Donna D. Ignatavicius
Pain
The Fifth Vital Sign
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
7 Perform a complete pain assessment, and document per agency policy.
8 Differentiate between addiction, pseudoaddiction, tolerance, and physical dependence.
9 Compare and contrast the characteristics of the major types of pain and examples of each.
10 Explain the role of non-opioid analgesics in pain management.
11 Develop a plan of care to prevent common side effects of opioid analgesics.
12 Compare the advantages and disadvantages of drug administration routes.
13 Determine the patient’s need for pain medication, including PRN and adjuvant therapy.
14 Prioritize care for the patient receiving patient-controlled analgesia.
15 Outline care for a patient receiving epidural analgesia.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
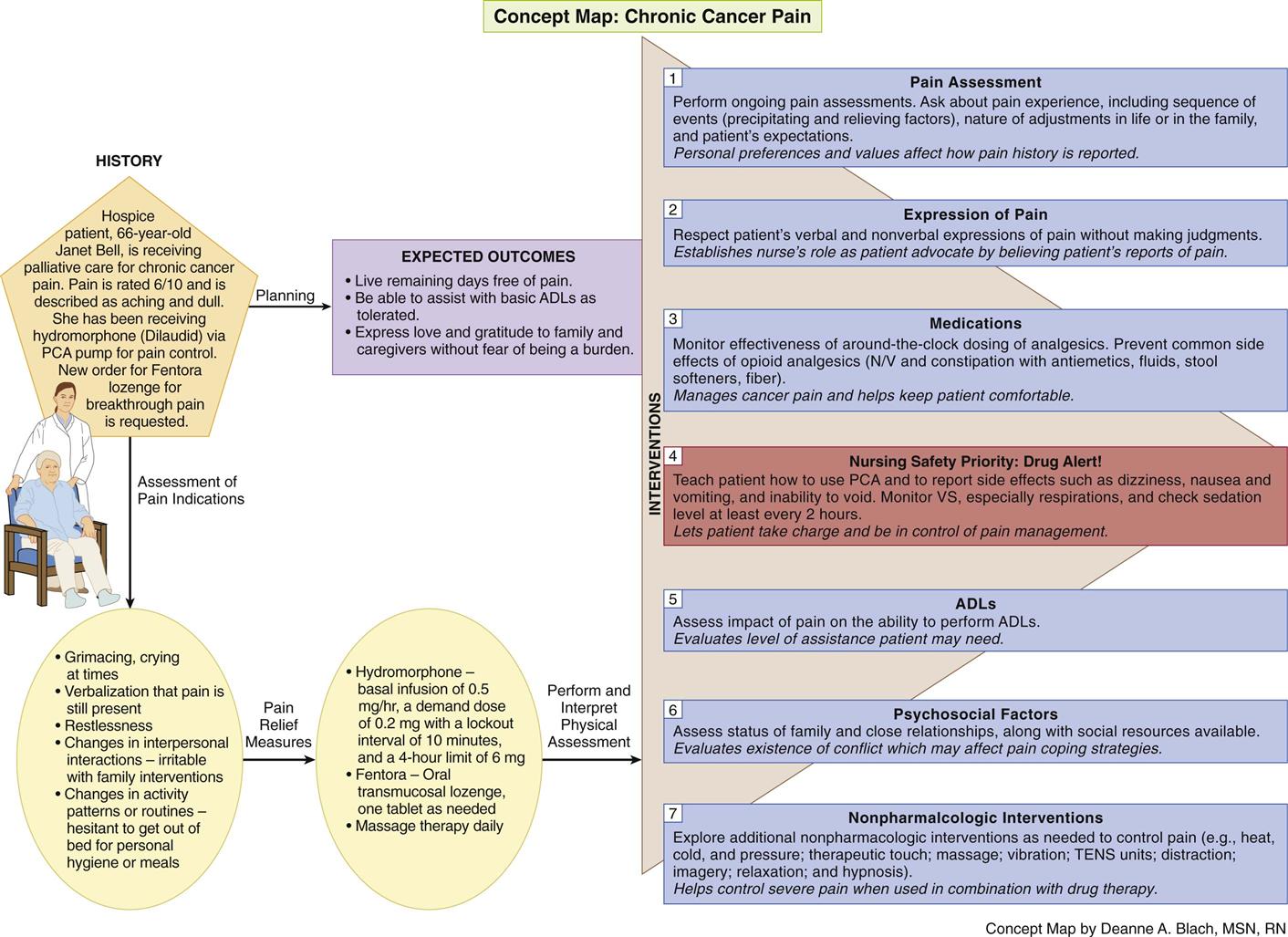
Concept Map: Chronic Cancer Pain
Key Points
Review Questions for the NCLEX® Examination
Pain is a universal, complex, subjective experience. It is the most common reason for a patient to seek medical care and the number-one reason for a person to take medication. It alters or diminishes quality of life more than any other single health-related problem. Despite more than 35 years of work by clinicians and professional and lay organizations, unrelieved and undertreated pain remains a major yet often avoidable public health problem in the world.
