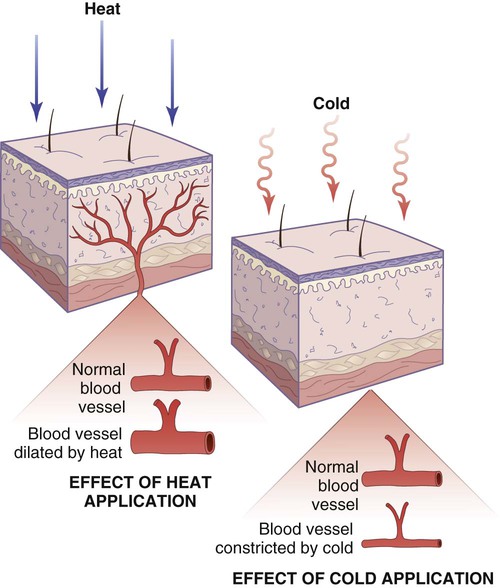
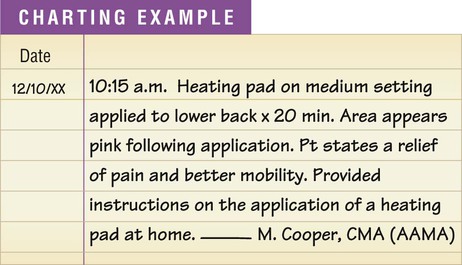
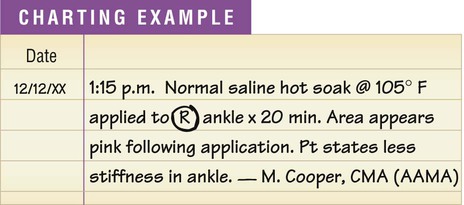
1. Dry heat: heating pad, chemical hot pack 2. Moist heat: hot soak, hot compress 3. Dry cold: ice bag, chemical cold pack 1. The age of the patient. Young children and elderly patients tend to be more sensitive to the application of heat or cold. 2. Location of the application. Certain areas of the body are more sensitive to the application of heat or cold, especially thin areas of the skin and areas that are usually covered by clothing, such as the chest, back, and abdomen. The skin on the hands and face is not as sensitive and is better able to tolerate temperature change. Broken skin, such as is found with an open wound, is more sensitive to heat and cold and is more prone to tissue damage. 3. Impaired circulation. Patients with impaired circulation tend to be more sensitive to heat and cold. This impairment may be at the site of the application or may be a systemic problem involving the entire body that is a result of certain conditions, such as peripheral vascular disease, diabetes mellitus, or congestive heart failure. 4. Impaired sensation. Patients with impaired sensation, such as diabetic patients, must be watched carefully because tissue damage may occur from the application of heat or cold without the patient’s awareness. 5. Individual tolerance to change in temperature. Some individuals cannot tolerate temperature change as easily as others. The application of moderate heat to a localized area of the body for a short time (approximately 15 to 30 minutes) produces dilation, or an increase in diameter, of the blood vessels in the area as the body tries to rid itself of excess heat (Figure 22-1). This results in an increased blood supply to the area, and tissue metabolism increases. Nutrients and oxygen are provided to the cells at a faster rate, and wastes and toxins are carried away faster. The skin in the area becomes warm and exhibits erythema. Erythema is reddening of the skin caused by dilation of superficial blood vessels in the skin. Procedures 22-1, 22-2, 22-3, and 22-6 (see later) present the proper application of heat with a heating pad, a hot soak, a hot compress, and a chemical hot pack.
Physical Agents to Promote Tissue Healing
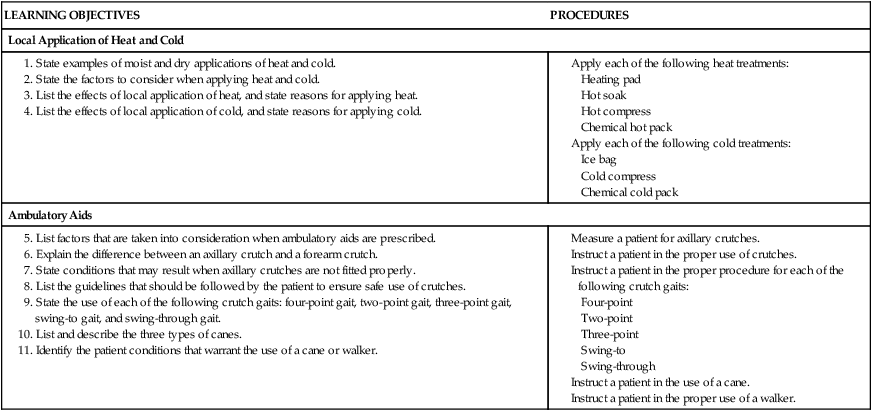
Introduction to Tissue Healing
Local Application of Heat and Cold
Factors Affecting the Application of Heat and Cold
Heat
Local Effects of Heat
Types of Heat Applications
Chemical Hot Pack

Physical Agents to Promote Tissue Healing
Get Clinical Tree app for offline access