Chapter 12. Physical growth and development in children
Janet Kelsey and Gill McEwing
LEARNING OUTCOMES
• Define growth and development and understand how they can be assessed.
• Demonstrate an understanding of the anatomy and physiology of the newborn baby.
• Gain an overview of the development of the child from birth to adolescence.
• Be aware of the importance of assessing child development and the detection of deviations from normal.
Introduction
The physical development of the child is only one aspect of its whole development, which includes cognitive, social and emotional elements. Inherited attributes and environmental factors will affect physical development. These factors interact to cause effects on the child’s development from conception to adulthood.
Babies and children vary considerably in exactly when and in what way they progress in all areas of development. It is not always appropriate to assign exact ages in months and years to stages of development, although an approximate age range is possible.
 Activity
Activity
 Activity
Activity• Write down what you think is meant by the terms ‘growth’ and ‘development’.
• Why might it be important to you as a nurse to have some understanding of the growth and development of children?
Factors affecting growth and development
• Genetic/chromosomal factors: inherited rate of growth and individual differences
• Racial factors
• Endocrine system
• Drugs
• Illness: children grow more slowly during periods of illness but there might be increased growth to catch up after recovery
• Nutrition: poorly nourished children grow more slowly and do not reach their full potential size; malnutrition can have a permanent effect on some parts of the brain and nervous system
• Environment: the ability to practise skills, e.g. crawling, walking.
Other factors also govern growth and physical changes. Hormones are the most important of these (Table 12.1).
| Gland | Hormone | Aspects of growth |
|---|---|---|
| Thyroid | Thyroxine | Normal brain development and overall rate of growth |
| Adrenal | Adrenal androgen | Involved in some changes at puberty, particularly the development of secondary sex characteristics in girls |
| Testes | Testosterone | Formation of male genitals before birth. Also triggers the sequence of changes in primary and secondary sex characteristics at puberty in the male |
| Ovaries | Oestradiol | Development of the menstrual cycle and breasts in girls. Less important than testosterone for secondary sex characteristics in boys |
| Pituitary | Growth hormone activating hormone | Rate of physical maturation. Signals other glands to secrete hormones |
Physical growth
Physical growth and maturation is important for child development. Maturation is the:
… universal sequence of biological events occurring in the body and the brain that permits psychological function to appear, provided that the infant is healthy and lives in an environment containing people and objects
(Mussen et al 1990)
Growth is defined as an increase in the size of and number of cells that results in an increase in size and weight of the whole, or any of its parts. In clinical practice, growth of the infant is generally measured by estimating the weight, length, head circumference and, in certain circumstances, skin-fold thickness.
Pattern of growth
The most obvious thing about children’s physical development is that they get bigger as they get older. Growth proceeds in a continuous pattern but is not smooth; the most rapid growth takes place in utero, the first 2 years of life and during adolescence (Fig. 12.1). However, acceleration and deceleration occur in response to illness and changes in nutrition or environment. As Figure 12.1 shows, infants grow very quickly in the first year of life, adding 25–30 cm to their height.
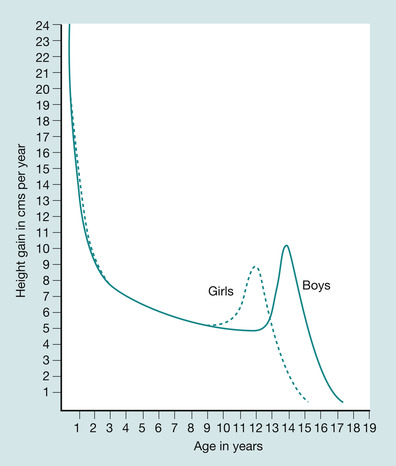 |
| Fig. 12.1 Rates of growth (adapted from Bee 1997). |
Children gain weight at an equally rapid rate, doubling birth weight by the age of 5–6 months and tripling it by the end of the first year. The birth size of a normal infant is determined by the mother. Inherited factors, however, are one of the greatest influences affecting the final stature of the child. Although children tend to attain a stature between those of their parents, some children take after one parent, a grandparent or even a more remote member of the family.