The nurse’s primary role in pain management is to advocate for the patient by believing reports of pain and acting promptly to relieve it, while respecting the patient’s preferences and values (Quality and Safety Education for Nurses [QSEN], 2011). Even though some nurses with many years of experience think that they can identify patients in pain, it is sometimes not easy to do.
In response to mandates by The Joint Commission and other organizations, many hospitals and other health care agencies in the United States have interdisciplinary pain teams, also known as analgesia teams, who consult with staff and prescribers on how best to control the patient’s pain. The team typically consists of one or more nurses, pharmacists, case managers, and physicians. In larger facilities, pain teams may specialize by type of pain (e.g., cancer pain team). Although a large part of the team’s plan may center on drug therapy, this group also recommends nonpharmacologic measures as appropriate.
Overview
Everyone experiences pain at some point in life. Because pain is such a private and personal experience, it may be difficult to describe or explain to others. The amount of pain and responses to it vary from person to person; therefore interpreting pain solely on actions or behaviors can be misleading.
Pain is generally related to some type of tissue damage and serves as a warning signal. Although pain is familiar to most people, it is so complex that there is no single, universal treatment.
Definitions of Pain
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage. In their classic work, McCaffery and Pasero (1999) offered a more personal explanation of pain when they stated that pain is whatever the experiencing person says it is and exists whenever he or she says it does. This understanding of pain requires that the patient be seen as the authority on the pain and as the only one who can define the experience. In other words, self-report is always the most reliable indication of pain. Nurses who approach pain from this perspective can help the patient achieve effective pain management by advocating for proper control. Of course, if the patient cannot communicate, self-report is not possible. In this case, a variety of methods and observation of nonverbal indicators are used to assess the pain, as described later in this chapter.
Scope of the Problem
Pain is also a major economic problem and a leading cause of disability that hampers the lives of many people, especially older adults. Chronic pain is the most common cause of long-term disability, affecting millions of Americans and others throughout the world.
Pain is not adequately treated in all areas of health care. Populations at the highest risk are older adults, substance abusers, and those whose primary language differs from that of the health care professional. Older adults in nursing homes are especially at risk because of lack of professional staff and communication problems. In patients who are substance abusers, unrelieved pain can contribute to relapses or increased substance use.
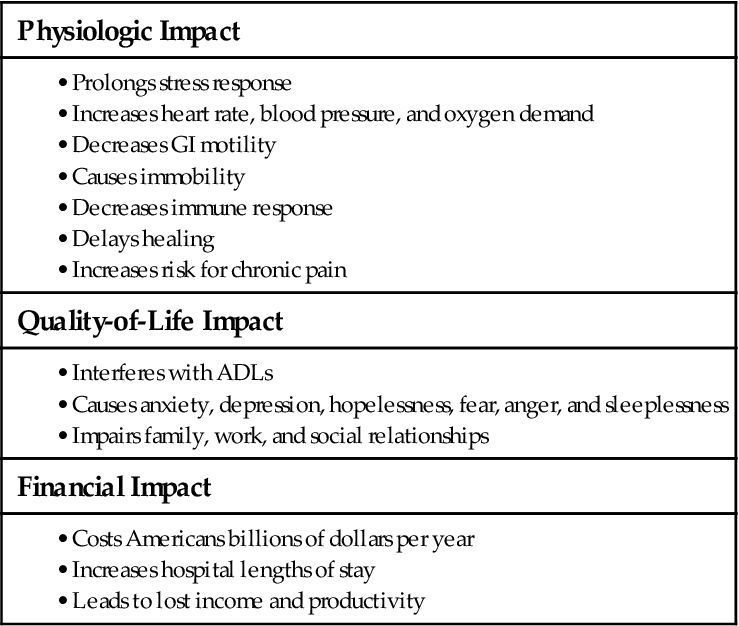
Inadequate pain management can lead to many consequences affecting the patient and family members. These consequences often affect the patient’s and family’s quality of life (Table 5-1). Therefore, as a nurse, you have a legal and ethical responsibility to ensure that patients receive adequate pain control. In 2000, The Joint Commission (TJC) published pain standards approved by the American Pain Society. TJC states that patients in all health care settings, including home care, have a right to effective pain management.
Patients rely on nurses and other health care professionals to adequately assess and manage their pain. As the coordinator of patient care, be sure to accurately document your assessments and actions, including patient and caregiver teaching.
