Describe the etiology of infertility.
 Describe the drugs used for infertility.
Describe the drugs used for infertility.
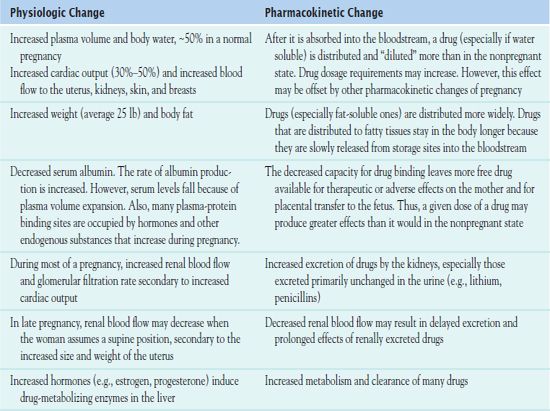
 Identify the pregnancy-associated changes that affect drug pharmacokinetics.
Identify the pregnancy-associated changes that affect drug pharmacokinetics.
 Analyze the effect of teratogens on the fetus during development.
Analyze the effect of teratogens on the fetus during development.
 Identify the Effects of herbal and dietary supplements on the mother and fetus during pregnancy.
Identify the Effects of herbal and dietary supplements on the mother and fetus during pregnancy.
 Identify pharmacological strategies to manage pregnancy-associated symptoms.
Identify pharmacological strategies to manage pregnancy-associated symptoms.
 Identify the prototype drugs that alter uterine motility and describe these drugs.
Identify the prototype drugs that alter uterine motility and describe these drugs.
 Identify the prototype drugs used during labor and delivery and describe these drugs.
Identify the prototype drugs used during labor and delivery and describe these drugs.
 Discuss the use of drugs and herbs during lactation, including their effect on the infant.
Discuss the use of drugs and herbs during lactation, including their effect on the infant.
 Implement the nursing process in the care of the women of childbearing age.
Implement the nursing process in the care of the women of childbearing age.
Clinical Application Case Study
Lauren Ross is in the 35th week of pregnancy with her fourth child. During her weekly visit to the certified nurse midwife, her blood pressure is elevated, 150/100 mm Hg, on two consecutive readings. The nurse midwife checks her urine for protein and determines that she is spilling protein in her urine. Ms. Ross has facial swelling with edema around the eyes and nose and complains of a headache, with mild epigastric pain. Also, her vaginal culture is positive for perinatal group B streptococcus (GBS). In addition, during her pregnancy, she has been taking the antidepressant escitalopram (Lexapro) 10 mg per day and has continued to smoke. The nurse midwife admits her to the labor and delivery unit.
KEY TERMS
Abortifacients: drugs used to terminate pregnancy up to 20 weeks after the last menstrual period
Eclampsia: characterized by the onset of seizures; occurs in some women with preeclampsia
Galactagogues: a category of herbs known to induce lactation or stimulate the production of breast milk in postpartal women
Organogenesis: formation of organs during development
Oxytocics: drugs that initiate uterine contractions, thus inducing childbirth
Preeclampsia: pregnancy-induced hypertension and proteinuria
Preterm labor: uterine contractions with cervical changes before 37 weeks of gestation, resulting in birth
Prostaglandins: chemical mediators, such as uterotonics, that help initiate uterine contractions
Teratogenic: causing abnormal embryonic or fetal development
Tocolytics: drugs used to stop preterm labor
Uterotonics: drugs to control postpartum bleeding
Introduction
Drug use before and during pregnancy and lactation requires special consideration. Women of childbearing age may become pregnant, and they may ingest drugs that may cause fetal harm before they know they are pregnant. In general, pregnant or lactating women should avoid or minimize use of medications whenever possible. This chapter discusses drugs related to pregnancy and lactation, including infertility drugs, vaccines, tocolytics (drugs used to stop preterm labor), oxytocics (drugs used to initiate uterine contractions), drugs used to stop postpartum hemorrhage (uterotonics), and selected teratogenic drugs (agents causing abnormal embryonic or fetal development). Description of many of these drugs appears elsewhere in the text.
