Chapter 40 The pelvic floor
After reading this chapter, you will:
Introduction
Perineal injury has occurred during childbirth throughout the ages and various methods and materials were used by accoucheurs in an attempt to restore the integrity of severely traumatized tissue. The earliest evidence of extensive perineal injury sustained during childbirth exists in the mummy of Henhenit, a Nubian woman aged approximately 22 years, from the harem of King Mentuhotep II of Egypt, 2050 BC (Derry 1935, Graham 1950, Magdi 1949). Despite the fact that maternity care has greatly improved over the past decade, women continue to suffer the consequences of pelvic floor damage resulting from childbirth.
The pelvic floor
The development of the upright posture in humans has been the dominant factor in the evolution of the pelvic floor (Benson 1992). Its main function is to provide support for the pelvic and abdominal organs and it must be strong to oppose the forces of gravity and increases in abdominal pressure. Childbirth is a known source of pelvic floor damage, causing muscle weakness, incontinence, and prolapse of the pelvic organs.
Structure
The ischial spines are key landmarks in understanding the location and structure of the pelvic floor. They lie laterally, in a plane which spans the pelvic cavity where many important parts of the pelvic floor are attached (Benson 1992). The soft tissues, which form the pelvic floor, fill the outlet of the bony pelvis forming a ‘sling’, which is higher posteriorly (Verralls 1993). In the female, the urethra, vagina, and rectum pass through its structures. It consists of the following six layers extending from the pelvic peritoneum above to the skin of the vulva, perineum, and buttocks below:
Pelvic fascia
This connective tissue fills the space between the pelvic organs lining the pelvic cavity walls. Its function is to provide support for the organs, whilst at the same time allowing them to move within the limits of normal function (Verralls 1993). In areas where extra support is needed, it thickens to form the pelvic ligaments:
 pass through the inguinal canal and anterior abdominal wall to become inserted into each labium majus
pass through the inguinal canal and anterior abdominal wall to become inserted into each labium majusDeep muscle layer
The deep muscles are named after the corresponding fused bones of the innominate bone (pubis, ilium and ischium) (Fig. 40.1):
 pass posteriorly below the bladder on either side of the urethra, upper vagina and anal canal to the anococcygeal body and coccyx
pass posteriorly below the bladder on either side of the urethra, upper vagina and anal canal to the anococcygeal body and coccyx fibres cross medially and join those from the opposite sides to form U-shaped slings around the urethra, vagina, and rectum
fibres cross medially and join those from the opposite sides to form U-shaped slings around the urethra, vagina, and rectum the puborectalis muscle forms a loop around the anorectal junction and its posterior fibres communicate with the external anal sphincter
the puborectalis muscle forms a loop around the anorectal junction and its posterior fibres communicate with the external anal sphincter on dissection, are paler in colour, suggesting they are fast-twitch muscle capable of rapid contraction (Benson 1992)
on dissection, are paler in colour, suggesting they are fast-twitch muscle capable of rapid contraction (Benson 1992) arise from the inner border of the white line of fascia on the inner aspects of the iliac bones and the ischial spines
arise from the inner border of the white line of fascia on the inner aspects of the iliac bones and the ischial spines arise from the ischial spines, pass downwards and inwards to be inserted into the coccyx and lower part of the sacrum
arise from the ischial spines, pass downwards and inwards to be inserted into the coccyx and lower part of the sacrum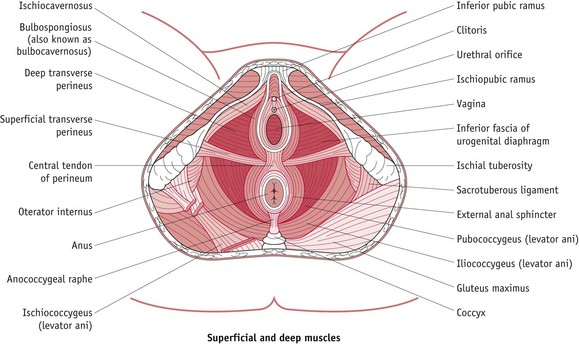
Figure 40.1 Muscles of the pelvic floor seen in the female perineum.
(From Principles of Anatomy and Physiology, 7th edn, by Tortora, G.J. and Grabowski, S.R.
