Patient Safety
Objectives
• Discuss the importance of consensus standards for public reporting of patient safety events.
• Describe environmental hazards that pose risks to a person’s safety.
• Discuss methods to reduce physical hazards and the transmission of pathogens.
• Discuss the specific risks to safety related to developmental age.
• Identify the factors to assess when a patient is in restraints.
• Describe the four categories of safety risks in a health care agency.
• Identify relevant nursing diagnoses associated with risks to safety.
• Develop a nursing care plan for patients whose safety is threatened.
• Define the knowledge, skills, and attitudes necessary to promote safety in a health care setting.
Key Terms
Aura, p. 387
Food and Drug Administration (FDA), p. 366
Immunization, p. 367
Pathogen, p. 367
Poison, p. 367
Pollutant, p. 368
Restraint, p. 384
Seizure, p. 387
Seizure precautions, p. 387
Status epilepticus, p. 387
![]()
Safety, often defined as freedom from psychological and physical injury, is a basic human need. Health care provided in a safe manner and a safe community environment is essential for a patient’s survival and well-being. A safe environment reduces the risk for illness and injury and helps to contain the cost of health care by preventing extended lengths of treatment and/or hospitalization, improving or maintaining a patient’s functional status, and increasing the patient’s sense of well-being. The Institute of Medicine’s report To Err Is Human: Building a Safer Health System (2000) was a pivotal publication that brought patient safety to the forefront of health care in the United States. This report indicated that 44,000 to 98,000 people die each year as a result of preventable medical errors. In an effort to improve patient safety, many organizations have become devoted to developing and monitoring key health care safety initiatives and providing information to health care organizations and the public. Health care organizations foster a patient-centered safety culture by continually focusing on performance improvement endeavors, risk management findings, and safety reports; providing current reliable technology; integrating evidence-based practice into procedures; designing a safe work environment and atmosphere; and providing continuing education and access to appropriate resources for staff (Box 27-1). As part of the health care team, the nurse has the professional responsibility to be engaged in activities that support a patient-centered safety culture. Considerable emphasis has also been placed on improving the education of student nurses so they become more competent in promoting safe health care practices. The Quality and Safety Education for Nurses (QSEN) project was developed to meet the challenge of preparing future nurses who will have the knowledge, skills, and attitudes necessary to continuously improve the quality and safety of the health care systems within which they work (QSEN, 2011). The QSEN safety competency for a nurse is defined as “Minimizes risk of harm to patients and providers through both system effectiveness and individual performance.” As a nurse you are responsible for incorporating critical thinking skills when using the nursing process, assessing each patient and his or her environment for hazards that threaten safety, and planning and intervening appropriately to maintain a safe environment. By doing this, you become a provider of safe acute, restorative, and continuing care and an active participant in health promotion.
Scientific Knowledge Base
Environmental Safety
A patient’s environment includes all of the many physical and psychosocial factors that influence or affect the life and survival of that patient. This broad definition of environment crosses the continuum of care for settings in which the nurse and patient interact such as the hospital, long-term care facility, clinic, community center, school, and home. A safe environment protects the staff as well, allowing them to function optimally. Vulnerable groups who often require help in achieving a safe environment include infants, children, older adults, the ill, the physically and mentally disabled, the illiterate, and the poor. A safe environment includes meeting basic needs, reducing physical hazards and the transmission of pathogens, and controlling pollution.
Basic Needs.
Physiological needs, including the need for sufficient oxygen, nutrition, and optimum temperature, influence a person’s safety. According to Maslow’s hierarchy of needs, these basic needs must be met before physical and psychological safety and security can be addressed (see Chapter 6).
Oxygen.
Supplemental oxygen is sometimes required to meet a person’s oxygenation needs. Oxygen is not flammable, but fire needs oxygen to start and to keep burning. When more oxygen is in the air, a fire burns hotter and faster. Strict codes regulate the use and storage of medical oxygen in health care facilities. This is not necessarily true in the home environment. Hospital emergency departments see approximately 1190 thermal burns per year caused by ignitions associated with home medical oxygen (National Fire Protection Association, 2008). Smoking is by far the leading cause of burns, reported fires, deaths, and injuries involving home medical oxygen.
Be aware of factors in a patient’s environment that decrease the amount of available oxygen. A common environmental hazard in the home is an improperly functioning heating system. A furnace, stove, or fireplace that is not properly vented introduces carbon monoxide into the environment. Carbon monoxide affects a person’s oxygenation by binding with hemoglobin, preventing the formation of oxyhemoglobin and thus reducing the supply of oxygen delivered to tissues (see Chapter 40). Low concentrations cause nausea, dizziness, headache, and fatigue. Very high concentrations cause death after 1 to 3 minutes of exposure (National Fire Protection Association, 2010a).
Nutrition.
Meeting nutritional needs adequately and safely requires environmental controls and knowledge (see Chapter 44). Health care facilities and restaurants are required to meet State Board of Health regulations. To protect consumers, commercially processed and packaged foods are subject to Food and Drug Administration (FDA) regulations. The FDA is a federal agency responsible for the enforcement of federal regulations regarding the manufacture, processing, and distribution of foods, drugs, and cosmetics to protect consumers against the sale of impure or dangerous substances. Although food supply in the United States is one of the safest in the world, each year about 76 million illnesses occur, more than 300,000 persons are hospitalized, and 5,000 die from foodborne illness (Centers for Disease Control and Prevention, 2009). Groups at the highest risk are children, pregnant women, older adults, and people with compromised immune systems. Foods that are inadequately prepared or stored or subject to unsanitary conditions increase the patient’s risk for infections and food poisoning.