Drug Therapy for Infertility
A woman who has been unable to conceive for at least 1 year of sexual intercourse without the use of any form of birth control is infertile. In women, the most common causes are ovulation disorders, blocked fallopian tubes, endometriosis, and advanced maternal age, which affects egg quality and quantity. In men, causes include absence of sperm, declining sperm counts, testicular abnormalities, and ejaculatory dysfunction. Factors such as implantation, uterine and hormonal environment, and embryo integrity may also play a role. They are critical to fetal viability and a normally progressing pregnancy.
Drug therapy is an integral part of treating infertility. Drugs prescribed for a woman experiencing infertility increase follicular maturation and promote ovulation. It is necessary to take the total dose at the same time each day to enhance effects of a particular medication. Also, coitus every other day enhances fertility due to increased sperm counts.
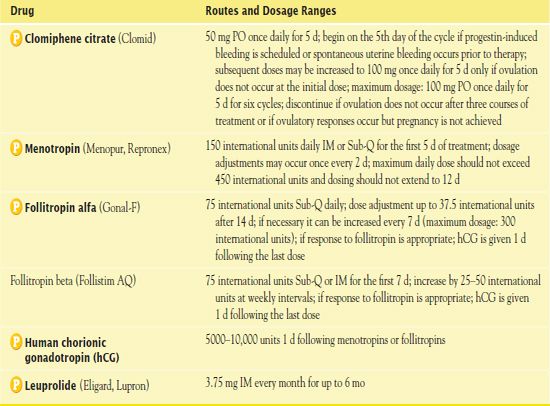
Table 6.1 presents the routes and dosage ranges for the infertility drugs.
Clomiphene Citrate
 Clomiphene citrate (Clomid) is an ovarian stimulator and selective estrogen receptor. This drug increases the amount of follicle-stimulating hormone (FSH) secreted by the pituitary gland, thus inducing ovulation for women who have infrequent or absent menstrual periods. Health care providers use it for the treatment of ovulatory failure in women who have tried to become pregnant but have failed. Ovulation occurs 5 to 10 days after the course of clomiphene treatment has been completed. Prior to beginning the drug regimen, the nurse instructs the woman about taking her basal temperature 5 to 10 days following administration. An incremental rise in temperature is an indication of ovulation.
Clomiphene citrate (Clomid) is an ovarian stimulator and selective estrogen receptor. This drug increases the amount of follicle-stimulating hormone (FSH) secreted by the pituitary gland, thus inducing ovulation for women who have infrequent or absent menstrual periods. Health care providers use it for the treatment of ovulatory failure in women who have tried to become pregnant but have failed. Ovulation occurs 5 to 10 days after the course of clomiphene treatment has been completed. Prior to beginning the drug regimen, the nurse instructs the woman about taking her basal temperature 5 to 10 days following administration. An incremental rise in temperature is an indication of ovulation.
Clomiphene is a mixture of zuclomiphene and enclomiphene. Metabolized by the liver, the drug has a half-life of 5 to 7 days. It is excreted in the feces and urine.
Possible adverse effects of clomiphene include hot flashes, breast pain and tenderness, and uterine bleeding. Some women have reported blurred vision, visual changes, and headaches. Contraindications include liver disease, thyroid or adrenal disease, ovarian cysts, and abnormal uterine bleeding.
Menotropin
 Menotropin (Menopur, Repronex) is a gonadotropin given to women who have been diagnosed with anovulation. The drug stimulates FSH and luteinizing hormone (LH) to promote the development and maturation of ovarian follicles. Administration may be subcutaneous, in alternating sides of the abdomen, or intramuscular, in large muscles. Following its administration, the woman receives human chorionic gonadotropin (hCG) (see later discussion). Menotropin is well absorbed and excreted in the urine.
Menotropin (Menopur, Repronex) is a gonadotropin given to women who have been diagnosed with anovulation. The drug stimulates FSH and luteinizing hormone (LH) to promote the development and maturation of ovarian follicles. Administration may be subcutaneous, in alternating sides of the abdomen, or intramuscular, in large muscles. Following its administration, the woman receives human chorionic gonadotropin (hCG) (see later discussion). Menotropin is well absorbed and excreted in the urine.
