Jacqueline L Rosenjack Burchum, DNSc, FNP-BC, APN, CNE On completion of this chapter, the reader will be able to: 1. Describe the characteristics of medication use in older adults. 2. List medications that are best avoided in older adults. 3. Identify potential risk factors for adverse drug reactions. 4. Describe the pharmacokinetic and pharmacodynamic changes associated with aging and the implications for drug therapy. 5. Recognize significant drug–drug, drug–food, and drug–disease interactions, giving specific examples of each. 6. State the impact that drugs may have on an older adult’s quality of life. 7. Describe issues related to the optimum use of psychotropics, cardiovascular agents, and antimicrobials. 8. Anticipate the effects of increased availability of nonprescription and herbal remedies on patient self-management. 9. Identify risk factors for nonadherence and suggest strategies to improve adherence. Drugs have an important and often essential role in the management of conditions and maintenance of well-being in older adults. At least 94% of adults aged 65 to 74 take medications of some type. Of these, more than 84% regularly take prescription medications, 46% take over-the-counter medications, and 53% take dietary supplements. The prevalence of drug use increases even more for those 75 years or older (Qato et al, 2008). When a drug is taken, it begins a journey of four phases: absorption, distribution, metabolism, and excretion. What the body does to the drug during the four phases of this journey is known as pharmacokinetics. The normal physiologic changes that occur with aging can alter pharmacokinetics. This section explores those pharmacokinetic changes that occur with aging. A summary of important age-related physiologic alterations that affect pharmacokinetics is presented in Table 22–1. TABLE 22–1 AGE-RELATED CHANGES IN PHARMACOKINETICS From Hammerlein A, Derendorf H, Lowenthal DT: Pharmacokinetic and pharmacodynamic changes in the elderly: clinical implications, Clin Pharmacokinet 35(1):49, 1998. GI, Gastrointestinal. Absorption refers to the movement of a drug from the site of administration to the systemic circulation. The primary alteration of absorption occurs with drugs taken orally or via feeding tubes. To be absorbed, orally administered drugs first need to enter the stomach and intestines. With aging there is decreased secretion of gastric acid, slowed gastric emptying and decreased gastrointestinal motility, decreased absorptive capacity, and decreased blood flow to the stomach and intestines (Hutchison & O’Brien, 2007). Although these effects may slow absorption of oral drugs, they do not substantially affect the amount of drug absorption that ultimately occurs; therefore age-related changes in absorption of most drugs are usually insignificant (Beers, Porter, Jones, et al, 2006; Flammiger & Maibach, 2006); however, the first dose of a new drug may take longer to take effect (Hutchison & O’Brien, 2007). Topical drugs also face barriers to absorption. Aged skin has decreased water content, a relative decrease in lipid content, and a decrease in tissue perfusion. These changes may result in impaired absorption of some medications that are administered via lotions, creams, ointments, and patches (Flammiger & Maibach, 2006). Distribution refers to movement of the drug from the systemic circulation to the site of action. Distribution is affected by the relative amounts of total body water, fat content, and protein binding. Older adults have alterations in each of these. Total body water decreases gradually with aging. Because there is less water for dilution, this may result in a higher concentration of highly water-soluble (hydrophilic) drugs (Lilley, Harrington, & Synder, 2007). Because hydrophilic drugs have a tendency to stay within the circulation longer, this will be reflected by a higher serum drug level on laboratory studies. If the risk of toxicity is to be decreased, smaller doses of hydrophilic medications such as digoxin, lithium, atenolol, and aminoglycosides may be needed for older adults (Beers et al, 2006). Conversely, older adults have a decrease in lean body mass, so the percentage of fat content is increased in comparison with younger adults of similar weight. As a consequence of this higher proportion of fat, there will be an increase in the distribution of highly fat-soluble (lipophilic) drugs (Hutchison & O’Brien, 2007). As a result, lipophilic drugs such as benzodiazepines and certain anesthetics (e.g., halothane and thiopental) may exhibit extended effects (Hutchison & O’Brien, 2007; Lilley et al, 2007). A final area of concern regarding distribution involves drugs that are highly protein bound. Drugs of this type, such as warfarin, phenytoin, furosemide, and naproxen, tend to bind primarily to albumin, a protein in the plasma, and only become active when unbound. With age, particularly for malnourished or frail adults, albumin levels may drop. As a result of decreased sites for protein binding, the activity of highly protein-bound drugs, and any side effects caused by these drugs, may be increased (Beers et al, 2006; Hutchison & O’Brien, 2007; Lilley et al, 2007). Metabolism refers to the reactions that transform drugs into metabolites that can be more easily excreted. (Less commonly, metabolism will convert inactive drugs, known as prodrugs, to an active form.) Metabolism is accomplished by biochemical reactions that take place primarily in the liver via phase 1 (oxidation–reduction via the cytochrome P [CYP] 450 enzyme system) and phase 2 (glucuronidation, acetylation, or sulfation) reactions. It was once believed that there was a generalized decrease in all metabolic processes with aging. More recent research demonstrates that aging does not appear to effect phase 2 processes. Furthermore, while some isoenzymes (e.g., CYP2C19 has a role in metabolizing diazepam, naproxen, omeprazole, and propranolol) are reduced with aging, others remain unchanged, are variable, or affect only those older adults who are malnourished or frail (Hutchinson & O’Brien, 2007). In addition to the metabolic processes, the adequacy of hepatic circulation to direct drugs to the liver for metabolism must be considered. With aging there is a 35% decrease in hepatic blood flow (Hutchison & O’Brien, 2007). This is particularly relevant in regard to the role of first-pass metabolism. First-pass metabolism is a process in which a large percentage of drugs absorbed from the stomach or intestines first enters the portal circulation of the liver and is metabolized (inactivated) before reaching the systemic circulation. A decrease in hepatic blood flow can result in a decrease in the amount of a drug diverted to the liver for transformation before it enters the systemic circulation. With decreased first-pass metabolism, a greater amount of active drug enters the systemic circulation; consequently, there is an additional risk that standard doses of drugs will more likely result in toxic effects (Hutchison & O’Brien, 2007; Lilley et al, 2007). The implications of these alterations are that metabolism of some drugs may be slowed, thus leading to a prolonged drug half-life and an increased risk of drug accumulation and toxic effects; however, this cannot be generalized to all older adults. Individualization of medication regimens and close assessments for signs or symptoms of toxic effects or complications are necessary while dosing schedules are being optimized. Excretion, the elimination of drugs from the body, occurs primarily via the kidneys. When renal function is decreased, half-life increases and drugs can accumulate to toxic levels. This has important implications for older adults because, for most, renal function decreases with aging, especially for those who have conditions such as hypertension or heart disease (Shi, Mörike, & Klotz, 2008). Because the degree of renal function varies from patient to patient, it is important to evaluate whether adequate renal function exists and, if not, to what degree it is compromised. A serum creatinine level is commonly used as a screening test for renal function; however, in older adults, the serum creatinine level may be within normal limits even when renal function is significantly compromised (Hutchison & O’Brien, 2007; Shi et al, 2008). The best indicator of renal function is the glomerular filtration rate (GFR). The most commonly used method to calculate the GFR is the Cockcroft-Gault (CG) formula; however, this may result in an inaccurate measure of GFR in older adults (Hutchison & O’Brien, 2007; Shi et al, 2008). For older adults, most experts currently recommend that laboratories use the Modification of Diet in Renal Disease (MDRD) formula to estimate GFR (Fliser, 2008; Schrier, 2008; Shi et al, 2008; Verhave, Fesler, Ribstein, et