Temperature.
A person’s comfort zone is usually between 18.3° and 23.9° C (65° and 75° F). Temperature extremes that frequently occur during the winter and summer affect comfort, productivity, and safety. Exposure to severe cold for prolonged periods causes frostbite and accidental hypothermia. Frostbite occurs when a surface area of the skin freezes as a result of exposure to extremely cold temperatures. Hypothermia occurs when the core body temperature is 35° C (95° F) or below. Older adults, the young, patients with cardiovascular conditions, patients who have ingested drugs or alcohol in excess, and people who are homeless are at high risk for hypothermia. Exposure to extreme heat changes the electrolyte balance of the body and raises the core body temperature, resulting in heatstroke or heat exhaustion. Chronically ill patients, older adults, and infants are at greatest risk for injury from extreme heat. These patients need to avoid extremely hot, humid environments (see Chapter 29).
Physical Hazards.
On average 33.5 million injuries take place each year, with the majority occurring inside or outside of the home (Centers for Disease Control and Prevention, 2010a). Physical hazards in the environment threaten a person’s safety and often result in physical or psychological injury or death. Unintentional injuries are the fifth leading cause of death for Americans of all ages (National Center for Injury Prevention, 2010a). Motor vehicle accidents are the leading cause, followed by poisonings and falls. Additional hazards consist of fire and disasters. A nurse plays a role in educating patients about common safety hazards and how to prevent injury while placing emphasis on hazards to which patients are more vulnerable.
Motor Vehicle Accidents.
Vehicle design and equipment such as seat belts, air bags, and laminated windshields (remain in one piece when impacted) have improved safety for vehicle occupants. State specific laws relating to young driver licensing, safety belt use, child restraint use, and motorcycle helmets exist for protection. Child safety seats and booster seats appropriate for the child’s age and weight and the type of car need to be used (Fig. 27-1). The American Academy of Pediatrics (2011) recommends that all infants and toddlers ride in the back seat with a rear-facing car safety seat until they are 2 years of age or they reach the highest weight or height allowed by the manufacturer of the car safety seat. The website of the Academy, Healthy Children, http://www.aap.org/healthtopics/carseatsafety.cfm, has information for children of all ages and the type of safety seat to use. The back seat of a car is the safest part of the vehicle in the event of a crash and prevents injury from deployment of passenger and side air bags. According to the Centers for Disease Control and Prevention (2010b), the risk of motor vehicle accidents is higher among 16- to 19-year-old drivers than any other age-group. Teens are more likely to underestimate dangerous situations or not be able to recognize hazardous situations, speed and allow shorter headways, ride with intoxicated drivers, and drive after using alcohol and drugs. Teens also have the lowest rate of seat belt use. Older drivers are keeping their licenses longer and driving more miles than in the past. Per mile traveled, fatal crash rates increase starting at age 75 and increase markedly after age 80 (Insurance Institute for Highway Safety, 2008). An older adult is not always able to quickly observe situations in which an accident is likely to occur. Decreased hearing acuity alters the ability to hear emergency vehicle sirens or vehicle horns. Because of decreased nervous system response, older adults are unable to react as quickly as they once could to avoid an accident. A decline in these skills accounts for the most common types of accidents, including right-of-way and turning accidents.
Poison.
A poison is any substance that impairs health or destroys life when ingested, inhaled, or absorbed by the body. Almost any substance is poisonous if too much is taken. Sources in a person’s home include drugs, medicines, other solid and liquid substances, and gases and vapors. Poisons often impair the function of every major organ system. Health care providers are at risk from chemicals such as toxic cleaning agents. In the home accidental poisoning is a greater risk for toddlers, preschoolers, and young school-age children, who often ingest household cleaning solutions, medications, or personal hygiene products. Emergency treatment is necessary when a person ingests a poisonous substance or comes in contact with a chemical that is absorbed through the skin. In 2008 more than 2000 people a day were seen in emergency departments after a poison incident (Centers for Disease Control and Prevention, 2010c). Specific antidotes or treatments are available only for some types of poisons. A poison control center is the best resource for patients and parents needing information about the treatment of an accidental poisoning.
Although lead has not been used in house paint or plumbing materials since the U.S. Consumer Product Safety Commission banned it in 1978, older homes in poorer communities continue to contain high lead levels. Soil and water systems are sometimes contaminated. Poisoning occurs from swallowing or inhaling lead. Fetuses, infants, and children are more vulnerable to lead poisoning than adults because their bodies absorb lead more easily and small children are more sensitive to the damaging effects of lead. Exposure to excessive levels of lead affects a child’s growth or causes learning and behavioral problems and brain and kidney damage (Agency for Toxic Substances and Disease Registry, 2010).
Falls.
Falls are a major public health problem. Among adults 64 years and older, falls are the leading cause of unintentional death (Centers for Disease Control and Prevention, 2010a). Numerous factors increase the risk of falls, including a history of falling, being age 65 or over, reduced vision, orthostatic hypotension, gait and balance problems, urinary incontinence, use of walking aids, and the effects of various medications (e.g., anticonvulsants, hypnotics, sedatives, certain analgesics) (Deandrea et al., 2010). Common physical hazards that lead to falls include inadequate lighting, barriers along normal walking paths and stairways, and a lack of safety devices in the home. Often a fall leads to serious injury such as fractures or internal bleeding. Patients most at risk for injury are those with bleeding tendencies resulting from disease or medical treatments and osteoporosis. Injuries frequently result from accidental contact with objects on stairs, floors, bedside tables, closet shelves, refrigerator tops, and bookshelves. Children fall from anywhere (i.e., trees, wall/fences, playground equipment, furniture, and moving objects such as skateboards and bicycles). Forces from falls lead to injury with variable severity, depending on the height of the fall, body position on impact, and impact surface.