During menotropin therapy, it is necessary to monitor both hCG and serum estradiol measurements. The adverse effects and contraindications of menotropin are similar to those of clomiphene citrate.
Follitropins
 Follitropin alfa (Gonal-F) and follitropin beta (Follistim AQ) are drugs used to stimulate follicle development and thus promote fertility. Administration is subcutaneous, in calibrated syringes provided by the manufacturer. It is important that the drugs not be shaken before administration. After receiving follitropins, as with menotropins, women should also receive hCG (see later discussion)—1 day after the last dose of follitropin.
Follitropin alfa (Gonal-F) and follitropin beta (Follistim AQ) are drugs used to stimulate follicle development and thus promote fertility. Administration is subcutaneous, in calibrated syringes provided by the manufacturer. It is important that the drugs not be shaken before administration. After receiving follitropins, as with menotropins, women should also receive hCG (see later discussion)—1 day after the last dose of follitropin.
The adverse effects of the follitropins are similar to those of clomiphene. Contraindications include hypersensitivity as well as the presence of tumors in the ovary, breast, pituitary gland, uterus, or hypothalamus. It is necessary to monitor serum estradiol levels to determine the medication response.
Human Chorionic Gonadotropin
 Human chorionic gonadotropin, or hCG, is manufactured as Novarel or Pregnyl. This drug is a human formulation of hCG that is obtained from the urine of pregnant women. It is usually used as a replacement for LH. After administration of this form of hCG (after administration of menotropin or follitropin), the LH stimulates ovulation.
Human chorionic gonadotropin, or hCG, is manufactured as Novarel or Pregnyl. This drug is a human formulation of hCG that is obtained from the urine of pregnant women. It is usually used as a replacement for LH. After administration of this form of hCG (after administration of menotropin or follitropin), the LH stimulates ovulation.
Adverse effects of hCG include edema, depression, breast enlargement, ovarian cyst, and ovarian hypersensitivity. Contraindications include neoplasms or known hypersensitivity to the hormone.
Leuprolide
 Leuprolide (Lupron) is a gonadotropin-releasing hormone that has an unlabeled use in the treatment of infertility. Administered subcutaneously, it prevents premature ovulation and enhances the production of a larger quantity of quality eggs.
Leuprolide (Lupron) is a gonadotropin-releasing hormone that has an unlabeled use in the treatment of infertility. Administered subcutaneously, it prevents premature ovulation and enhances the production of a larger quantity of quality eggs.
Potential adverse effects of leuprolide include hot flashes, headache, mood swings, insomnia, vaginal dryness, decreased breast size, painful intercourse, and bone loss.
NCLEX Success
1. A couple has been trying to conceive for the past 8 months without success. Which of the following medications is the first drug of choice?
A. leuprolide (Lupron)
B. human chorionic gonadotropin (hCG) (Novarel)
C. follitropin beta (Follistim AQ)
D. clomiphene citrate (Clomid)
2. A woman diagnosed with anovulation receives a prescription for menotropin (Menopur, Repronex) to be administered subcutaneously. The nurse is teaching her about the administration of the medication. The nurse should teach the woman to
A. massage the area prior to administering the drug
B. administer the drug at a 90-degree angle
C. alternate the sides of the abdomen for the injection sites
D. take human chorionic gonadotropin before the menotropin
Drugs Used in Pregnancy
During pregnancy, mother and fetus undergo physiologic changes that influence drug effects. In pregnant women, physiologic changes alter drug pharmacokinetics (Table 6.2). In general, drug effects are less predictable because plasma volume expansion decreases plasma drug concentrations, and increased metabolism by the liver and increased elimination by the kidneys shorten the duration of drug actions and effects.