al, 2005). The prescriber can then use information gleaned from the GFR to determine whether lower doses are needed. The physiologic alterations associated with aging can also alter how the older adult responds to drugs. Pharmacodynamics, what the drug does to the body, is the term used to explain the body’s response to a drug. As people age, pharmacodynamics is altered by the number of receptors and their affinity for drugs, as well as by alterations in response to receptor stimulation (Shi et al, 2008). As a result, drug sensitivity may be either increased (e.g., increased sedative effects of benzodiazepines) or decreased (e.g., decreased bronchodilator response to beta agonists such as albuterol). In both respects, the altered sensitivity is unrelated to the drug level. Furthermore, the bodily processes that maintain homeostasis become less effective; consequently, the older adult may be less able to tolerate the effects and side effects of certain drugs. As with nursing actions related to pharmacokinetics, it is imperative that the nurse assess responses to drugs so that therapy can be adjusted, if needed, to improve patient outcomes. As a result of age-related changes in pharmacodynamics and pharmacokinetics, there are some drugs and drug classes that are more likely to create problems for older adults. To delineate problematic medications, expert panels have developed a number of screening tools and lists detailing inappropriate drugs for older adults. The most well-known of these is the Beers Criteria for Potentially Inappropriate Medication Use in Older Adults originally formulated in 1991 (Beers et al, 1991) and subsequently revised (Stuck et al, 1994; Beers, 1997). The most recent update by Dr. Beers and his colleagues was in 2002 (Fick, Cooper, Wade, et al, 2003). Despite newer guides for inappropriate drugs such as that developed by the Academy of Managed Care Pharmacy and the National Committee for Quality Assurance (2006), the Beers criteria remain the most often used reference for published research. The Beers list has been widely disseminated in the literature since its initial development; however, the use of potentially inappropriate medication in older adults remains a significant problem. A nationwide study of 493,971 older patients from 384 U.S. hospitals revealed that almost half (49%) were prescribed one or more of these drugs (Rothberg et al, 2008). A separate study that included a review of prehospitalization and discharge medications also found significant concerns for inappropriate medications prescribed in the nonhospital setting. Of those in the study, 39% of older patients were taking at least one inappropriate medication before admission, and on discharge, those prescribed at least one inappropriate medication increased to 41% (Hale et al, 2008). Although the Beers criteria provide important information regarding inappropriate medications, it is important to recognize that those medications that are considered appropriate and are commonly prescribed for older adults may carry serious drug-related risks. For example, a retrospective review of more than 175,000 emergency department visits for adverse drug events (ADEs) by older adults revealed that a third of the visits were in response to problems caused by insulin, warfarin, and digoxin (Budnitz, Shehab, Kegler, & Richards, 2007). Of these, only digoxin is included in the Beers criteria, and there it is designated low risk. Thus, it is important to remember that all drugs are potentially harmful and must be weighed in terms of benefit versus risk. Drug–drug interactions occur in a variety of ways. Perhaps the most common interaction is the result of altered metabolism via the CYP450 hepatic enzyme system. Some drugs have the ability to induce or inhibit the activity of various CYP isozymes, which results in speeding up or slowing down biotransformation of drugs metabolized by the affected set of isoenzymes. If the biotransformation is accelerated, the drug affected will be inactivated prematurely; whereas, if the biotransformation is decelerated, the drug may accumulate to toxic levels. Drugs may also interact indirectly through opposing or antagonistic actions. For example, in the patient who has both asthma and hypertension, a beta-blocker given to control hypertension may oppose the actions of a beta-agonist given to dilate airway passages. Drugs