Measuring growth
Length/height
An infant’s recumbent length is measured supine on a measuring board, placing the head firmly at the top of the board and the heels of the feet at the foot-board (Fig. 12.2 and Fig. 12.3).
 Classic clues
Classic clues
height
 Classic clues
Classic cluesheight
The height of an infant increases by around 12 cm during the first 6 months of life. By the age of 1 year, the height has increased by almost 50% and by the age of 2 years an infant is about half as tall as he or she will be as an adult (Bee 1997). There is a rapid increase in size during the first 2 years, which then settles down to a slower and steadier rate: 5–7.5 cm in height per year and 3 kg in weight per year. Adolescence then brings a ‘growth spurt’, following which height and weight are slowly gained until adult size is achieved.
 |
| Fig. 12.2 Infant length. |
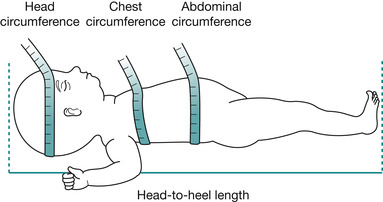 |
| Fig. 12.3 Measurement of the head, chest, abdominal circumference and the recumbent length. |
Height is the measurement taken when children are measured upright. Shoes should be removed and the child should stand as tall and straight as possible with the head in mid-line and the line of vision parallel to the floor. The most accurate measurement of height is gained by using a wall-mounted stadiometer (Fig. 12.4). It might be useful to remember that the height will be less when measured in the afternoon than in the morning. This effect can be reduced by applying modest upward pressure under the jaw or mastoid process.
 Classic clues
Classic clues
weight
 Classic clues
Classic cluesweight
On average an infant gains 600–800 g in weight per month. An infant’s weight at 6 months will therefore be almost double the birth weight. By the first year of life, weight has tripled.
 |
| Fig. 12.4 Child height. |
Weight
Infants should be weighed naked and preferably at the same time of the day. Older children can be weighed in light clothing without their shoes (Fig. 12.5).
 |
| Fig. 12.5 Child weight. |
Head circumference
This measurement is important because the size of the skull is closely related to the size of the brain. It is usually recorded in children who are under 3 years of age or in cases where the growth of the brain/skull is under observation. It is advisable to use a paper disposable tape measure for this measurement as linen tape measures stretch and produce inaccurate results (Hockenberry et al 2003). The head should be measured around the point of greatest circumference, this is usually slightly above the eyebrows and pinna of the ears and around the occipital prominence at the back of the skull.
 Classic clues
Classic clues
head circumference
 Classic clues
Classic clueshead circumference
The head growth of an infant is rapid. In the first 6 months the circumference increases by between 8 and 9 cm. By the first year there is an increase of 33% in the overall size of the head.
Surface area
The child’s surface area can be calculated once the height and weight of the child is known using the body surface area nomogram. This measurement is important for the prescription of some drugs.
 Activity
Activity
 Activity
ActivityFind a copy of the body surface area nomogram and calculate the body surface area for:
• a newborn weighing 3 kg and 50 cm in length
• a 6-year-old child weighing 20 kg and with a height of 115 cm.
Skinfold thickness
Skinfold thickness is a quick and easy method of measuring subcutaneous fat that allows for the estimation of an individual’s body fat. The most common site for measuring skinfold thickness is the triceps; others include the subscapula, suprailiac, abdomen and upper thigh. The measurement is made by pinching the skin between two fingers and measuring the skinfold thickness using specially designed callipers (Fig. 12.6).
 |
| Fig. 12.6 Skinfold thickness. |
Bone age
Bone age is a method of measuring skeletal maturity; the appearance of the epiphyseal centres is compared with standard charts. This is best achieved using the child’s left wrist and hand, where the 20 bones can be judged against that recognised as the normal pattern of development.