Fire.
A total of 386,500 home fires were reported in the United States in 2008, resulting in 2,755 deaths and 13,160 injuries (National Fire Protection Association, 2010b). The leading cause of fire-related death is careless smoking, especially when people smoke in bed at home. The improper use of cooking equipment and appliances, particularly stoves, is the main source for in-home fires and fire injuries. Smoke detectors and carbon monoxide detectors need to be placed strategically throughout a home. Multipurpose fire extinguishers need to be near the kitchen and any workshop areas.
Disasters.
When they strike, natural disasters such as floods, tsunamis, hurricanes, tornadoes, and wildfires are a major cause of death and injury. These types of disasters result in death and leave many people homeless. Every year millions of Americans face disaster and its terrifying consequences (FEMA, 2010). Bioterrorism is another cause of disaster. Threats of this type come in the form of biological, chemical, and radiological attacks. Bioterrorism, or the use of biological agents to create fear and threat, is the most likely form of a terrorist attack to occur. Although terrorists could use any agent, health officials are most concerned with biological agents such as anthrax, smallpox, pneumonic plague, botulism, tularemia, and viral hemorrhagic fevers (American Medical Association, 2010).
Transmission of Pathogens.
Pathogens and parasites pose a threat to patient safety (see Chapter 28). A pathogen is any microorganism capable of producing an illness. The most common means of transmission of pathogens is by the hands. For example, if an individual infected with hepatitis A does not wash his or her hands thoroughly after having a bowel movement, the risk for transmitting the disease during food preparation is great. One of the most effective methods for limiting the transmission of pathogens is the medically aseptic practice of hand hygiene (see Chapter 28). The human immunodeficiency virus (HIV), the pathogen that causes acquired immunodeficiency syndrome (AIDS), and the hepatitis B virus are transmitted through blood and other select body fluids. High-risk behaviors that include sexual contact and drug use are common risk factors for HIV. People who abuse drugs often share syringes and needles, which increase the risk of acquiring these viruses. Some states and many nonprofit organizations fund syringe exchange programs as a means to slow down the spread of infectious diseases obtained through needle sharing (Coalition for Safe Community Needle Disposal, 2010).
Immunization also reduces, and in some cases prevents, the transmission of disease from person to person. Individuals acquire active immunity by an injection of a small amount of attenuated (weakened) or dead organisms or modified toxins from the organism (toxoids) into the body. Passive immunity occurs when antibodies produced by other persons or animals are introduced into a person’s bloodstream for protection against a pathogen.
Insects and rodents often carry pathogens. For example, some mosquitoes are carriers of malaria and West Nile virus. Rats and mice carry rat-bite fever. Uncontrolled mosquito and rodent populations increase the risk for these diseases. People living at the poverty level sometimes live in unmaintained homes or housing. Rat and roach infestations are common problems. Mosquito repellant and rodent traps help eliminate this risk.
Proper disposal of human waste controls the transmission of disease and parasites. Without a satisfactory sewer and waste system in a community, the population is at risk for illnesses such as typhoid fever and hepatitis.
Pollution.
A healthy environment is free of pollution. A pollutant is a harmful chemical or waste material discharged into the water, soil, or air. People commonly think of pollution only in terms of air, land, or water pollution; but excessive noise is also a form of pollution that presents health risks. Air pollution is the contamination of the atmosphere with a harmful chemical. Prolonged exposure to it increases the risk of pulmonary disease. In urban areas industrial waste and vehicle exhaust are common contributors to air pollution. In the home, school, or workplace, cigarette smoke is the primary cause of air pollution. Improper disposal of radioactive and bioactive waste products (e.g., dioxin) can cause land pollution. Water pollution is the contamination of lakes, rivers, and streams, usually by industrial pollutants. Water treatment facilities filter harmful contaminants from the water, but these systems sometimes contain flaws. If water becomes contaminated, the public needs to use bottled or boiled water for drinking and cooking. Flooding frequently causes damage to water treatment stations and also requires the use of bottled or boiled water.
Nursing Knowledge Base
Factors Influencing Patient Safety
In addition to being knowledgeable about the home and health care environment and the inherent safety risks, nurses need to be familiar with a patient’s developmental level; mobility, sensory, and cognitive status; lifestyle choices; and knowledge of common safety precautions. They also need to be aware of the special risks to safety that are found in health care settings.
Risks at Developmental Stages.
A patient’s developmental stage creates threats to safety as a result of lifestyle, cognitive and mobility status, sensory impairments, and safety awareness. With this information, you tailor safety prevention programs to the needs, preferences, and life circumstances of particular age-groups. Unfortunately all age-groups are subject to abuse. Child abuse, domestic violence, and elder abuse are serious threats to safety. Chapters 12 through 14 discuss these topics.
Infant, Toddler, and Preschooler.