Categorizing Pain
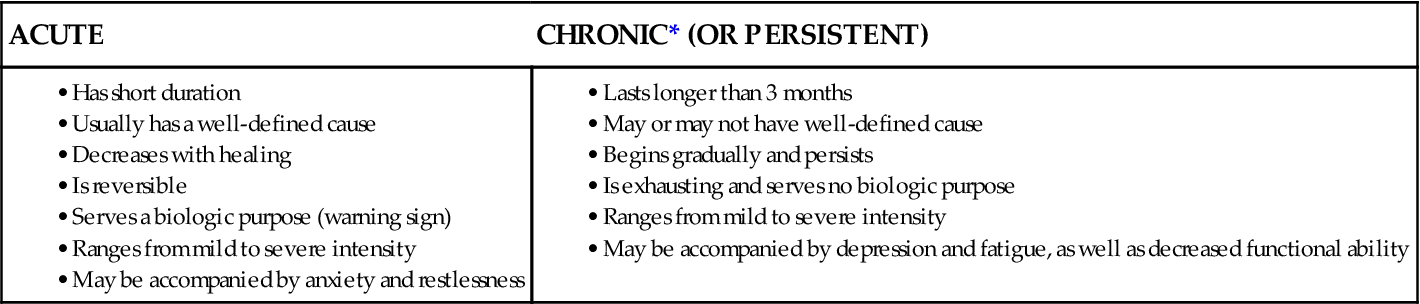
Pain can be categorized in two ways: by type related to the characteristics of the pain (Table 5-2) or by the physiologic source of the pain. The two major types of pain are acute and chronic. Acute pain often results from sudden, accidental trauma (e.g., fractures, burns, lacerations) or from surgery, ischemia, or acute inflammation. Chronic pain or persistent pain is further divided into two subtypes. Chronic cancer pain is pain associated with cancer or another progressive disease such as acquired immune deficiency syndrome (AIDS). The cause of pain is usually life threatening. Chronic non-cancer pain is associated with tissue injury that has healed or is not associated with cancer, such as arthritis or chronic back pain. This type of pain is the most common.
Acute Pain
Almost everyone experiences acute pain at some time. The major distinction between acute pain and chronic pain is the effect on biologic responses. Acute pain serves a biologic purpose. It acts as a warning signal by activating the sympathetic nervous system and causing various physiologic responses. These responses are similar to those found in “fight-or-flight” reactions and include:
Behavioral signs of acute pain may include restlessness (especially among older adults), an inability to concentrate, apprehension, and overall distress.
Acute pain is usually temporary, has a sudden onset, and is easily localized. The pain is typically confined to the injured area and may subside with or without treatment. As the injured area heals, the pain sensation changes. Although possibly severe, acute pain is limited over time and generally can be managed successfully. Both the caregiver and the patient can see an end to the pain, which makes coping somewhat easier.
Pain that accompanies surgery is one of the most common examples of acute pain, but it is not always well managed. Usually, poorly managed postoperative pain is a result of inadequate drug therapy.
The severity of postoperative pain may be a predictor of long-term pain. The use of preemptive analgesia is a technique designed to decrease pain in the postoperative period, decrease the requirements for a postoperative analgesic, prevent morbidity, and decrease hospital stay. Preemptive analgesia includes administering local anesthetics, opioids, and other drugs in the preoperative, intraoperative, and/or postoperative period. This intervention may inhibit changes in the spinal cord—changes that can lead to a central sensitization that results in chronic pain.
In general, intrathoracic and upper intra-abdominal surgical approaches are associated with more severe, steady wound pain and with pain on movement after surgery. Many patients who undergo superficial surgery of the head and neck, chest wall, or limbs report minimal postoperative pain. Muscle-splitting procedures, like thoracotomy, are generally far more painful than muscle-stretching procedures, such as open hysterectomy. Patients who have joint replacements for severe arthritic pain often report less pain after surgery than before surgery because the damaged joint cartilage has been removed.
Chronic Pain
Chronic pain or persistent pain is often defined as pain that lasts or recurs for indefinite periods, usually for more than 3 months. The onset is gradual, and the character and quality of the pain change over time. Because chronic pain often involves deep body structures, it is usually poorly localized (hard to pinpoint) and often difficult to describe. If the underlying cause cannot be treated, controlling the long-term effects of chronic pain may be a difficult clinical challenge.
Because chronic pain persists for extended periods, it can interfere with personal relationships and ADLs. It can also result in emotional and financial burdens. Some patients feel depressed and hopeless because of uncontrolled chronic pain and its consequences. Although many characteristics of chronic pain are similar in different patients, be aware that each patient is unique and requires a highly specialized plan of care.
Chronic Cancer Pain.
Most patients with advanced cancer have moderate to severe pain. What is frustrating is that we have known for over 30 years that 90% of cancer pain can be successfully managed by giving adequate amounts of oral opioids around the clock. Yet patients with terminal cancer are often inadequately treated for their excruciating pain.
