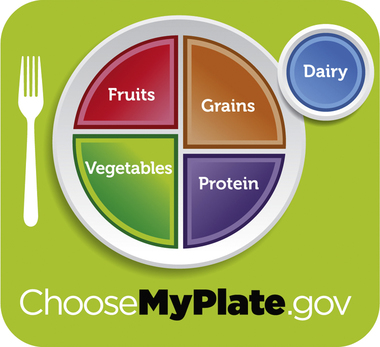
On completing this chapter, you will be able to do the following: 1. Develop a reasonable healthy eating and physical activity plan for yourself using the Dietary Guidelines for Americans 2010 (http://www.health.gov/dietaryguidelines/dga2010DietaryGuidelines2010.pdf). 2. Explain why the June 2011 MyPlate.gov (http://www.choosemyplate.gov/) is easier to comprehend and use as a mealtime food guide than MyPyramid. 3. List six how-to messages to guide healthy eating as a part of healthy food guidelines. 4. Explain why proper body mechanics help but do not prevent all back, shoulder, and other injuries nurses may develop. 5. Locate items on the clinical unit available to assist you with moving and lifting patients. 6. Differentiate between stress and burnout. 7. Develop a realistic plan to assist you in dealing with overwhelming stress or feelings of hopelessness during the school year. 8. Identify possible clues that may indicate a nurse is chemically impaired by alcohol and/or other drugs while on duty. 9. Explain the difference between codependency and conscientious nursing. 10. Discuss the difference between recreation and relaxation. 11. Describe which source of relaxation is most effective for you to use during class or on clinical. 12. Explain methods you will use to prevent the spread of infection among patients and from the clinical setting to your home and into the community. Because of the rise in childhood obesity and related illnesses, the 2010 White House Child Obesity Task Force requested that reasonable advice be developed to help facilitate easier healthy food choices. The 2010 guidelines are helpful, but both adults and children have had difficulty understanding and using the MyPyramid icon. As a result, the MyPlate icon was designed to replace MyPyramid (Figure 6-1). In June 2011, First Lady Michelle Obama and Secretary of Agriculture Tom Vilsack introduced the new icon. The White House is playing a leading role by coordinating the USDA guidelines with Michelle Obama’s “Let’s Move” initiative. • Enjoy your food, but eat less. • Make half of your plate fruits and vegetables. • Make half of your plate grains and proteins. • Make at least half of your grains whole grain. • Protein is the smallest part of the plate. • Switch to fat-free or low-fat (1%) milk. • Look for lower-sodium soup, bread, and frozen meals; choose foods with lower numbers. • Drink water instead of sugary drinks (http://www.chosemyplate.gov). • The 30 minutes of activity can even be divided into 10-minute increments. Ten-minute bursts of activity have been shown to be as effective as continuous exercise. The important thing is to choose an activity that you like and that fits in with your busy lifestyle. • Brisk walking (meaning 3.5 miles per hour) is probably the easiest for most people to incorporate into a busy day. If possible, walk to work, or park your car farther away from your destination. • Use stairs rather than the elevator. • Walk with a coworker during your lunchtime, or volunteer to be the one to go to another part of the building to pick up something. • If you are fitting in a walk with a friend at lunchtime, a few minutes of slower walking at the beginning can be a useful preparation for more brisk walking. Slow your pace for a cool-down toward the end of the walk (Table 6-1). Table 6-1 Stretching and flexing cannot be overemphasized for the nurse. • Before getting out of bed, start your day with stretching. Think of how a cat or dog stretches before they get busy with their activities. Follow their lead and prepare your sleepy muscles for the day by stretching while still in bed. • If the back muscles are feeling uncomfortable, lying on your back and drawing the knees to your chest may be helpful. Stay that way until you sense some relief. • The lower back may benefit from a low-back stretch. You are already lying flat with the previous exercise. Bend your knees slightly and keep your feet on the bed. Roll your knees to the side and back to the center. Reverse to the other side, keeping your back flat. • When ready to get up, roll to the side with your knees bent. Use your elbow and arms to push yourself up gently. This is much easier on the back than bolting upright or jumping out of bed. • If you work at a desk for much of the day, a small, latex-free hand exerciser in the shape of a ball can be squeezed when one hand is free. It is useful for strengthening the muscles in the lower arm and