Injuries are the leading cause of death in children over age 1 and cause more death and disabilities than do all diseases combined (Hockenberry and Wilson, 2009). The nature of the injury sustained is closely related to normal growth and development. For example, the incidence of lead poisoning is highest in late infancy and toddlerhood. Children at this stage explore the environment and, because of their increased level of oral activity, put objects in their mouth. This increases risk for poisoning and choking. Fire often results from their curiosity in playing with matches. In addition, limited physical coordination contributes to falls from bicycles and playground equipment. Additional injuries at this age are related to riding unrestrained in a motor vehicle, drowning, and head trauma from objects. Accidents involving children are largely preventable, but parents need to be aware of specific dangers at each stage of growth and development. Accident prevention thus requires health education for parents and the removal of dangers whenever possible.
School-Age Child.
When a child enters school, the environment expands to include the school, transportation to and from school, school friends, and after-school activities. School-age children are learning how to perform more complicated motor activities and often are uncoordinated. Parents, teachers, and nurses need to instruct children in safe practices to follow at school or play, including what to do if approached by strangers. Teach school-age children involved in team and contact sports the rules for playing safely and how to use protective safety equipment such as helmets and other protective gear. Head injuries are a major cause of death, with bicycle accidents being one of the major causes of such injuries (Hockenberry and Wilson, 2009). Bikes need to be the proper size for the child, and helmets must be worn (Fig. 27-2). Additional injuries in this age-group are decreased by properly using seat belts and booster seats in motor vehicles and providing pedestrian safety education.
Adolescent.
As children enter adolescence, they develop greater independence and begin to develop a sense of identity and their own values. The adolescent begins to separate emotionally from his or her family, and peers generally have a stronger influence. Wide variations that swing from childlike to mature behavior are characteristic of adolescent behavior (Hockenberry and Wilson, 2009). In an attempt to relieve the tensions associated with physical and psychosocial changes and peer pressures, some adolescents engage in risk-taking behaviors such as smoking, drinking alcohol, and using drugs. This increases the incidence of accidents such as drowning and motor vehicle accidents. When adolescents learn to drive, their environment expands, and so does their potential for injury. Fortunately teen motor vehicle crashes are preventable by avoiding distractions such as using cell phones, texting, eating, and drinking while driving.
To assess for possible substance abuse, have parents look for environmental and psychosocial clues from their children. Environmental clues include the presence of drug-oriented magazines, beer and liquor bottles, drug paraphernalia and blood spots on clothing and the continual wearing of long-sleeved shirts in hot weather and dark glasses indoors. Psychosocial clues include failing grades, change in dress, increased absenteeism from school, isolation, increased aggressiveness, and changes in interpersonal relationships. Because adolescence is a time when mature sexual physical characteristics develop, some adolescents begin to have physical relationships with others that present the risk of sexually transmitted diseases.
Adult.
The threats to an adult’s safety are frequently related to lifestyle habits. For example, a person who uses alcohol excessively is at greater risk for motor vehicle accidents. People who smoke long-term have a greater risk of cardiovascular or pulmonary disease as a result of the inhalation of smoke and the effect of nicotine on the circulatory system. Likewise, the adult experiencing a high level of stress is more likely to have an accident or illness such as headaches, gastrointestinal (GI) disorders, and infections.
Older Adult.
The physiological changes associated with aging, effects of multiple medications, psychological factors, and acute or chronic disease increase the older adult’s risk for falls and other types of accidents. Falls often result in bruises, hip fractures, or head trauma. The risk of being seriously injured in a fall increases with age. Older patients are more likely to fall in the bedroom, bathroom, and kitchen. Environmental factors such as broken stairs, icy sidewalks, inadequate lighting, throw rugs, and exposed electrical cords cause many of the accidents. Inside falls most often occur while transferring from beds, chairs, and toilets; getting into or out of bathtubs; tripping over items such as cords covered by rugs or carpets, carpet edges, or doorway thresholds; slipping on wet surfaces; and descending stairs. Fear of falling is a concern of community-dwelling older adults, and many avoid activities because of their fear (Zijlstra et al., 2007). Falls can be decreased by multiple-component group exercise, Tai Chi, having a physician or pharmacist review all medications, having an eye examination annually, and decreasing hazards in the home that increase falls (Gillespie et al., 2009).
Individual Risk Factors.
Other risk factors posing threats to safety include lifestyle, impaired mobility, sensory or communication impairment, and the lack of safety awareness.
Lifestyle.
Some lifestyle choices increase safety risks. People who drive or operate machinery while under the influence of chemical substances (drugs or alcohol), work at inherently dangerous jobs, or are risk takers are at greater risk of injury. In addition, people experiencing stress, anxiety, fatigue, or alcohol or drug withdrawal or those taking prescribed medications are sometimes more accident prone. Because of these factors, some people are too preoccupied to notice the source of potential accidents such as cluttered stairs or a stop sign.
Impaired Mobility.
A patient with impaired mobility has many kinds of safety risks. Muscle weakness, paralysis, and poor coordination or balance are major factors in falls. Immobilization predisposes patients to additional physiological and emotional hazards, which in turn further restrict mobility and independence. Persons who are physically challenged are at greater risk for injury when entering motor vehicles and buildings that are not handicapped accessible.
Sensory or Communication Impairment.
Cognitive impairments associated with delirium, dementia, and depression place patients at greater risk for injury. These conditions contribute to altered concentration and attention span, impaired memory, and orientation changes. Patients with these alterations become easily confused about their surroundings and are more likely to have falls and burns. Patients with visual, hearing, tactile, or communication impairment such as aphasia or a language barrier are not always able to perceive a potential danger or express their need for assistance (see Chapter 49).
Lack of Safety Awareness.
Some patients are unaware of safety precautions such as keeping medicine or poisons away from children or reading the expiration date on food products. A complete nursing assessment, including a home inspection, helps you identify the patient’s level of knowledge regarding home safety so you can correct deficiencies with an individualized nursing care plan.