Most cancer pain is caused by the disease itself. The sources of pain include nerve compression, invasion of tissue, and/or bone metastasis, an extremely painful condition. Cancer treatments also can cause pain (e.g., from surgery and toxicities from chemotherapy and radiation therapy).
Patients with cancer pain generally have pain in two or more areas but usually talk about only the primary area of pain. Be sure to perform a complete pain assessment to ensure an effective plan of care (see the Concept Map on p. 42).
Chronic Non-Cancer Pain.
Chronic non-cancer pain is an even larger global health problem, occurring most often in people older than 65 years. Unlike acute pain, chronic pain serves no biologic purpose. After the initial warning signal of pain, the body must learn to adapt to the persistent pain impulses by blocking or adjusting to sympathetic nervous system response (which causes the fight-or-flight reaction in acute pain). Because of this adaptation, the symptoms often associated with acute pain, such as increased pulse, are absent with chronic pain.
Chronic non-cancer pain was formerly called chronic nonmalignant pain. However, most pain experts, and certainly patients who suffer with daily pain, believe that all pain is malignant—thus the newer term. Chronic non-cancer pain may be caused by chronic diseases such as rheumatoid arthritis, back injuries, and fibromyalgia.
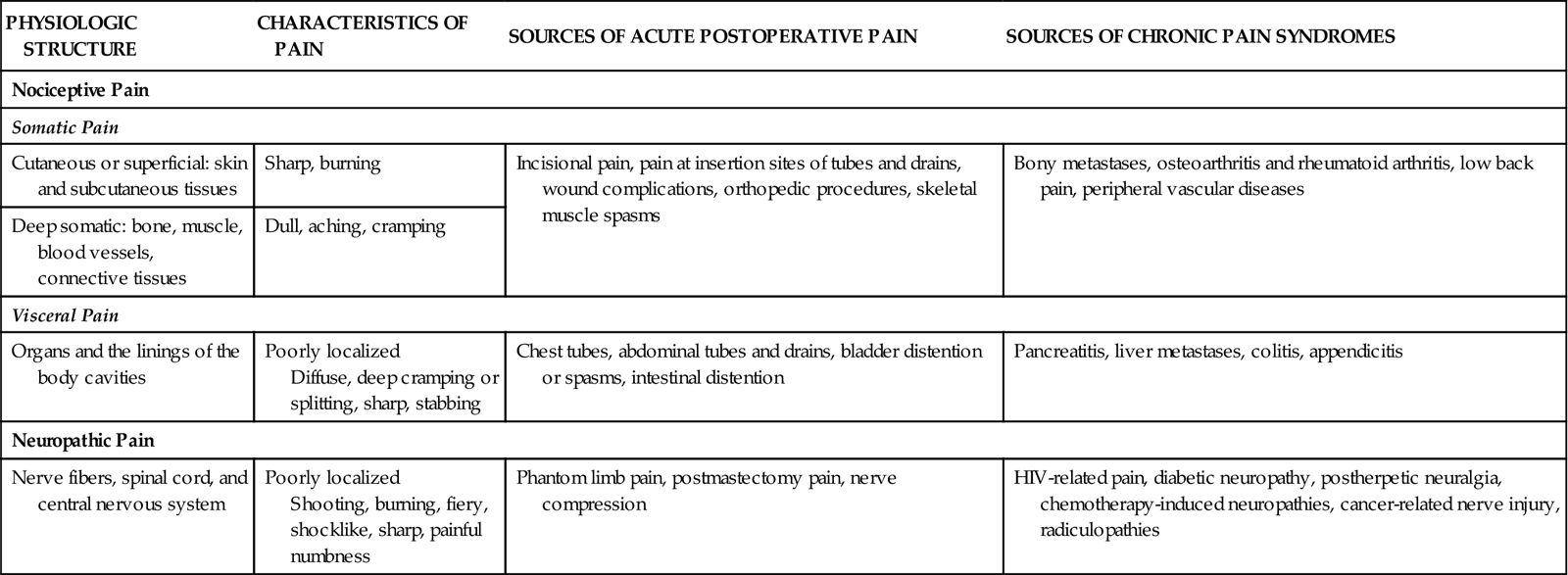
Pain is also categorized as either nociceptive (normal processing of pain) or neuropathic (abnormal pain processing). Nociceptive pain is either visceral or somatic (Table 5-3). Somatic pain arises from the skin and musculoskeletal structures, and visceral pain arises from organs. Neuropathic pain is one of the most challenging types of chronic non-cancer pains; it results from some type of nerve injury. Neuropathic pain is still not completely understood. It is divided into centrally or peripherally generated pain. Regardless of the cause, neuropathic pain is described as burning (most common), shooting, stabbing, and feeling “pins and needles.”