 Activity
Activity
 www
www
 Activity
ActivityTwo groups of factors that strongly influence normal growth and development are heredity and environment. From your observations of children, give two examples from each group.
 www
wwwGo to:
Search for and read the growth reference charts, paying attention to the recommendations of the expert consensus group on the use of growth reference charts in the UK.
Assessment of growth
Centile charts have been developed using statistics of children’s growth patterns. They give estimations of expected height, weight and head circumference for boys and girls at different ages. An infant usually has a similar centile at birth for head circumference and weight. Children of large parents tend to be towards the 90th centile and those of small parents tend towards the 10th, most will remain on these centiles for the rest of their lives. A common problem in the paediatric outpatient department is short parents who think that their child is not growing as expected because he or she is not as big as their peers. Plotting growth measurements confirms that the child’s growth is normal and that the child’s final size will be similar to that of the parents.
 Activity
Activity
 Activity
Activity
 Activity
ActivityPercentile charts provide a useful measure of normal growth. Different charts are available for boys and girls, for different age groups and for different cultures. Children may need to be assessed if they are above the 97th or below the 3rd centile. Some show height and weight measurements only, whereas others also show head circumference. To ensure that you understand the format of a percentile chart, look at a chart in your practice area and answer the following questions:
• What sex, age and measurements does it cover?
• Which percentiles does it show?
• Where on the chart would you find a child of abnormal growth?
• If Helen is 3.5 years and 98 cm tall, which percentile is she on?
• How many children fall below the 50th centile and how many above?
• John is on the 90th centile. Is he above or below the average for his age?
 Activity
ActivityPlot the following weight, height/length and head circumferences on to growth charts from your practice area.
| John (male) | |||
| Age | Weight (kg) | Head (cm) | Length (cm) |
| Birth (40 weeks) | 3.5 | 34 | 51 |
| 6 weeks | 5 | 38 | 56 |
| 20 weeks | 7.25 | 42 | 66 |
| 36 weeks | 9.75 | 46 | 72 |
| Rebecca (female) | |||
| Age | Weight (kg) | Head (cm) | Length (cm) |
| Birth (37 weeks) | 2.6 | 34 | 50 |
| 4 weeks | 4 | 36 | 52 |
| 12 weeks | 6.25 | 41 | 61 |
| 40 weeks | 9.25 | 44.25 | 68 |
Some children resemble one parent more than the other in final size. If only their weights are recorded, they may appear to have faltering growth if father is small, or gaining weight excessively if father is tall. If weight is plotted against head circumference then they can be seen to be running in parallel, i.e. the whole of the child’s size is approaching that of a particular parent.
Growth charts give an early warning of some problems, such as obesity, which will be indicated by the child’s weight starting to deviate upwards even though the head circumference remains on the same centile.
Changes in shape and proportion
After 2 years, the rate of growth slows down and the child gains approximately 2.7 kg in weight each year until adolescence. Changes in proportion and shape take place at the same time. An adult’s head is an eighth of his total height but in a 2-year-old the head is a quarter of the total body length. In addition to this, a 2-year-old has a large body and shorter legs in proportion to that of an adult (Bee 1997).
If a child is growing and his or her shape is altering then there must be changes occurring in the child’s bones, muscles and fat. Bones increase in number, become longer and grow harder. Although bones are not all formed at birth, the newborn baby has virtually all the muscle fibres that will ever be needed. As a child grows, the muscle fibres get longer, thicker and less watery.
Development
According to the Penguin dictionary (Allan 2001), the definition of development is ‘to bring out the possibilities of something, to acquire gradually’. It is the sequence of organic changes by which the fertilised ovum becomes the mature human being. An increase in complexity of the individual involves structure and function; the emerging of an individual’s capacities through learning, growth and maturation. Maturation can be defined as an increase in competence and adaptability; a change in the complexity of a structure that makes it possible for that structure to work. Many of the debates about child development have centred on the nature versus nurture controversy. The former believe that human behaviour is guided by inborn factors and argues that differences are a result of heredity. Those who err towards nurture stress the importance of acknowledging the influence of a child’s physical and social environment. According to them, individual differences are a result of the child’s life experiences. The reality is probably somewhere in between. What is certain is that development is a complex process in which many variables play a part. We as nurses need to assess each child on an individual basis.