Risks in the Health Care Agency.
Patient safety continues to be one of the most pressing health care challenges in the nation. Medical errors are the eighth leading cause of death (Agency for Healthcare Research and Quality, 2010). Medical errors happen when something that was planned as part of medical care doesn’t work out or when the wrong plan was used. They occur in all health care settings. You must be aware of regulatory and organizational safety initiatives and individual patient risk factors. The Joint Commission (TJC) and the Centers for Medicare and Medicaid Services (CMS) have placed an increased emphasis on error prevention and patient safety. Their “Speak Up” campaign encourages patients to take a role in preventing health care errors by becoming active, involved, and informed participants on the health care team. For example, patients are encouraged to ask health care workers if they have washed their hands before providing care. National Patient Safety Goals of TJC (2011b) are specifically directed to reduce the risk of medical errors (Box 27-2). The goals are designed to promote specific improvements in patient safety and highlight ongoing problematic areas in health care. These evidence-based recommendations require health care facilities to focus their attention on a series of specific actions.
The National Quality Forum (NQF) (2011a) has the mission of improving the quality of health care in America by:
• Endorsing national consensus standards for measuring and publicly reporting on performance; and
• Promoting the attainment of national goals through education and outreach programs.
Recently the NQF released its National Voluntary Consensus Standards for Public Reporting of Patient Safety Events (NQF, 2011b). The report provides a framework for publicly reporting patient safety information—including events, indicators, and measures—about health care organizations to consumers. It is important for nurses to understand the NQF standards and their intent since ultimately they influence the types of priorities that patient care organizations (e.g., hospitals, community health centers) set to improve the quality of care delivered to patients. Many of the NQF measures of patient safety (e.g., patient falls with injury, incidence of pressure ulcers, and central line bloodstream infection) are standards for judging the quality of care of health care organizations. The measures are also used by other organizations such as TJC and the CMS. Among the safety measures, the NQF endorsed a select list of serious reportable events (SREs), which was updated in 2006. The 28 events (Box 27-3) are a major focus of health care providers for patient safety initiatives. The CMS names select SREs as Never Events (i.e., adverse events that should never occur in a health care setting) (Department of Health and Human Services, 2008). The CMS now denies hospitals higher payment for any hospital-acquired condition resulting from or complicated by the occurrence of certain Never Events (Box 27-4). Many of the hospital-acquired conditions (e.g., fall or stage III pressure ulcer) are nurse-sensitive indicators, meaning that a nurse directly affects their development. The NQF (2010) also released 34 safe practices for better health care. Evidence supports the effectiveness of these practices in reducing the occurrence of adverse health care events.
Being aware of and engaged in activities focused on the prevention of these conditions not only enhances patient safety but also contributes to the overall success of the health care facility. The CMS believes that the Never Events will strengthen incentives by hospitals to develop safety practices and reduce health care costs in the long term. Health care facilities often conduct a failure mode and effect analysis (FMEA) to identify problems with processes and products before they occur.
When an actual or potential adverse event occurs, the nurse or health care provider involved completes an incident or occurrence report. An incident report is a confidential document that completely describes any patient accident occurring on the premises of a health care agency (see Chapter 23). Reporting allows the organization to identify trends/patterns throughout the facility and areas to improve. Focusing on the root cause of an event instead of the individual involved promotes a “culture of safety” that helps in specifically identifying what contributed to an error. The probability of an accident occurring declines with adherence to evidence-based principles of safety (Taylor-Adams et al., 2009).
Nurses face specific environmental risks in health care facilities. An example is the various forms of chemicals used. Chemicals found in some medications (e.g., chemotherapy), anesthetic gases, cleaning solutions, and disinfectants are potentially toxic if ingested, absorbed into the skin, or inhaled. Material safety data sheets (MSDSs) are required resources available in any health care agency (Occupational Safety and Health Administration, 1996). The MSDS provides detailed information about the chemical, health hazards imposed, first aid guidelines, and precautions for safe handling and use. MSDSs give information on the steps to take in case the material is released or spilled. Be aware of the location of the MSDSs and be knowledgeable about hazardous chemicals in your environment. Spread of pathogens also presents a risk to both nurses and other patients. Therefore always follow standard and transmission-based isolation precautions, along with proper hand hygiene (see Chapter 28).
Specific risks to a patient’s safety within the health care environment include falls, patient-inherent accidents, procedure-related accidents, and equipment-related accidents. The nurse assesses for these four potential problem areas and, considering the developmental level of the patient, takes steps to prevent or minimize accidents.
Falls.
Falls result in minor to severe injuries such as hip fractures or head trauma that result in reduced mobility and independence and increase the risk for premature death. Patients who have underlying disease states are more susceptible to fall-related injuries (Hughes, 2008). For example, a patient with a bleeding disorder is more likely to have an intracranial bleed; a patient with osteoporosis has a greater chance for fracture. The unfamiliar environment, acute illness, surgery, mobility status, medications, treatments, and placement of various tubes and catheters are common challenges that place patients of any age at risk of falling. Factors the nurse can influence include assessment and communication about patient risks, information access, signage, the environment, teamwork, and involving the patient and family (Dykes et al., 2009). Falls that result in injuries often extend a patient’s length of stay in the health care environment, placing them at an even greater risk for other complications.
Patient-Inherent Accidents.