Maternal–Placental–Fetal Circulation
Drugs ingested by the pregnant woman reach the fetus through the maternal–placental–fetal circulation, which is completed about the 3rd week after conception. On the maternal side, arterial blood pressure carries blood and drugs to the placenta. In the placenta, maternal and fetal blood are separated by a few thin layers of membrane, which drugs can readily cross. Placental transfer begins about the 5th week after conception. After drugs enter the fetal circulation, relatively large amounts are pharmacologically active because the fetus has low levels of serum albumin and thus low levels of drug binding. Most drug molecules are transported to the fetal liver, where they are metabolized. Metabolism occurs slowly because the liver is immature in quantity and quality of drug-metabolizing enzymes. Drugs metabolized by the fetal liver are excreted by fetal kidneys into amniotic fluid. Excretion also is slow and inefficient due to immature development of fetal kidneys. Other drug molecules are transported directly to the heart, which then distributes them to the brain and coronary arteries. Drugs enter the fetal brain easily because the blood–brain barrier is poorly developed. Approximately half of the drug-containing blood is then transported through the umbilical arteries to the placenta, where it reenters the maternal circulation. The mother can metabolize and excrete some drug molecules for the fetus.
Drug Effects on the Fetus
Drug effects are determined mainly by the type and amount of drug, duration of exposure, and level of fetal growth and development during exposure. The fetus is sensitive to drug effects because it is small, has few plasma proteins that can bind drug molecules, and has a weak capacity for metabolizing and excreting drugs. In addition, the fetus is exposed to any drugs circulating in maternal blood. Molecular size, weight, and lipid solubility determine which substances (chemicals, drugs, and antibodies) are readily absorbed into the fetal circulation from the maternal circulation. When drugs are taken on a regular schedule, fetal blood usually contains 50% to 100% of the amount in maternal blood. This means that any drug that stimulates or depresses the central nervous, cardiovascular, respiratory, or other body system in the mother has the potential to stimulate or depress those systems in the fetus. In some cases, fetotoxicity occurs. Drugs that may be teratogenic (causing abnormal embryonic or fetal development) are a major concern. Drug-induced teratogenicity is most likely to occur when drugs are taken during the first 3 months of pregnancy—during organogenesis (formation of embryonic organs during the first 3 to 8 weeks after conception) (Fig. 6.1). Malformations that occur during the preembryonic period (first and second week of pregnancy postconception) rarely result in a viable fetus (fetal stage starts after completion of week 8 of embryonic life). During the embryonic and fetal stages, teratogenic insult and timing result in the targeting of specific organ growth during organogenesis and subsequent maturation and refinement of an organ’s physiologic purpose.
For drugs taken during the second and third trimesters, adverse effects are usually manifested in the neonate (birth to 1 month) or infant (1 month to 1 year) as growth retardation, respiratory problems, infection, or bleeding. It should be emphasized, however, that drugs taken at any time during pregnancy can affect the baby’s brain because brain development continues throughout pregnancy and after birth. The U.S. Food and Drug Administration (FDA) requires manufacturers to assign new drugs a pregnancy risk category to indicate their potential for causing birth defects (see Chap. 2 for more information). Box 6.1 is a list of teratogenic drugs.
BOX 6.1 Selected Teratogenic Drugs
Risk Category D
 Angiotensin-converting enzyme (ACE) inhibitors (e.g., captopril and others) (second and third trimesters)
Angiotensin-converting enzyme (ACE) inhibitors (e.g., captopril and others) (second and third trimesters)
 Angiotensin II receptor blockers (ARBs; e.g., losartan and others) (second and third trimesters)