TABLE 5-3
| PHYSIOLOGIC STRUCTURE | CHARACTERISTICS OF PAIN | SOURCES OF ACUTE POSTOPERATIVE PAIN | SOURCES OF CHRONIC PAIN SYNDROMES |
| Nociceptive Pain | |||
| Somatic Pain | |||
| Cutaneous or superficial: skin and subcutaneous tissues | Sharp, burning | Incisional pain, pain at insertion sites of tubes and drains, wound complications, orthopedic procedures, skeletal muscle spasms | Bony metastases, osteoarthritis and rheumatoid arthritis, low back pain, peripheral vascular diseases |
| Deep somatic: bone, muscle, blood vessels, connective tissues | Dull, aching, cramping | ||
| Visceral Pain | |||
| Organs and the linings of the body cavities | Poorly localized Diffuse, deep cramping or splitting, sharp, stabbing | Chest tubes, abdominal tubes and drains, bladder distention or spasms, intestinal distention | Pancreatitis, liver metastases, colitis, appendicitis |
| Neuropathic Pain | |||
| Nerve fibers, spinal cord, and central nervous system | Poorly localized Shooting, burning, fiery, shocklike, sharp, painful numbness | Phantom limb pain, postmastectomy pain, nerve compression | HIV-related pain, diabetic neuropathy, postherpetic neuralgia, chemotherapy-induced neuropathies, cancer-related nerve injury, radiculopathies |
Theoretical Bases for Pain
Pain Transmission
Painful stimuli often originate in the periphery (extremities) of the body. To be perceived, the stimuli must be transmitted first to the spinal cord and then to the central areas of the brain. If the pain impulse is not transmitted to the brain, the person feels no pain. In the periphery, two specific fibers can transmit stimuli: (1) A delta fibers, which are found primarily in the skin and muscle; and (2) C fibers, which are distributed in muscle, periosteum, and viscera. Both of these nerve fibers are capable of accepting nociceptive stimuli.
A delta fibers are myelinated fibers that carry rapid, sharp, pricking, or piercing sensations. A person feeling these sensations can generally localize them readily to a fairly well-defined area. Because these fibers respond mainly to mechanical rather than chemical or thermal stimuli, they are called mechanical nociceptors.
C fibers are unmyelinated or poorly myelinated fibers that conduct thermal, chemical, and strong mechanical impulses. Pain conduction from C fibers is slow, more diffuse (widespread) and dull, burning, or achy—quite different from the sensations of A delta fibers. In contrast to the intermittent nature of A delta sensations, C fibers usually produce persistent pain.
Although many theories of pain have been discussed, the classic gate control theory by Melzack and Wall (1982) still forms the basis of what is believed by most pain researchers today. According to this theory, a gating mechanism occurs in the spinal cord. Nerve fibers (A delta and C fibers) transmit pain impulses from the periphery of the body. These impulses travel to the dorsal horn of the spinal cord, specifically to the substantia gelatinosa, where the gating mechanism occurs. When the gate is opened, pain impulses ascend to the brain; when the gate is closed, the impulses do not get through and pain is not perceived (Fig. 5-1).
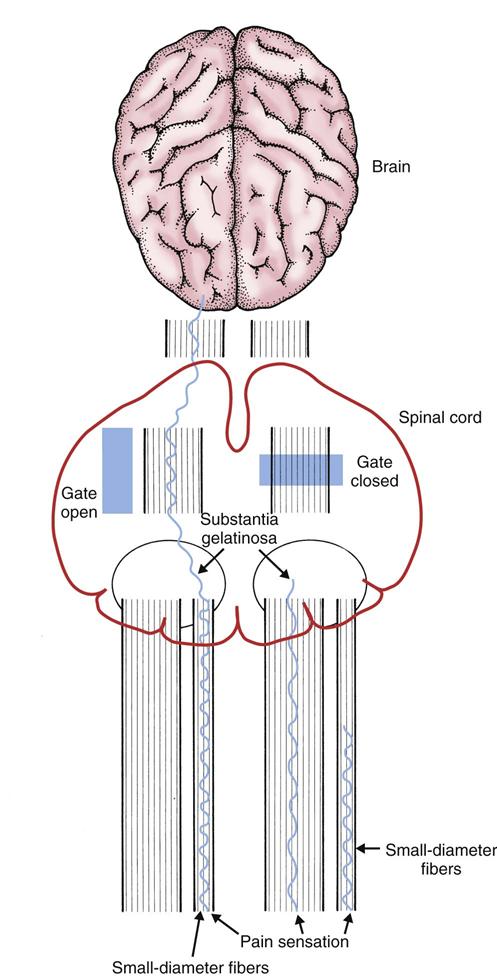
Morphine-like substances called endorphins are released when the large-diameter nerve fibers are stimulated. These fibers close the gate and decrease pain transmission. This helps explain why many noninvasive pain management techniques work to relieve pain. Endorphins are thought to be a gene product, and producing them requires a stimulus to the brain.