Patient-inherent accidents are accidents (other than falls) in which the patient is the primary reason for the accident. Examples include self-inflicted cuts, injuries, and burns; ingestion or injection of foreign substances; self-mutilation or fire setting; and pinching fingers in drawers or doors. One of the more common precipitating factors for a patient-inherent accident is a seizure.
Procedure-Related Accidents.
Procedure-related accidents are caused by health care providers and include medication and fluid administration errors, improper application of external devices, and accidents related to improper performance of procedures such as dressing changes or urinary catheter insertion. Nurses are able to prevent many procedure-related accidents by adhering to organizational policy and procedures and standards of nursing practice. For example, proper preparation and administration of medications, use of patient and medication bar coding, and “Smart” intravenous (IV) pumps reduce medication errors (see Chapters 31 and 41). All staff need to be aware that distractions and interruptions contribute to procedure-related accidents and need to be limited, especially during high-risk procedures such as medication administration. The potential for infection is reduced when surgical asepsis is used for sterile dressing changes or any invasive procedure such as insertion of a urinary catheter. Finally, correct use of safe patient handling techniques and equipment reduces the risk of injuries when moving and lifting patients (see Chapter 47).
Equipment-Related Accidents.
Accidents that are equipment related result from the malfunction, disrepair, or misuse of equipment or from an electrical hazard. To avoid rapid infusion of IV fluids, all general-use and patient-controlled analgesic pumps need to have free-flow protection devices. To avoid accidents, do not operate monitoring or therapy equipment without adequate instruction. If faulty equipment is discovered, place a tag on it to prevent it from being used on another patient and promptly report any malfunctions. Assess potential electrical hazards to reduce the risk of electrical fires, electrocution, or injury from faulty equipment. In health care settings the clinical engineering staff make regular safety checks of equipment. Facilities must report all suspected medical device—related deaths to both the FDA and the manufacturer of the product if known (FDA, 2009). This is usually done in conjunction with the risk management department after tagging and removing the piece of equipment.
Critical Thinking
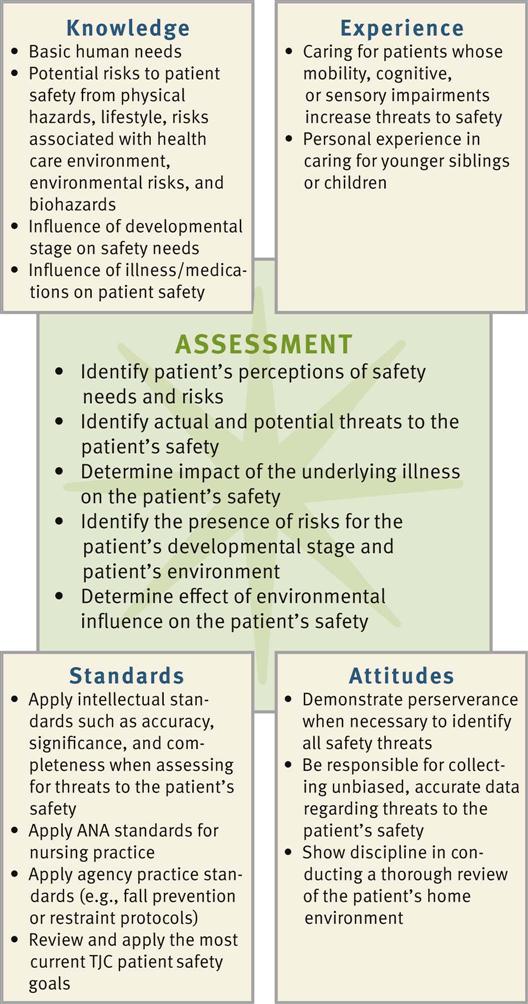
Successful critical thinking requires a synthesis of knowledge, experience, information gathered from patients, critical thinking attitudes, and intellectual and professional standards. Clinical judgments require the nurse to anticipate necessary information, analyze the data, and make decisions regarding patient care. Critical thinking is an ongoing process. During assessment (Fig. 27-3) you consider all critical thinking elements and information about the specific patient to make appropriate nursing diagnoses.
In the case of safety, the nurse integrates knowledge from nursing and other scientific disciplines, previous experiences in caring for patients who had an injury or were at risk, critical thinking attitudes such as responsibility and discipline, and any standards of practice that are applicable. For example, the American Nurses Association (ANA) standards for nursing practice address the nurse’s responsibility in maintaining patient safety. TJC (2011b) also provides standards for safety. You refer to all of this information and experience as you conduct a detailed assessment of a specific patient. For example, while assessing a specific patient’s home environment, you consider typical locations within the home where dangers commonly exist. If a patient has a visual impairment, you apply previous experiences in caring for patients with visual changes to anticipate how to thoroughly assess his or her needs. Critical thinking directs you to anticipate what needs to be assessed and how to make conclusions about available data.
Nursing Process
Apply the nursing process and use a critical thinking approach in your care of patients. The nursing process provides a clinical decision-making approach for you to develop and implement an individualized plan of care.
Assessment
During the assessment process thoroughly assess each patient and critically analyze findings to ensure that you make patient-centered clinical decisions required for safe nursing care.
Through the Patient’s Eyes.
Patients generally expect to be safe in health care settings and in their homes. However, there are times when a patient’s view of what is safe does not agree with that of the nurse and the standards he or she hopes to enforce. For this reason your assessment needs to be patient centered and include the patient’s own perceptions of his or her risk factors, knowledge of how to adapt to such risks, and previous experience with any accidents. This is important if you need to make changes in the patient’s environment. Patients usually do not purposefully put themselves in jeopardy. When they are uninformed or inexperienced, threats to their safety occur. You always need to consult patients or family members about ways to reduce hazards in their environment. To conduct a thorough patient assessment, consider possible threats to a patient’s safety, including the immediate environment and any individual risk factors. Ask the patient specific questions related to safety (Box 27-5).