Angiotensin II receptor blockers (ARBs; e.g., losartan and others) (second and third trimesters)
 Antibacterials (aminoglycosides, tetracyclines, tigecycline, trimethoprim in third trimester)
Antibacterials (aminoglycosides, tetracyclines, tigecycline, trimethoprim in third trimester)
 Antiepileptics (carbamazepine, phenytoin, valproic acid)
Antiepileptics (carbamazepine, phenytoin, valproic acid)
 Antifungals (voriconazole)
Antifungals (voriconazole)
 Antineoplastics (ibritumomab, idarubicin, ifosfamide, imatinib, irinotecan)
Antineoplastics (ibritumomab, idarubicin, ifosfamide, imatinib, irinotecan)
 Antithyroid agents (e.g., propylthiouracil)
Antithyroid agents (e.g., propylthiouracil)
 Antivirals (efavirenz)
Antivirals (efavirenz)
 Benzodiazepine (e.g., alprazolam, diazepam, lorazepam)
Benzodiazepine (e.g., alprazolam, diazepam, lorazepam)
 Bisphosphonates (pamidronate, zoledronic acid) Mood stabilizer (lithium)
Bisphosphonates (pamidronate, zoledronic acid) Mood stabilizer (lithium)
 Nicotine replacement products (oral inhaler, nasal spray, transdermal patch)
Nicotine replacement products (oral inhaler, nasal spray, transdermal patch)
 Opioid analgesics (with prolonged use or high doses at term)
Opioid analgesics (with prolonged use or high doses at term)
Risk Category X
 Anticoagulant (warfarin)
Anticoagulant (warfarin)
 Antineoplastics (e.g., cyclophosphamide, methotrexate)
Antineoplastics (e.g., cyclophosphamide, methotrexate)
 Antirheumatoid arthritis drug (leflunomide)
Antirheumatoid arthritis drug (leflunomide)
 Antiviral (ribavirin)
Antiviral (ribavirin)
 Benzodiazepine sedative/hypnotics (e.g., flurazepam)
Benzodiazepine sedative/hypnotics (e.g., flurazepam)
 Female sex hormones (estrogens, progestins, oral contraceptives)
Female sex hormones (estrogens, progestins, oral contraceptives)
 Male sex hormones (androgens, anabolic steroids)
Male sex hormones (androgens, anabolic steroids)
 Nicotine replacement product, chewing gum
Nicotine replacement product, chewing gum
 Retinoids (e.g., acitretin, isotretinoin, and several topical preparations)
Retinoids (e.g., acitretin, isotretinoin, and several topical preparations)
 Statin cholesterol-lowering drugs (e.g., atorvastatin, others)
Statin cholesterol-lowering drugs (e.g., atorvastatin, others)
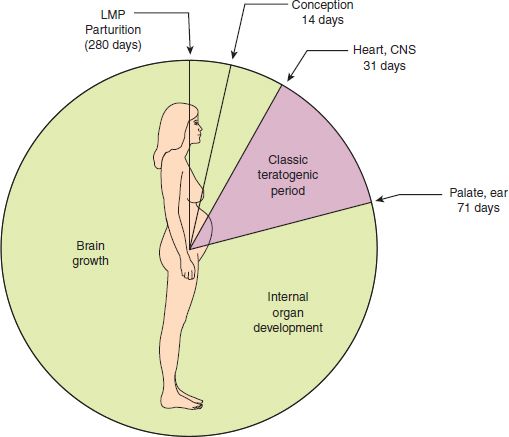
Figure 6.1 The gestational clock showing the classic teratogenic risk assessment. (Adapted from Niebyl, J. (1999). Drugs and related areas in pregnancy. In J. Sciarra (Ed.). Obstetrics and gynecology. Philadelphia, PA: Lippincott Williams & Wilkins.)
Principles of Drug Therapy in Pregnancy
Before administering a drug to a pregnant woman, it is the responsibility and obligation of all health care providers, including nurses, to conduct a risk–benefit assessment—a comprehensive analytic comparison of the benefits to the mother and the risks to the fetus. Inclusion of family in a decision regarding drug exposure during pregnancy and lactation to obtain informed consent is critical. Ideally, the risk to the fetus should be small compared with the potential maternal benefit. It is necessary to consider the consequences with and without drug therapy. Important factors are gestational age; drug route, dosage, and concentration; and duration of exposure.
General guidelines for drug therapy in pregnancy include the following:
• Pregnant women should take no drugs, regardless of their pregnancy risk category. It is essential that no drug be used during pregnancy unless it is clearly needed and the potential benefit to the mother outweighs the risk of potential harm to the fetus.
• However, although the teratogenicity of many drugs is unknown, most medications required by pregnant women can be used safely and most children are born healthy.
• When drug therapy is necessary, the choice of drug depends on the stage of pregnancy and available drug information. During the first trimester, for example, an older drug that has not been associated with fetotoxic or teratogenic effects is usually preferred over a newer drug of unknown fetotoxicity or teratogenicity.
• It is important to give any drug used during pregnancy at the lowest effective dose for the shortest possible time.