Measuring development
Development is measured using developmental scales. It is divided into four major areas:
1. Physical: growth, vision, hearing, locomotion, coordination.
2. Cognitive: language and understanding.
3. Psychosocial: adapting to the society and culture to which the child belongs.
4. Emotional: control of feelings and emotions.
As with growth we need to have some idea of what is the norm. The charts by Sheridan (1997) and Frankenburg & Dodds (1967) (the Denver Developmental Screening Test) were developed to show what can be expected at key stages of development. Sheridan (1997) is a little didactic, she herself suggested that her charts should be used only by experienced professionals. The Denver scale is a little more flexible, allowing the assessor to accommodate the individuality of the child, although it is suggested that the user should be trained in the use of the scale.
Differences in rate
There may be individual differences in the rate and timing of developmental progress, e.g. three perfectly normal infants may sit unaided at 5, 6 or 9 months. However, the sequence of developmental progress is always the same. A child may be consistently early, average or slow in development, e.g. a child whose bone development is slower probably walks later and eventually reaches puberty later.
The development of walking can be used to illustrate the factors that influence growth and development (Bee 1997):
• Newborn infants held with the sole of the foot on a table move their legs in a reflex walking action.
• By 8 weeks: infants briefly hold their head up if held in a standing posture.
• At 36 weeks: infants pull themselves up and remain standing by grasping furniture.
• At 48 weeks: infants walk forwards if both hands are held, or sideways if holding furniture.
• By 52 weeks: infants walk forwards if held by one hand.
• At 13 months: infants walk without help.
Factors required for the development of walking
A complex set of changes occurs in the muscles, bones, and nervous system:
• Nutrition: for growth
• Environment: in which to practice walking
• Genetics: were the parents early walkers?
The child’s ability to walk (or not) will also affect other areas of development such as social, emotional and intellectual.
 Activity
Activity
 Activity
ActivityFrom your experience of your own childhood, can you think of areas where the rate and timing of the development for certain skills was different between yourself and others. Make some notes about your ideas.
Developmental assessment
In the main, developmental assessments are performed by the child’s health visitor and GP, although there might be occasions when a paediatrician will also perform them. These assessments include the evaluation of:
• locomotion or gross motor development referring to large muscle skills
• fine motor or manipulation skills: referring to small muscle skills
• hearing and speech
• vision
• social development, e.g. feeding, dressing and social behaviour.
To assess deviations from normal, it is first necessary to know about normal development. The development of a child between the ages of 0 and 18 months is very complex. These are the major milestones and their approximate age of appearance:
 Activity
Activity
• smile: 1–2 months
• laugh: 6 months
• sits (without support): 8–9 months
• crawls: 8–9 months
• stands/walks: 12 months
• pincer grip: 12 months
• delicate pincer: 18 months
• walks backwards: 18 months.
 Activity
ActivityWatch a video showing different aspects of child development, find one at your university library or your local health promotion centre.
All aspects of development are interlinked. Skills are acquired sequentially; an example of this is the sequence of development of motor skills, which is often described as cephalocaudal, i.e. head (cephalo) to toe via the spine (caudal). So, initially, head control is developed before the baby is able to sit independently; this is followed by crawling and finally by control of the lower limbs for standing and walking. Each new skill usually appears at the most appropriate time to make use of information coming in to carry out activities to prepare for the next stage (Table 12.2).
| Skill | Information | Activity | Next stage |
|---|---|---|---|
| Drawing | Holding pencil | Drawing | Writing |
| Running | Spatial awareness | Running | Football, dancing |
It is important to know about child development to:
• teach and advise parents
• have reasonable expectations of the child
• be able to plan suitable activities and play
• be able to identify limits and capabilities
• be able to recognise deviations from the norm and be alert to regression (behaviour from an earlier stage of development), disability and abnormality.