Superficial perineal muscles
These are less important than the levator ani muscles; but contribute to the overall strength of the pelvic floor and likely to be damaged during vaginal delivery (Fig. 40.1):
 extend from central point in the perineal body, and encircle the vagina and urethra before inserting anteriorly into the corpora cavernosa of the clitoris
extend from central point in the perineal body, and encircle the vagina and urethra before inserting anteriorly into the corpora cavernosa of the clitoris situated beneath bulbocavernosus are the vestibular bulbs anteriorly and Bartholin’s glands posteriorly
situated beneath bulbocavernosus are the vestibular bulbs anteriorly and Bartholin’s glands posteriorly pass upwards and inwards along the pubic arch and are inserted into the corpora cavernosa of the clitoris
pass upwards and inwards along the pubic arch and are inserted into the corpora cavernosa of the clitoris fibres of each transverse muscle unite and interweave with the superficial tissue of the perineal body and external anal sphincter
fibres of each transverse muscle unite and interweave with the superficial tissue of the perineal body and external anal sphincterSphincters
 in females, the EAS is shorter anteriorly and fuses with the bulbocavernosus and transverse perinei in the lower part of the perineum (Sultan et al 1994a)
in females, the EAS is shorter anteriorly and fuses with the bulbocavernosus and transverse perinei in the lower part of the perineum (Sultan et al 1994a) the deep EAS is inseparable from the puborectalis muscle and posteriorly is attached to the coccyx by some of its fibres
the deep EAS is inseparable from the puborectalis muscle and posteriorly is attached to the coccyx by some of its fibres the circular striated (voluntary) muscle of the EAS, when dissected or torn, looks similar to ‘dark red meat’
the circular striated (voluntary) muscle of the EAS, when dissected or torn, looks similar to ‘dark red meat’Midwifery implications
Prolonged, repeated or extreme stretching of the pelvic floor muscles may cause permanent damage, resulting in loss of tone and elasticity. If these muscles fail to support the pelvic organs, prolapse results, though this may not manifest until later life when postmenopausal oestrogen deficiencies may predispose to muscle weakness (Haadem et al 1991). (For long term effects, please see website.)
Perineal trauma
Prevalence
Over 85% of women who have a vaginal birth will sustain some form of perineal trauma (McCandlish et al 1998) and up to 69% of these will require stitches (McCandlish et al 1998, Sleep et al 1984).
Rates will vary considerably according to individual practices and hospital policies throughout the world, illustrated by wide variations in episiotomy rates internationally from 8% in the Netherlands, 13% in England and 43% in the USA, to 99% in the Eastern European countries (Graham & Graham 1997, Graves 1995, Statistical Bulletin 2003, Wagner 1994).
Certain intrapartum interventions or alternative forms of care may also affect the rate and extent of perineal trauma; including continuous support during labour, delivery position, epidural anaesthesia, style of pushing, restricted use of episiotomy and ventouse delivery (Kettle 1999, 2001).
Aetiology and risk factors
Perineal trauma occurs during spontaneous or assisted vaginal delivery and is usually more extensive after the first vaginal birth (Sultan et al 1996). Women who have no visible damage may be subject to transient pudendal or peripheral nerve injury due to prolonged active pushing or pressure exerted by the fetal head on the surrounding structures (Allen et al 1990).
Associated risk factors include:
Short- and long-term effects
In the UK, approximately 23–42% of women will have perineal pain and discomfort up to 10–12 days following vaginal delivery and 7–10% of these women will continue to have long-term pain up to 18 months post partum (Glazener et al 1995, Gordon et al 1998, Grant et al 2001, McCandlish et al 1998, Mackrodt et al 1998, Sleep et al 1984).
In terms of sexual function, 62–88% of women will resume intercourse by 8–12 weeks postpartum, though 17–23% of women experience superficial dyspareunia at 3 months after delivery and 10–14% will continue to have pain at 12 months (Barrett et al 2000, Glazener 1997, Gordon et al 1998, Grant et al 2001, Kettle et al 2002, Mackrodt et al 1998).
Estimation of the extent of urinary and faecal incontinence is difficult because of under-reporting of these problems due to the sensitive nature of the complaint (Sultan et al 1996). One survey found that 15.2% of participating women (number 1782) reported stress incontinence which started for the first time within 3 months of the baby’s birth, and 75% of these still had problems over a year later (MacArthur et al 1993). Sleep & Grant (1987) and MacArthur et al (1997) found that up to 4% of women reported occasional loss of bowel control.








