• Some immunizations are safe in pregnancy, although live-virus vaccines (e.g., measles, mumps, rubella) should be avoided because of possible harmful effects to the fetus. Vaccines against pneumococcal pneumonia, meningococcal meningitis, and hepatitis A can be used if indicated. Influenza vaccine is indicated in all women who are pregnant during influenza season. (However, FluMist, a live virus vaccine given by nasal spray, should not be given to pregnant women.) In addition, hepatitis B vaccine (if the mother is high risk and negative for hepatitis B antigen) and toxoids (e.g., diphtheria, tetanus) are considered safe for use. Hyperimmune globulins can be given to pregnant women who are exposed to hepatitis B, tetanus, or varicella (chickenpox).
• It is essential that pregnant women know how these principles affect them. Box 6.2 summarizes patient teaching guidelines regarding the use of drugs during pregnancy (and lactation).
BOX 6.2  Patient Teaching Guidelines: Drug Use During Pregnancy and Lactation
Patient Teaching Guidelines: Drug Use During Pregnancy and Lactation
 Any systemic drug ingested by a pregnant woman reaches the fetus and may interfere with fetal growth and development. For most drugs, safety during pregnancy has not been established, and all drugs are relatively contraindicated. Therefore, any drug use must be cautious and minimal to avoid potential harm to the fetus.
Any systemic drug ingested by a pregnant woman reaches the fetus and may interfere with fetal growth and development. For most drugs, safety during pregnancy has not been established, and all drugs are relatively contraindicated. Therefore, any drug use must be cautious and minimal to avoid potential harm to the fetus.
 Avoid drugs when possible and use them very cautiously when necessary. If women who are sexually active and not using effective contraception take any drugs, there is a high risk that potentially harmful agents may be ingested before pregnancy is suspected or confirmed. It is estimated that 50% or more of pregnancies are unplanned.
Avoid drugs when possible and use them very cautiously when necessary. If women who are sexually active and not using effective contraception take any drugs, there is a high risk that potentially harmful agents may be ingested before pregnancy is suspected or confirmed. It is estimated that 50% or more of pregnancies are unplanned.
 Lifestyle or nontherapeutic drugs associated with problems during pregnancy include alcohol, caffeine, and cigarette smoking. Women should completely avoid alcohol when trying to conceive and throughout pregnancy; no amount is considered safe. Caffeine intake should be limited to about three caffeinated beverages per day; excessive intake should be avoided. Women who smoke should quit if possible during pregnancy to avoid the effects of nicotine, carbon monoxide, and other chemicals on the fetus. However, the use of nicotine replacement products during pregnancy/lactation is recommended with behavioral interventions.
Lifestyle or nontherapeutic drugs associated with problems during pregnancy include alcohol, caffeine, and cigarette smoking. Women should completely avoid alcohol when trying to conceive and throughout pregnancy; no amount is considered safe. Caffeine intake should be limited to about three caffeinated beverages per day; excessive intake should be avoided. Women who smoke should quit if possible during pregnancy to avoid the effects of nicotine, carbon monoxide, and other chemicals on the fetus. However, the use of nicotine replacement products during pregnancy/lactation is recommended with behavioral interventions.
 Herbal supplements are not recommended; their effects during pregnancy are unknown.
Herbal supplements are not recommended; their effects during pregnancy are unknown.
 Measures to prevent the need for drug therapy include a healthful lifestyle (adequate nutrition, exercise, rest, and sleep; avoiding alcohol and cigarette smoking) and avoiding infection (personal hygiene, avoiding contact with people known to have infections, maintaining indicated immunizations).
Measures to prevent the need for drug therapy include a healthful lifestyle (adequate nutrition, exercise, rest, and sleep; avoiding alcohol and cigarette smoking) and avoiding infection (personal hygiene, avoiding contact with people known to have infections, maintaining indicated immunizations).
 Inform any health care provider from whom treatment is sought if there is a possibility of pregnancy.
Inform any health care provider from whom treatment is sought if there is a possibility of pregnancy.