Transition from intrauterine to extrauterine life
This demands considerable effective physiological changes by the baby to ensure survival. Simultaneously, he or she has to make major adjustments in his or her respiratory and circulatory systems, as well as gaining control of his or her body temperature. The baby emerges to encounter, light, noise, cool air, gravity and tactile stimuli. Adaptation to extrauterine life involves the onset of respiration, circulatory changes and thermal adaptation.
Onset of respiration
Regular respirations begin 60–90 seconds after complete expulsion from the mother as a result of both chemical and thermal stimulation. Thermal stimulation is caused by the sudden cooling of the infant leaving the warm environment of the uterus (37.7°C) and entering the cold atmosphere of the outside environment (approximately 21°C). This cooling excites sensory impulses in the skin that are transmitted to the respiratory centre. In addition, low levels of oxygen, high levels of carbon dioxide and low pH initiate impulses that excite the respiratory centre. At term, approximately 100 mL lung fluid is present within the respiratory tract. Some fluid is expelled through the mouth, assisted by the pressure on the thorax during vaginal delivery; the remainder is absorbed via the pulmonary lymphatics during the first 24 hours of life. The first breath requires a large pressure to open the terminal airways and overcome the initial stiffness of the lungs.
Circulatory changes
Separated from the placenta, the infant must make major adjustments within the circulatory system to divert deoxygenated blood to the lungs for reoxygenation. The transition from fetal to postnatal circulation involves the closure of the foramen ovale, the ductus arteriosus and the ductus venosus.
Fetal blood pressure (BP) is low as a result of low vascular resistance in the placental circuit. A systolic BP of around 76 mmHg is found at birth; this level rises to 96 mmHg by 4 weeks. Coughing, crying and straining raise the BP.
The newborn baby
Measurements
The average measurements at the 50th centile are shown in Table 12.3. The weight of the infant at birth also correlates with the incidence of perinatal morbidity and mortality. At birth, head circumference head is usually 2–3 cm greater than the circumference of the chest.
| Girls | Boys | |
|---|---|---|
| Weight on 50th centile | 3.4 kg | 3.5 kg |
| Length on 50th centile | 50 cm | 51 cm |
| Occipitofrontal circumference on 50th centile | 34.5 cm | 35 cm |
Appearance
• Plump.
• Prominent abdomen.
• Lies in an attitude of flexion.
The skin
The skin has a film of vernix caseosa – a white sticky substance that is absorbed within a few hours and thought to have a protective function. The skin is thin and delicate; it is prone to blistering, infection and excoriation. Lanugo (downy hair) covers the skin and is plentiful over the shoulders, upper arms and thighs. Colour depends on ethnic origin.
Sebaceous glands are active late in fetal life and early infancy because of the high levels of maternal androgens. Plugging of the sebaceous glands causes milia. The epidermis and dermis are loosely bound to each other and very thin; friction such as removing sticky tape can separate the layers and cause blistering. The eccrine sweat glands (found mainly on the palms of the hands and the soles of the feet and forehead) are functional at birth and respond to heat and emotional stimulus. By the age of 43 weeks, palmar sweating can be used in pain assessment. The mature baby has many skin creases on its palms and soles; the nails are fully formed and adhere to the fingertips. Melanin levels are low at birth therefore the skin of the newborn is lighter than that it will be as a child, which means that young babies are more susceptible to the harmful effects of the sun. The hair is soft and silky; there may be lots or nearly none. The same is true for the eyebrows. The cartilage of the ears is well formed. The cord stump necroses and falls off within the first 10 days of life.