Similar gating mechanisms exist in the nerve fibers descending from the thalamus and cerebral cortex. These areas of the brain regulate thoughts and emotions, including beliefs and values. When pain occurs, a person’s thoughts and emotions can modify one’s perceptions as they reach the level of conscious awareness.
The gate control theory has helped nurses and other health care professionals recognize the holistic nature of pain. As a result, many cognitive-behavioral therapies (e.g., imagery and distraction described on p. 60) are used to help relieve pain.
Attitudes and Practices Related to Pain
The attitudes of health care professionals toward pain influence the way they perceive and interact with patients in pain. Without adequate assessment skills or knowledge of pain and analgesic therapy, they may not be able to understand their patients’ pain.
Nurses who have little personal experience with pain may not appreciate the scope of painful conditions associated with diseases and medical or surgical interventions. They may expect patients with chronic pain to react similarly to those with acute pain. Nurses may assume that reactions to pain fall within a certain norm based on their own cultural values. The more that a patient’s response varies from these expected norms, the more likely that a nurse’s attitude toward the patient will be positively or negatively biased.
Not only do health care professionals need continued education about pain management, but the public needs education as well. Nurses can help patients and their families achieve and maintain successful pain management through education.
Many patients are reluctant to report pain. When they do, they may underreport its severity. Patients may not share their existence of pain because they want to be “good” patients or do not want to bother or distract their caregivers from other issues in their care. In patients with a history of cancer, pain can be an unwanted reminder of the disease and its progression.
Some patients are also reluctant to take pain medications, especially opioid analgesics, because they fear becoming addicted to or used to the drug, especially older adults. Educate patients and reassure them that these drugs are not likely to cause addiction in those having pain.
Pain Perception
Many variables affect the perception of and response to pain. Factors such as age, gender, sociocultural background, and genetics influence the patient’s ability to process and react to pain. These factors also put patients at risk for undertreatment.
Certain painful conditions are more common in either men or women. Most chronic pain sufferers are women. Women have more migraine headaches, tension headaches, rheumatoid arthritis and osteoarthritis, fibromyalgia, and multiple sclerosis. Men have more cluster headaches, back pain, gout, peripheral vascular disease, and postherpetic neuralgia.
Addiction, Pseudoaddiction, Tolerance, and Physical Dependence
It is crucial that nurses and other health care professionals not label a patient as an “addict,” “clock-watcher,” or “drug seeker.” These labels have caused biases and have a negative impact on the patient-nurse relationship.
In their classic position statement, the American Society for Pain Management Nursing (ASPMN) states that addiction is (ASPMN, 2002):
… a primary, chronic neurobiologic disease with genetic, psychosocial, and environmental factors influencing its development and manifestations. It is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving. (p. 1)
Addiction occurs over a long time—not as a result of one hospital stay or treatment for one episode of acute pain.
The danger of addiction to pain medication is vastly overrated. Although available data on addiction consistently show that it is rarely a result of using opioids for pain relief, health care professionals still have exaggerated fears. Patients and families also have fears related to addiction. Carefully explain the difference between physical dependence and addiction whenever a patient starts on opioid therapy.
Pseudoaddiction is (ASPMN, 2002):
… an iatrogenic syndrome created by the undertreatment of pain. It is characterized by patient behaviors such as anger and escalating demands for more or different medications, and results in suspicion and avoidance by staff. (p. 1)
Pseudoaddiction can be distinguished from true addiction in that the behaviors resolve when pain is effectively treated.
Tolerance is (ASPMN, 2002):
… a state of adaptation in which exposure to a drug induces changes that result in a decrease in one or more of the drug’s effects over time. (p. 1)
Some of these changes include increasing drug excretion and reducing the number of receptors to bind the drug. Many advanced cancer patients find that they need increasing doses of opioids to control their pain.
Physical dependence is the (ASPMN, 2002):
… adaptation manifested by a drug-class–specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug, and/or administration of an antagonist. (p. 1)
A person who is drug tolerant, however, does not experience withdrawal, even when the drug is stopped suddenly.
Physical dependence occurs in everyone who takes opioids over a period of time. It is important to prevent physical withdrawal. So-called withdrawal or abstinence syndrome results when a patient who is physically dependent on opioids abruptly ceases using them. Abstinence syndrome may also occur if a patient on opioids receives a reversal agent, such as naloxone (Narcan). These symptoms result from autonomic nervous system responses and include nausea and vomiting, abdominal cramping, muscle twitching, profuse perspiration, delirium, and convulsions. When necessary to discontinue opioid analgesia for a patient who is opioid dependent, a slow tapering (weaning) of the drug dosage lessens or alleviates the physical withdrawal symptoms. Doses of opioids should be tapered by 10% to 20% daily for patients on chronic opioid therapy. Clonidine (Catapres, Dixarit ![]() ) may be used to help alleviate the distressing symptoms of withdrawal in younger adults. It should not be given to older adults because of its side effects.