hand. • Even easier is to pick up something from the desk, such as a stapler, and flex your lower arm. • Resistive, nonlatex exercise tubing is color-coded according to the resistance desired. The tubing (or band) can be rolled up and takes limited space to transport. You can do any stretching exercise without it. The tubing just provides more resistance. • Improve circulation and prevent muscle cramps by doing a gentle, seated spinal twist. Sit up straight with your upper thighs at the edge of the seat. Cross your right leg over your left leg. Place your left hand on the inside of your left knee. Twist to the right as you exhale. Bring your right elbow or shoulder around toward the back of the chair. Hold the stretch for four to five breaths, twisting deeper when you exhale. Do this gently. Return to the starting position. Repeat in the opposite direction, crossing your left leg over your right leg, and so on. • Correct poor posture. Nurses often assume poor posture to do the work that they do. In fact, few of the tasks involved in direct patient care permit you to maintain good posture. Poor posture is hard on the spine, interferes with breathing, and increases the risk of shoulder and back pain. Stand up straight. Clasp your hands behind you at your buttocks. Press your shoulder blades toward each other. Have your elbows bent slightly. Breathe deeply, and then exhale. Press your knuckles toward the floor, straightening your arms. Do not arch forward; keep the back straight. Breathe in. Lift your chest, lengthening your spine. Straighten your arms a little as you exhale. Hold the stretch for five breaths. Release. After some practice, this stretching exercise will be easy to do and feel great on the back. • Deep breathing periodically throughout the shift helps to relieve tension in the lower back, neck, and shoulders. Place a hand on the abdomen and the other on the rib cage. Inhale deeply and feel the abdomen rise. As you exhale, feel the air move to the ribs and on up. Do this three to four times. • A head roll helps to relieve tension in the neck, upper shoulders, and back. Do not roll the head all the way around. Instead, drop your head down, roll the neck to the right over the shoulder, and then back to the left shoulder. Repeat, reversing the direction. • Back stretches while sitting stretch the back, neck, and arm muscles. Sit fully in a chair. Bring your torso over your knees and touch the floor with your hands. Sit up gently, raise your arms, and reach as high as you can with your fingers. Do this two to three times. • Relieve back pain by sitting on the edge of a chair. Bend forward slightly. Lift a weight you are comfortable with, first with one arm and then with the other. Repeat several times. • Side stretches may relieve tensed arm, hip, and lower back muscles. Stand with your feet apart. Hold a towel or tubing overhead and stretch your arms up and to the right side. Keep the hips still and facing front during the stretch. Switch sides and repeat. Body mechanics do help reduce the rate of nurse injury, but it is not enough by itself. Interestingly, body mechanics were based on studies with men. Yet, nursing remains primarily a female occupation. Women often have less upper-body strength than their male counterparts. Some of the early rationale was based on lifting boxes with handles, bending the knees, and keeping the back straight. In our experience, we have never had patients who came complete with handles for lifting! Other roadblocks are bedside clutter and small, confined spaces. Many nursing tasks involve unnatural positions, such as bending forward with the torso twisted. In their article, Nelson and colleagues offered the 16 most stressful handling tasks in order of rank (Box 6-1).
Personal Health Promotion
A Role Model for Patients
New Look at Nutrition and Health
Introduction to the MyPlate Icon
How-To Messages to Guide Healthy Eating
Making Time for Physical Activity
Moderate physical activity
Activity
Time
Bicycling
5 miles in 30 minutes
Walking
2 miles in 30 minutes
Social dancing (fast)
30 minutes
Swimming laps
20 minutes
Walking stairs
15 minutes
Gardening
30-45 minutes
Playing volleyball
45 minutes
Pushing stroller
1.5 miles in 30 minutes
Shooting baskets
30 minutes
Running
1.5 miles in 15 minutes
Raking leaves
30 minutes
Start the day with a stretch and flex
Making minimal effort pay off at work
Back Injuries in Nursing: What We Did Not Know
Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access