may also interact chemically. This is more readily seen in intravenous (IV) solutions in which incompatible drugs may crystallize when mixed; however, it may also occur when certain oral drugs are taken together. Table 22–2 lists examples of significant drug–drug interactions. TABLE 22–2 COMMON DRUG–DRUG INTERACTIONS IN OLDER ADULTS Drug–food interactions are less common than drug–drug interactions but still increase risk. The metabolism or effect of certain drugs can be altered when combined with certain foods. For example, potentially dangerous interactions can occur when certain drugs are taken with grapefruit juice. This occurs because a chemical found in grapefruit juice inhibits metabolism by 3A4 isoenzymes of the CYP450 enzyme system. The 3A4 isoenzymes are responsible for first-pass metabolism of a large number of drugs; therefore, as a result of inhibited metabolism, drugs normally metabolized by 3A4 isoenzymes, such as calcium channel blockers, may accumulate to high or even toxic levels. Some drugs may affect drug levels in other ways. For example, some laxatives may cause rapid transit of an orally administered drug through the gastrointestinal system so that it is not adequately absorbed. See Table 22–3 for examples (Kiani & Imam, 2007). TABLE 22–3 COMMON DRUG–FOOD INTERACTIONS IN OLDER ADULTS Drug–disease interactions may exacerbate patient conditions and hinder healing. These drugs are generally contraindicated in patients with coexisting underlying disease. For example, 13% of African American men and 20% of African American women are carriers of the gene that can cause a deficiency in the enzyme glucose-6-phosphate dehydrogenase (G6DP). If a patient with this deficiency takes certain drugs such as sulfonamides or aspirin, erythrocyte hemolysis can occur (Lilley et al, 2007). Table 22–4 lists examples of drug–disease interactions. TABLE 22–4 COMMON DRUG–DISEASE INTERACTIONS IN OLDER ADULTS GI, Gastrointestinal; NSAIDs, nonsteroidal antiinflammation drugs. Education is an essential component of any risk prevention program. Nurses should provide patients with information regarding the risk of potentially dangerous interactions among the drugs they are taking. It may also be helpful to provide the patient with a list of acceptable over-the-counter drugs for common problems such as mild pain or constipation. A “safe over-the-counter medication list” may be a useful tool for health care providers to review with patients before completing the office visit (Table 22–5). TABLE 22–5 A SAFE LIST FOR OVER-THE-COUNTER MEDICATIONS
Pharmacologic Management
Overview of Medication Use and Problems
Demographics of Medication Use
Pharmacokinetic Changes: What the Body Does to the Drug
VARIABLE
CHANGE
EXAMPLE
Absorption
Gastric pH
Increased
Calcium carbonate: decreased dissolution
Acid secretory capacity
Decreased
Calcium carbonate: decreased dissolution
GI blood flow or gastric motility
Diminished
Analgesics: delayed onset of effect, naproxen, salicylates; increased free concentration
Distribution
Plasma albumin
Diminished
Meperidine: increased free concentration caused by decreased binding to red blood cells
Protein affinity
Diminished
Propranolol: reduced unbound fraction
Alpha-1-acid glycoprotein
Increased
Psychotropics: increased distribution into fat; potential accumulation
Body fat
Increased
Long-acting benzodiazepines, tricyclic antidepressants, beta-blockers, narcotic analgesics: higher concentrations from decreased metabolism
Metabolism
Size of liver
Decreased
Long-acting benzodiazepines, tricyclic antidepressants, beta-blockers, narcotic analgesics: higher concentrations from decreased metabolism
Hepatic blood flow
Decreased
Long-acting benzodiazepines, tricyclic antidepressants, beta-blockers, narcotic analgesics: higher concentrations from decreased metabolism
Renal Function
Glomerular filtration rate
Decreased
Allopurinol, cephalosporins, chlorpropamide, ciprofloxacin, digoxin, H2-receptor blockers: higher concentrations due to reduced renal clearance
Renal plasma flow
Decreased
Allopurinol, cephalosporins, chlorpropamide, ciprofloxacin, digoxin, H2-receptor blockers: higher concentrations due to reduced renal clearance
Pharmacodynamic Changes: What the Drug Does to the Body
Inappropriate Drugs for Older Patients
Pharmacologic Contributors to Risk
Drug Interactions
DRUG–DRUG COMBINATION
POTENTIAL EFFECT
Warfarin and aspirin