) may be used to help alleviate the distressing symptoms of withdrawal in younger adults. It should not be given to older adults because of its side effects.
Although tolerance, physical dependence, and addiction are different conditions, they may coexist. However, it is important to distinguish tolerance and physical dependence from addiction.
Patients who are substance abusers often have traumatic injuries and other health problems that cause pain. Keep in mind that substance abusers, typically those abusing opioids, are often tolerant to the pain-relieving effects of opioid analgesics and generally require increased doses. Abrupt physiologic withdrawal is always a danger when recreational users of opioid agonists are given mixed agonist-antagonists and partial agonists.
The clinical use of placebos in non–research-based therapies has not been shown to have a sustained effect on pain relief. A placebo is any medical treatment or nursing care that produces an effect in a patient because of its therapeutic intent and not because of its actual physical or chemical properties. When a patient responds favorably to a placebo, it is known as the placebo effect. Placebos do not indicate whether or not a patient has real pain.
As required by most health care accrediting or regulatory agencies, health care agencies have developed programs to educate professionals about pain management, including the inappropriate use of placebos. Because of The Joint Commission’s commitment to effective pain control, a policy against the use of placebos is recommended to be in place in all accredited institutions and agencies. The American Society for Pain Management Nursing (ASPMN) has a position statement available on the website against the use of placebos for the management of pain (ASPMN, 2010).
Patient-Centered Collaborative Care
Assessment
History
The American Pain Society refers to pain as the fifth vital sign. Like for vital signs, health care agencies require initial and ongoing pain assessments. Begin by asking the patient about the:
• Pain experience, including the sequence of events (precipitating and relieving factors)
• Nature of adjustments, if any, in life or in the family
• Beliefs about the cause of the pain and what should be done about it (patient’s expectations)
Remember that the patient’s personal preferences and values affect how he or she reports the pain history. When culturally appropriate, be sure to include families and significant others in this information-gathering process to be family-centered.
Patients may report pain in the absence of any observable or documented physiologic changes. To be patient-centered, respect the patient’s verbal and nonverbal expressions of pain without making judgments or inferences about the reality of the pain. If patients perceive that health care professionals doubt the existence of their pain, mistrust and other negative feelings can arise and interfere with a therapeutic nurse-patient relationship.
Assess the length of time the patient has experienced pain. Patients may welcome an opportunity to discuss acute pain with the nurse because it is a relatively short-term experience and is easily described. However, those with chronic pain can become frustrated when they are unable to adequately describe their often vague and diffuse pain experience. Structured interviews using assessment aids (e.g., pain scales, descriptors) often help patients express their pain.
Information about a person’s pain can be helpful in understanding the factors associated with the present pain or previous episodes of pain. If the patient is in pain when you are obtaining the history, keep the session reasonably short or continue later. Essential data include:
Physical Assessment/Clinical Manifestations
People with acute pain may have physiologic changes, such as tachycardia and blood pressure changes. Blood pressure is usually increased initially and then decreased. However, not all patients with acute pain have these signs, so his or her statement of pain is the only reliable indicator.
A person with chronic pain usually adapts to these physiologic changes as the body attempts to compensate for and adapt to noxious stimuli. The pain no longer serves as a necessary warning. Patients with chronic pain, then, often develop coping skills and may appear to look quite well.
Certain motor or body movements may be associated with either acute or chronic pain. Some may be more exaggerated or obvious than others. Patients in pain may support or shield (“splint”), holding painful body parts while moving, or they may lie listlessly because they are afraid to move. Assess the functional status and degree of impairment in the patient with pain.
The mnemonic PQRST may be helpful in organizing the pain assessment (Jarvis, 2012):
Q: Quality or quantity. How does it look, feel, or sound? How intense/severe is it?
R: Region or radiation. Where is it? Does it spread anywhere?
Location of Pain.
Assess the level and location of pain. If oriented, most patients can usually describe the severity of acute pain or chronic pain. The actual area or location of the pain, however, may not be as easily identified. Ask the patient whether the pain is superficial or deep. In general, those with pain involving superficial or cutaneous (skin) structures describe their pain as superficial and can often localize the pain to a specific area.
Pain may be described as belonging to one of four categories related to its location:
• Localized pain is pain confined to the site of origin.
• Projected pain is pain along a specific nerve or nerves.
• Radiating pain is diffuse pain around the site of origin that is not well localized.
• Referred pain is pain perceived in an area distant from the site of painful stimuli.