Nursing History.
A nursing history includes data about a patient’s level of wellness to determine if any underlying conditions exist that pose threats to safety. For example, give special attention to assessing a patient’s gait, lower-body muscle strength and coordination, balance, and vision. Consider a review of the patient’s developmental status as you analyze assessment information. Also review if the patient is taking any medications or undergoing any procedures that pose risks. For example, use of diuretics increases the frequency of voiding and results in the patient having to use toilet facilities more often. Falls often occur with patients who have to get out of bed quickly because of urinary urgency.
Health Care Environment.
When the patient is cared for within a health care facility, you need to determine if any hazards exist in the immediate care environment. Does the placement of equipment (e.g., drainage bags, IV pumps) or furniture pose barriers when the patient attempts to ambulate? Does positioning of the patient’s bed allow him or her to easily reach items on a bedside table or stand? Does the patient need assistance with ambulation? Are there multiple tubes or IV lines? Is the call bell within reach? The nurse collaborates with clinical engineering staff to make sure that equipment functions properly and is in good condition.
Risk for Falls.
Assessment of a patient’s risk factors for falling is essential in determining specific needs and developing targeted interventions to prevent falls. Many different fall assessment instruments are available; use the tool chosen by your health care agency. A fall assessment tool (Table 27-1) helps you assess important risk factors. At a minimum the assessment needs to be completed on admission, following a change in the patient’s condition, after a fall, and when transferred. If it is determined that the patient is at risk for falling, regular assessment always continues. In many cases family members are important resources in assessing a patient’s fall risk. Families often are able to report on the patient’s level of confusion and ability to ambulate. Based on the results of a fall risk assessment, you implement multiple evidence-based interventions. It is very important to inform a patient and family members about the patient’s risks. Often younger patients are not aware of how medications and treatments cause dizziness, orthostatic hypotension, or changes in balance. When patients are unaware of their risks, they are less likely to ask for assistance. If family members are informed, they will often call for help (when they are visiting patients) to be sure that patients are appropriately assisted.
TABLE 27-1
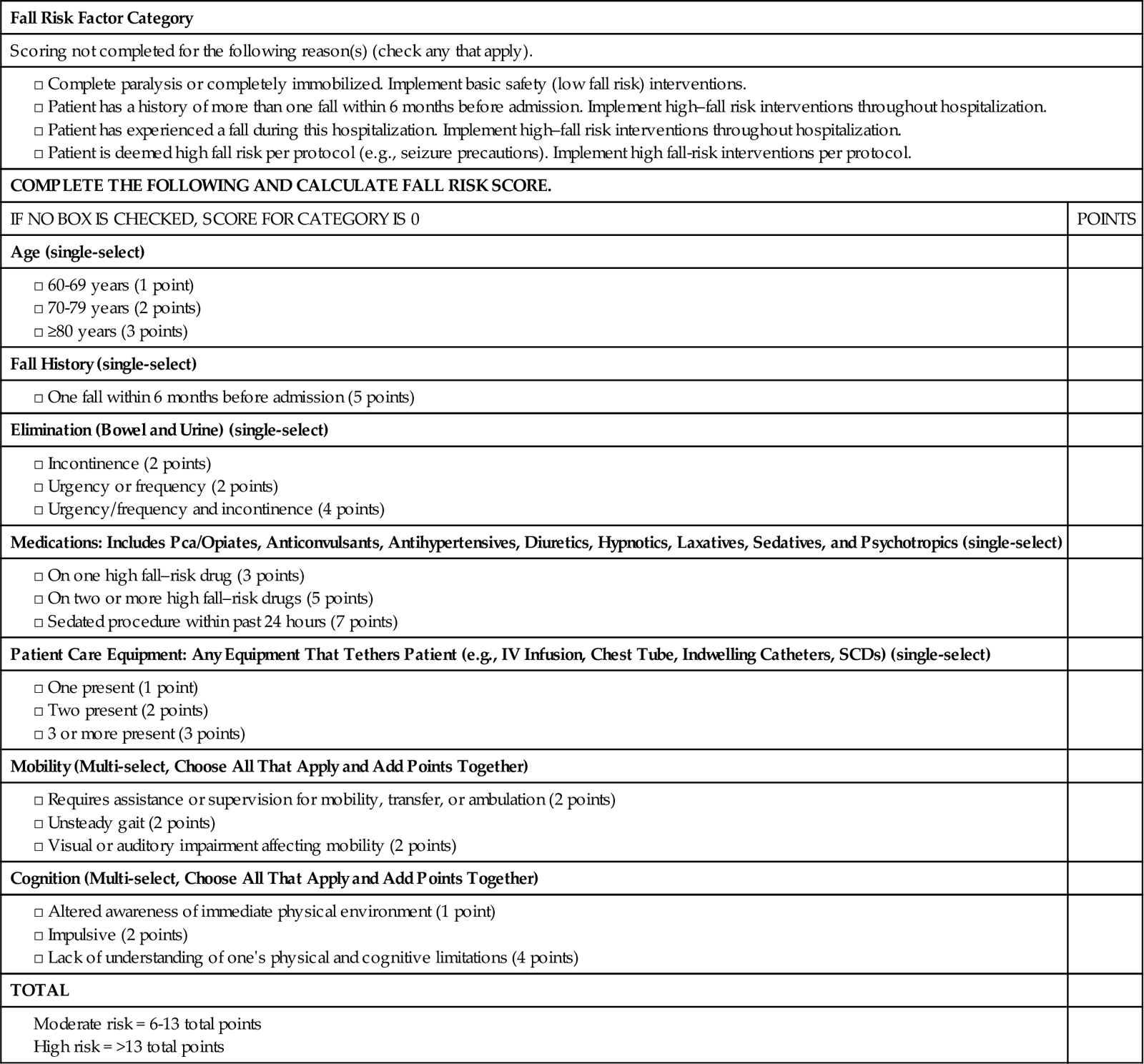
Copyright © 2007 by The Johns Hopkins Health System Corporation. All rights reserved.