Increased risk of bleeding
Warfarin and chloral hydrate
Increased risk of toxicity
Digitalis and quinidine
Increased risk of toxicity
Cimetidine and propranolol
Decreased clearance, increased bradycardia
Thiazides and longer acting antidiabetics
Increased risk of hypoglycemia
Levodopa and clonidine
Decreased antiparkinsonian effect
Diuretics and NSAIDs
Renal impairment
Lithium and diuretics
Increased risk of toxicity
Lovastatin (Mevacor) and gemfibrozil (Lopid)
Toxic liver effect
Prednisone and barbiturates
Decreased steroid effect
St. John’s wort and pseudoephedrine
Increased blood pressure
Ginkgo with aspirin
Increased bleeding risk
FOOD
DRUG
POTENTIAL EFFECT
Caffeine
Theophylline
Increased potential for toxicity
Fatty food
Griseofulvin
Increased absorption of drug
Blue cheese
Penicillin
Antagonistic action
Fiber
Digoxin
Absorption of drug into fiber, reducing drug action
Vitamin K foods: cabbage, greens, egg yolk, fish, rice
Warfarin
Decreased effect of drug, inhibiting anticoagulation
Food
Many antibiotics
Reduced absorption rate of drug
Mineral oil
Fat-soluble vitamins
Fat-soluble vitamins dissolve in oil; deficiency possible
Tyramine foods: aged cheese, wines, pickled herring, chocolate
Monoamine oxidase (MAO) inhibitors (phenelzine [Nardil], tranylcypromine [Parnate]), St. John’s wort
May precipitate hypertensive crisis
Vitamin B6 supplements
Levodopa-carbidopa
Reverses antiparkinsonian effect
Grapefruit juice
Cisapride, calcium channel blockers, quinidine
Altered metabolism and elimination can increase concentration of drug
Citrus juice
Calcium channel blockers
Gastric reflux exacerbated
DISEASE
DRUG
POTENTIAL EFFECT
Atrophic gastritis
Aspirin, NSAIDs
GI hemorrhage
Sinus or atrioventricular note disease
Digitalis, verapamil
Bradycardia
Venous insufficiency
Calcium channel blockers or beta-blockers
Edema, intermittent claudication
Cataracts
Corticosteroids
Accelerated cataract formation
Unstable bladder
Diuretics
Incontinence
Prostatic hypertrophy
Anticholinergics
Urinary retention
Parkinson’s disease
Metoclopramide, neuroleptics
Parkinson’s syndrome
Renal impairment
NSAIDs, contrast material, aminoglycosides
Acute renal failure
Chronic obstructive pulmonary disease
Beta-blockers, opiates
Bronchoconstriction, respiratory depression
Hypokalemia
Digitalis
Cardiac toxicity
Osteopenia
Corticosteroids
Fracture risk
Orthostatic hypotension
Diuretics, psychotropics, antihypertensives
Increased fall risk
Depression
Central-acting antihypertensives, alcohol, antianxiety drugs, corticosteroids
Exacerbation of depression
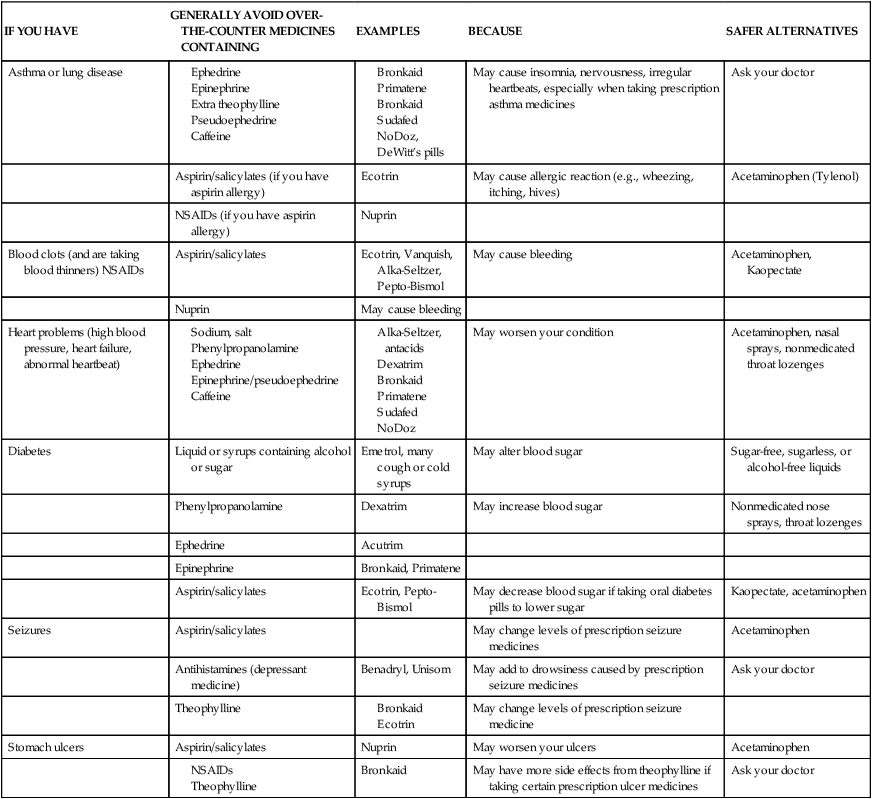
IF YOU HAVE
GENERALLY AVOID OVER- THE-COUNTER MEDICINES CONTAINING
EXAMPLES
BECAUSE
SAFER ALTERNATIVES
Asthma or lung disease
May cause insomnia, nervousness, irregular heartbeats, especially when taking prescription asthma medicines
Ask your doctor
Aspirin/salicylates (if you have aspirin allergy)
Ecotrin
May cause allergic reaction (e.g., wheezing, itching, hives)
Acetaminophen (Tylenol)
NSAIDs (if you have aspirin allergy)
Nuprin
Blood clots (and are taking blood thinners) NSAIDs
Aspirin/salicylates
Ecotrin, Vanquish, Alka-Seltzer, Pepto-Bismol
May cause bleeding
Acetaminophen, Kaopectate
Nuprin
May cause bleeding
Heart problems (high blood pressure, heart failure, abnormal heartbeat)
May worsen your condition
Acetaminophen, nasal sprays, nonmedicated throat lozenges
Diabetes
Liquid or syrups containing alcohol or sugar
Emetrol, many cough or cold syrups
May alter blood sugar
Sugar-free, sugarless, or alcohol-free liquids
Phenylpropanolamine
Dexatrim
May increase blood sugar
Nonmedicated nose sprays, throat lozenges
Ephedrine
Acutrim
Epinephrine
Bronkaid, Primatene
Aspirin/salicylates
Ecotrin, Pepto-Bismol
May decrease blood sugar if taking oral diabetes pills to lower sugar
Kaopectate, acetaminophen
Seizures
Aspirin/salicylates
May change levels of prescription seizure medicines
Acetaminophen
Antihistamines (depressant medicine)
Benadryl, Unisom
May add to drowsiness caused by prescription seizure medicines
Ask your doctor
Theophylline
May change levels of prescription seizure medicine
Stomach ulcers
Aspirin/salicylates
Nuprin
May worsen your ulcers
Acetaminophen
Bronkaid
May have more side effects from theophylline if taking certain prescription ulcer medicines
Ask your doctor
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Pharmacologic Management
Get Clinical Tree app for offline access