Genitalia and breasts
In both sexes the breasts may be enlarged in the period immediately after birth. They may also discharge clear fluid. This is due to the stimulation caused by maternal hormones; these effects subside in the first few weeks of extrauterine life (MacGregor 2000). There are nodules of breast tissue around the nipple. The testes are descended and the scrotum has plenty of rugae, the prepuce is adherent to the glans penis. The labia majora cover the labia minora.
Thermoregulation
Heat regulation is critical to the newborn baby’s survival. The baby’s capacity for heat production is adequate but several factors predispose to excessive heat loss. The newborn’s large surface area increases the possibility of heat loss to the environment, although this is normally partially compensated for by their position flexion, which effectively decreases the amount of surface area exposed to the environment. The subcutaneous fat layer is thin, giving poor insulation. This also allows transfer of core heat to the environment and cooling of blood. The hypothalamus in the brain has the capacity to promote heat production in response to stimuli received to thermoreceptors. Babies cannot shiver, nor are they able to voluntarily increase muscle activity to generate heat. Infants do produce heat by non-shivering thermogenesis and that generated by the heart, liver, brain and skeletal muscles.
Noradrenaline (norephinephrine) is secreted by the sympathetic nerve endings in response to chilling and stimulates fat metabolism in brown adipose tissue (BAT); this is unique to the newborn baby. BAT has a greater capacity for heat production through intensified metabolic activity than ordinary adipose tissue. BAT is situated between the scapulae, around the neck, in the axilla, behind the sternum, and around the kidneys, trachea, oesophagus, adrenal glands and some arteries. However, this process does require energy, so the infant’s oxygen requirement will increase. The regeneration of this tissue also requires good nutrition; a poor calorie intake will mean that the brown fat is not replaced and the infant will be less able to maintain body heat in a cool environment. Healthy, clothed infants will maintain their temperature provided the environmental temperature is maintained between 18°C and 20°C, nutrition is adequate and movements are not restricted. The temperature of the newborn is 37.5°C and by the age of 13 years it has reduced to 36.6°C; this is because infants produce more heat per kilogram body weight than older children. The temperature regulatory system is immature in the newborn infant, rendering infants and small children susceptible to temperature fluctuations. Factors such as environmental temperature, increased activity, crying or infection can cause a rapid increase in body temperature in the infant.
Eyes
At birth, the eyeball is too short for its lens therefore babies focus best at approximately 20 cm (Fig. 12.8). As the eyeball continues to grow, distance vision is achieved. The ciliary muscles are immature, limiting the ability of the eyes to accommodate and fixate for any length of time. Babies have been shown to demonstrate visual preferences for some colours rather than others. No tears are present and eyes are easily infected. Corneal, papillary and blink reflexes are present.
 |
| Fig. 12.8 The eyes. |
Hearing
Once the amniotic fluid is drained from the external ear canal the acuity is similar to that of an adult. Babies can detect pitch, loudness and timbre of sound in addition to location and changes in complex sounds. The internal and middle ear is larger in proportion at birth and the external canal small. The mastoid process and the bony part of the external canal have not yet developed. The tympanic membrane and facial nerve are close to the surface and easily damaged.
Respiratory system
The respiratory system is developmentally incomplete. The lungs mature after birth and new alveoli continue to grow for many years. There are 20 million alveoli at birth, increasing to 300 million alveoli in the fully formed lungs of the adult (Meadow & Newell 2002). This means that infants and young children have a relatively small alveolar surface area for gaseous exchange. Airway resistance in children is high due to the small diameter of the respiratory tree. The lumen of the peripheral airways is narrow, which predisposes the infant to airway obstruction. The infant’s breathing is mainly abdominal: the abdomen distends, the diaphragm contracts and the thorax expands. The chest wall is very compliant and therefore easily distorted, which can increase the work of respiration.
