Chapter 27 Fertility and its control
After reading this chapter, you will be able to:
Worldwide, 1 in 5 pregnancies end in abortion. In England and Wales in 2006 the abortion rate rose to 18.3 per 1000 women aged 15 to 44, with rates varying from 3.9 for the under 16 years to 35 for 19-year-olds (DH 2007). Britain has one of the highest rates for teenage pregnancies in Europe, with 90,000 teenagers becoming pregnant every year, 8000 being under 16 years old. The Government teenage pregnancy strategy has aimed to halve this number by 2010 (Social Exclusion Unit 1999), though indications suggest that this target will not be achieved.
Resuming relationships following childbearing
Women vary in their approach to resuming marital relations after childbirth and it is common for newly delivered mothers to feel extremely tired and also guilty about their reluctance to have sexual intercourse. For the man, the effects of witnessing a delivery can be a highly emotional experience and may result in tension or guilt (Clement 1998), but problems of changed sexual relationships are often regarded as the fault of the woman. The man may feel rejected when the baby is establishing a relationship with its mother, and mothers experiencing postnatal depression may find their satisfaction with the relationship with their partner is reduced. This, in turn, may increase the man’s guilt and frustration. Women have far better opportunities than men for obtaining advice on these intimate matters, so it is important that the midwife takes the time to provide opportunities for counselling or, where necessary, referral to specialist counsellors.
Methods of contraception
Male contraception
Condom or sheath
The condom or sheath is probably the most widely used contraception in the first few months after childbirth. As a barrier method, it not only provides protection against conception but also is effective in preventing the transmission of sexually transmitted diseases, including HIV (Everett 2004). For this reason, many couples use this in addition to other methods and the regular use of condoms should be encouraged as part of the promotion of safer sex. Condoms, however, cannot protect against local infestations such as scabies and lice. Because of the strong links between specific types of the human papillomavirus (HPV) and cervical cancer (Guillebaud 2007), it is reasonable to assume that condoms may reduce the risk of cervical neoplasm.
In the UK, condoms can be obtained free from family planning clinics and Department of Sexual Health clinics, or purchased at chemists or other retail outlets, with a wide variety of sizes, textures and flavours being available. Condoms should no longer be used if lubricated with spermicide, as this is thought to increase the risk of HIV transmission (Guillebaud 2007). Most condoms are made from latex. Occasionally, men and women report sensitivity to the latex, and condoms made from a hypoallergenic latex can be tried. Rarely, an allergy to the latex occurs; the Avanti condom, which is made from polyurethane, can be used in these situations. A new condom, called Ez.on, is also made from polyurethane and is slightly different in shape to conventional ones, with a tight base but a looser-fitting shaft, thus theoretically making it less likely to break and allowing more sensation for the man.
Future developments
Male hormonal contraception is presently under research. Current trials are mainly using progestogens that inhibit production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH), thus reducing sperm production, with testosterone replacement needed to prevent side-effects. Other trials are using androgen, which induces sperm suppression (Herdiman et al 2006). The aim is to prevent sperm production whilst having no effect on ejaculation. Apart from the effectiveness of this type of contraception, there is the issue of whether women would be happy to rely on their male partner for contraception of this type.
Female contraception
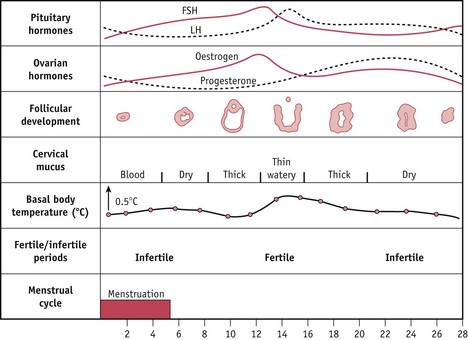
Physiological methods (Fig. 27.1)
Lactational amenorrhoea method (LAM)
If any of the criteria change, the mother is potentially fertile. It is estimated that this method has a failure rate of 2% (Guillebaud 2007).
Persona
Persona may be of limited value following childbirth, as it requires the woman to have two successive cycles of 23–35 days and this makes it inappropriate for use in breastfeeding mothers. With perfect use, the failure rate of Persona as a contraceptive tool is 6 per 100 woman years; however, for the typical user the rate is higher (Guillebaud 2007). Persona can be used for planning a pregnancy but there are few references to the efficacy of Persona used for this purpose.
Barrier methods
Occlusive caps
These devices cover the cervix and mechanically obstruct the entrance of spermatozoa.
They are made in a variety of sizes and must be fitted individually. Caps are checked for fit at regular intervals, especially after childbirth or loss or gain of weight. With correct and conscientious use, the rate of pregnancy can be as low as 2 per 100 woman years, but a more typical rate would be 5–10 per 100 women years (Guillebaud 2007). Cervical caps are less effective as a contraceptive in multiparous women.
The diaphragm or Dutch cap
This is one of the oldest methods of female contraception and has changed very little in design. A postnatal mother who wishes to use a diaphragm should not be fitted until 6–8 weeks postnatally, to allow the uterus and cervix to return to a non-pregnant size and the vaginal muscles to regain their tone. The shallow rubber diaphragm has a circular spring around the perimeter, allowing it to be compressed and inserted into the vagina rather like a tampon, with the diaphragm lying between the posterior fornix of the vagina posteriorly and the suprapubic ridge anteriorly (Fig. 27.2). The diaphragms come in graduated sizes and must be fitted individually.