 Many drugs are excreted in breast milk to some extent and reach the nursing infant. The infant’s health care provider should be informed about medications taken by the nursing mother and consulted about potential drug effects on the infant. Before taking over-the-counter medications, consult a health care provider. In regard to nontherapeutic drugs, recommendations include the following:
Many drugs are excreted in breast milk to some extent and reach the nursing infant. The infant’s health care provider should be informed about medications taken by the nursing mother and consulted about potential drug effects on the infant. Before taking over-the-counter medications, consult a health care provider. In regard to nontherapeutic drugs, recommendations include the following:
 Alcohol should be used in moderation and nursing should be withheld temporarily after alcohol consumption (1 to 2 hours per drink). Alcohol reaches the baby through breast milk, with the highest concentration about 30 to 60 minutes after drinking (60 to 90 minutes if taken with food). The effects of alcohol on the baby are directly related to the amount of alcohol the mother consumes. Moderate-to-heavy drinking (two or more drinks per day) can interfere with the ability to breast-feed, harm the baby’s motor development, and slow the baby’s weight gain. If you plan to drink (e.g., wine with dinner), you can avoid breastfeeding for a few hours (until the alcohol has time to leave your system) or you can pump your milk before drinking alcohol and give it to the baby after you have had the alcohol. You can also pump and discard the milk that is most affected by the ingested alcohol.
Alcohol should be used in moderation and nursing should be withheld temporarily after alcohol consumption (1 to 2 hours per drink). Alcohol reaches the baby through breast milk, with the highest concentration about 30 to 60 minutes after drinking (60 to 90 minutes if taken with food). The effects of alcohol on the baby are directly related to the amount of alcohol the mother consumes. Moderate-to-heavy drinking (two or more drinks per day) can interfere with the ability to breast-feed, harm the baby’s motor development, and slow the baby’s weight gain. If you plan to drink (e.g., wine with dinner), you can avoid breastfeeding for a few hours (until the alcohol has time to leave your system) or you can pump your milk before drinking alcohol and give it to the baby after you have had the alcohol. You can also pump and discard the milk that is most affected by the ingested alcohol.
 Caffeine is considered compatible with breast-feeding. However, large amounts should be avoided because infants may be jittery and have difficulty sleeping.
Caffeine is considered compatible with breast-feeding. However, large amounts should be avoided because infants may be jittery and have difficulty sleeping.
 Cigarette smoking is contraindicated. Nicotine and an active metabolite are concentrated in milk, and the amounts reaching the infant are proportional to the number of cigarettes smoked by the mother. Ideally, the mother who smokes would stop. If unable or unwilling to stop, she should decrease the number of cigarettes as much as possible, avoid smoking before nursing, and avoid smoking (or allowing other people to smoke) in the same room with the infant. The risk of sudden infant death syndrome (SIDS) is greater when a mother smokes or when the baby is around secondhand (passive) smoke. Maternal smoking and passive smoke may also increase respiratory and ear infections in infants.
Cigarette smoking is contraindicated. Nicotine and an active metabolite are concentrated in milk, and the amounts reaching the infant are proportional to the number of cigarettes smoked by the mother. Ideally, the mother who smokes would stop. If unable or unwilling to stop, she should decrease the number of cigarettes as much as possible, avoid smoking before nursing, and avoid smoking (or allowing other people to smoke) in the same room with the infant. The risk of sudden infant death syndrome (SIDS) is greater when a mother smokes or when the baby is around secondhand (passive) smoke. Maternal smoking and passive smoke may also increase respiratory and ear infections in infants.
 All drugs of abuse (e.g., cocaine, heroin, marijuana, methamphetamine, and phencyclidine) are contraindicated.
All drugs of abuse (e.g., cocaine, heroin, marijuana, methamphetamine, and phencyclidine) are contraindicated.
NCLEX Success
3. A woman with a seizure disorder has been taking phenytoin (Dilantin) since she was 6 years old. She has recently married and wants to start a family. She understands the risk related to the use of phenytoin during pregnancy. What should the nurse advise the woman about pregnancy?
A. She should discuss her concerns with her gynecologist and neurologist.
B. She should stop the phenytoin and take folic acid.
C. She should begin to take prenatal vitamins.
D. She should consult a genetic counselor about her seizure disorder.
4. During the autumn, it is recommended that a pregnant woman receive which of the following immunizations?
A. rubella
B. mumps
C. influenza
D. tetanus
 TABLE 6.1
TABLE 6.1