IV, Intravenous.
Risk for Medical Errors.
Be alert to factors within your own work environment that create conditions in which medical errors are more likely to occur. Studies show that overwork and fatigue cause a significant decrease in alertness and concentration, leading to errors (Trinkoff et al., 2006). It is important for you to be aware of these factors and include checks and balances when working under stress. For example, to reduce the potential for a medical error, it is essential for you to check the patient’s identification by using two identifiers (e.g., name and birthday or name and account number) according to facility policy before beginning any procedure or administering a medication (see Chapter 31).
Disasters.
Hospitals must be prepared to respond and care for a sudden influx of patients at the time of a community disaster. Guidelines for a disaster response are included in a facility emergency management plan. All hospitals conduct disaster drills on a routine basis. Communication is a key to any emergency management plan. Nurses must know what happened, how many patients to expect, and when patients will begin to arrive so they can prepare both themselves and their facility. Although the occurrence of a bioterrorist attack has been limited to the anthrax deaths following September 11, 2001, the threat is very real. Be prepared to make accurate and timely assessments in any type of setting. A bioterrorist attack will likely resemble a natural outbreak initially. Acutely ill patients representing the earliest cases after a covert attack seek care in emergency departments. Patients less ill at the onset of an illness possibly seek care in primary care settings. Basic epidemiological principles exist to assess whether a patient’s presentation of symptoms is typical of an endemic disease or an unusual event that raises concern. Features that alert nurses to the possibility of a bioterrorism-related outbreak include the following (Dire, 2008):
Patient’s Home Environment.
When caring for a patient in the home, a home hazard assessment is necessary. See http://homesafetycouncil.org/safetyguide for a sample home assessment guide. A thorough hazard assessment covers topics such as adequacy of lighting (inside and outdoors), presence of safety devices, placement of furniture or other items that can create barriers, condition of flooring, and safety in the kitchen and bathrooms. Know where medications and cleaning supplies are located. Walk through the home with the patient and discuss how he or she normally conducts daily activities and whether the environment poses problems. Assess for the presence of locks on doors and windows that make the home less susceptible to intruders. When assessing the adequacy of lighting, inspect the areas where the patient moves and works such as outside walkways, steps, interior halls, and doorways. Getting a sense of the patient’s routines helps you recognize less obvious hazards.
Assessment for risk of food infection or poisoning includes assessing a patient’s knowledge of food preparation and storage practices. For example, does a patient know to check expiration dates of prepared food and milk products? Does he or she keep foods in the refrigerator that are fresh and not spoiled? Does the patient clean fresh fruits and vegetables correctly before eating them? Assess for clinical signs of infection by conducting an examination of GI and central nervous system function, observing for a fever, and analyzing the results of cultures of feces and emesis. In the home inspect suspected food and water sources and assess the patient’s handwashing practices. It is useful to ask patients when they routinely wash their hands. This then prompts a helpful discussion about the purpose and importance of handwashing.
Assessment of the environmental comfort of a patient’s home includes a review of when the patient normally has heating and cooling systems serviced. Does the patient have a functional furnace or space heater? Does the home have air conditioning or fans? You need to inform patients who use space heaters of the risk for fires. Are smoke detectors, carbon monoxide detectors, and fire extinguishers present and placed strategically throughout the home and checked routinely?
When patients live in older homes, encourage them to have inspections for the presence of lead in paint, dust, or soil. Because lead also comes from the solder or plumbing fixtures in a home, patients need to have water from each faucet tested. Local health offices will help homeowners locate a trained lead inspector who takes samples from various locations and has them analyzed at a laboratory for lead content.
It is important that your assessment help individuals focus on avoiding losses and reducing their risk for injury associated with disasters. The FEMA (http://www.fema.gov/) and the American Red Cross (http://www.redcross.org/) provide nationwide education to help community members prepare for disasters of all types.
Nursing Diagnosis
Gather data from your nursing assessment and analyze clusters of defining characteristics to identify relevant nursing diagnoses. Include specific related or contributing factors to individualize your nursing care (Box 27-6). For example, the nursing diagnosis risk for injury is sometimes related to altered mobility or sensory alteration (e.g., visual). Altered mobility leads you to select such nursing interventions as range-of-motion (ROM) exercises or teaching the proper use of safety devices such as side rails, canes, or crutches. Visual impairment as the related factor leads you to select different interventions such as keeping the area well lit; orienting the patient to the surrounding; or keeping eye glasses clean, handy, and well protected. When you do not identify the correct related factor, the use of inappropriate interventions increases a patient’s risk for injury. For example, not evaluating the home environment for hazards possibly results in sending a hospitalized patient home only to return with an additional injury. Nursing diagnoses for patients with safety risk include the following:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree