Dizygotic twinning is different as there are several known associated factors (Chitayat & Hall 2006): maternal age, parity, race, maternal height and weight, and infertility treatments.
Determination of zygosity
Placentation
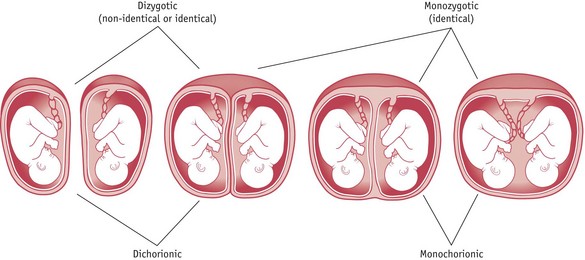
There can be two separate placentas (dichorionic) or a single placenta (monochorionic), which can sometimes be fused (dichorionic) (Fig. 59.4). All dizygous twins have dichorionic (two chorions) and diamniotic (two amnions) placentas (DCDA).
Importance of chorionicity
When a twin pregnancy is diagnosed on ultrasound scan, an assessment of the chorionicity should be made (preferably during the first trimester) by measuring the thickness of the dividing membranes (Fisk & Bryan 1993). Nearly all monochorionic placentas have blood vessels linking the placenta together. As long as the bloodflow can pass in both directions, there will not be a problem; however, if anastomoses occur between an artery and a vein, causing the blood to flow in one direction only, twin-to-twin transfusion syndrome is likely to occur. This happens in approximately 15% of MCDA twins.
Diagnosis of a multiple pregnancy
Antenatal preparation
At whatever stage parents are told, it is essential that whoever shares the news is aware of the effect the revelation may have. Although some mothers and fathers are delighted to know that more than one baby is expected, in many cases there are reactions of shock and disbelief (Spillman 1986). It is important that an obstetrician or midwife is available to answer questions and give appropriate counselling at this time. It is helpful if the mother can be put in touch with other parents of twins who can understand and provide reassurance. Contact numbers for local twins groups and information about other relevant support organizations can be a great source of reassurance (see website).
Parent education
Routine parentcraft classes need to be booked as early as possible; ideally, the mother should commence these at 24 weeks’ gestation, which is earlier than for a singleton pregnancy, or specialist multiple pregnancy classes at 28 weeks (Davies 1995). When planning classes, contact with the local twins club can provide a very useful source of practical information. Mothers from twins clubs are usually delighted to participate and offer practical information, such as on equipment, clothes and breastfeeding (Denton & Bryan 1995).
Preparation for breastfeeding
Mothers expecting twins or triplets will inevitably give a lot of thought to how they are going to feed their babies, not only from the nutritional aspect but also from the practical one because feeding will take a large part of the first months. Mothers should be encouraged that breastfeeding not only is possible for two babies and in some cases three (Fuducia 1995), but can be a very rewarding experience for all. Breast milk is ideal for all babies and especially important because twins, and more so triplets, tend to be born prematurely and of low birthweight.
Early in the pregnancy the mother should be given as much information about breastfeeding as possible, with contact numbers of local breastfeeding organizations. Both parents should have the chance to talk through any issues; a good idea is to suggest they meet with another mother who is successfully breastfeeding twins (see Davies & Denton 1999).