Babies are obligatory nose breathers and do not convert automatically to mouth breathing when nasal obstruction occurs. Respiratory rate is 30–60 per minute. Respirations are shallow and the pattern alters during sleeping and waking. Many term babies have periods of rapid breathing alternating with periods of breathing at a slower rate, or they may not breathe for periods of up to 15 seconds – this is normal as long as the colour and heart rate do not change significantly and the infant then begins to breathe again spontaneously (MacGregor 2000). Periods of apnoea, when breathing ceases for more than 20 seconds, are only common in babies under 32 weeks’ gestation unless there is an underlying condition.
Cardiovascular system
The heart rate is roughly 120–160 beats per minute and fluctuates with respiratory function, activity and sleep. It reaches a maximum at month, after which there is a gradual slowing until adult levels at 12–16 years of age. Peripheral circulation is sluggish and there may be mild cyanosis of hands and feet with mottling of skin when exposed.
Normal blood pressure ranges between 50/25 and 70/40 mmHg. The amount of total circulating blood is 80 mL/kg or approximately 300 mL at birth. Haemoglobin (Hb) = 15–20 g/dL; 70% is fetal Hb, which is replaced by adult Hb in the first 2 years of life. Mean cell volume (MCV)/100 L = 135 femtolitres = 10 −12 g.
Breakdown of excess red blood cells in the liver and spleen predisposes to jaundice in the first few weeks. Prothrombin levels are low due to a lack of vitamin K. Colonisation of the intestine promotes synthesis of vitamin K. The white cell count is initially 18 × 10 9/L and reduces rapidly. Cardiac output is related to the heart rate and the stroke volume; as children have smaller hearts the stroke volume is reduced. The heart then needs to beat faster in order to oxygenate their body tissues.
Renal system
The newborn baby’s kidneys weigh 23 g; this will have doubled by 6 months and trebled by the end of the first year (Sinclair 1991, cited in MacGregor 2000). The renal system is functional before birth but the workload is minimal. The infant is not able to concentrate or dilute urine very well in response to variations in fluid intake, and cannot compensate well for high or low solutes in blood. The ability to excrete drugs is also limited. However, the newborn can excrete amino acids and conserve sodium and glucose. The glomeruli are immature; they are resistant to aldosterone, which results in limited ability to concentrate the urine. This lack of ability to conserve or excrete water makes the baby vulnerable to dehydration. The glomerular filtration rate is 30 mL/min/m 2 at birth, 100 mL/min/m 2 at 9 months, and reaches adult values at year (Davenport 1996, cited in MacGregor 2000). Dehydration, hypotension and hypoxaemia all produce a fall in glomerular filtration rate, so renal function becomes compromised very quickly in a crisis. Urine is voided by reflex emptying of the bladder. The first urine is passed either at birth or during the first 24 hours and then increases in frequency as the fluid intake increases. The specific gravity should be 1.020. After birth, the kidneys increase in size in proportion to body length, the weight doubling in the first 10 months as a result of tubular growth.
Endocrine system
The endocrine system produces limited quantities of antidiuretic hormone from the posterior pituitary gland, thus making the infant more susceptible to dehydration. The effect of maternal hormones may cause the labia to be hypertrophied and the breasts engorged.
Gastrointestinal system
This system is structurally complete but functionally immature. The teeth are usually still buried in the gums. Sucking pads in the cheeks give them a full appearance. Sucking and swallowing reflexes are coordinated.
The stomach’s capacity at birth is approximately 10–20 mL, although this increases rapidly in the first few weeks of life up to 150 mL by 1 month. The cardiac sphincter is weak, making the baby prone to regurgitation or possiting and gastric emptying time is 2.5–3 hours. Hydrochloric acid is present in the stomach at birth but, due to swallowing of amniotic fluid, the pH is nearly neutral. Acid secretion commences within 8 hours of birth and digestion in the stomach is then reliant on the action of hydrochloric acid and rennin to cause the formation of curds by coagulating the casein in milk. Human milk contains e-fructose, a bacterium that raises the acidity of the gut inhibiting the growth of Escherichia coli bacteria. Adult levels of acid secretion are reached by the age of 10 years.
Get Clinical Tree app for offline access