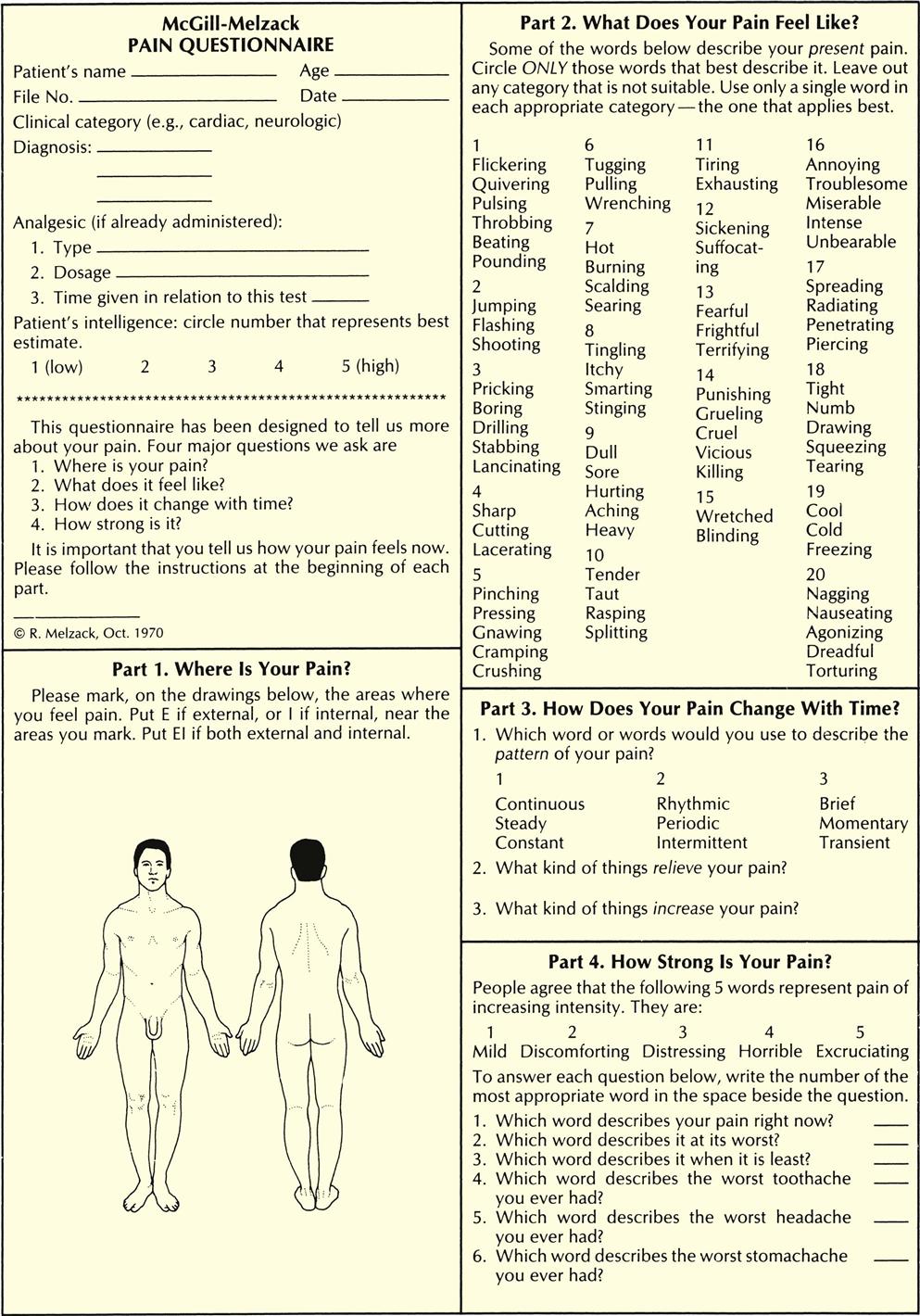
Ask the patient who has difficulty specifying the exact location of pain to point to the painful areas on his or her own body or on another person. If the patient is able to communicate, have him or her point to or shade in the painful areas on a diagram of the front and back of the human body (Fig. 5-2). Encourage those who cannot identify the painful areas and state that they just “hurt all over” to focus on parts of the body that are not painful. Ask the patient to concentrate on different body parts, beginning with the hand and fingers of one extremity, and identify the presence or absence of pain. By focusing attention on selected areas of the body, the patient is assisted in localizing painful areas. People who state that they hurt everywhere often begin to realize that some parts of the body are not painful.
Patients may present with more than one specific painful site. Identifying painful areas helps the patient understand the origin of the pain. This understanding is particularly important for those with cancer, because every new pain often raises the suspicion of metastasis (spread of disease). The pain may have other causes, such as immobility or constipation.
Intensity and Quality of Pain.
After asking the patient to locate the pain, ask him or her to describe it. He or she may use one word or a group of words to convey the sensations or feelings of the pain. Avoid suggesting descriptive words for the pain.
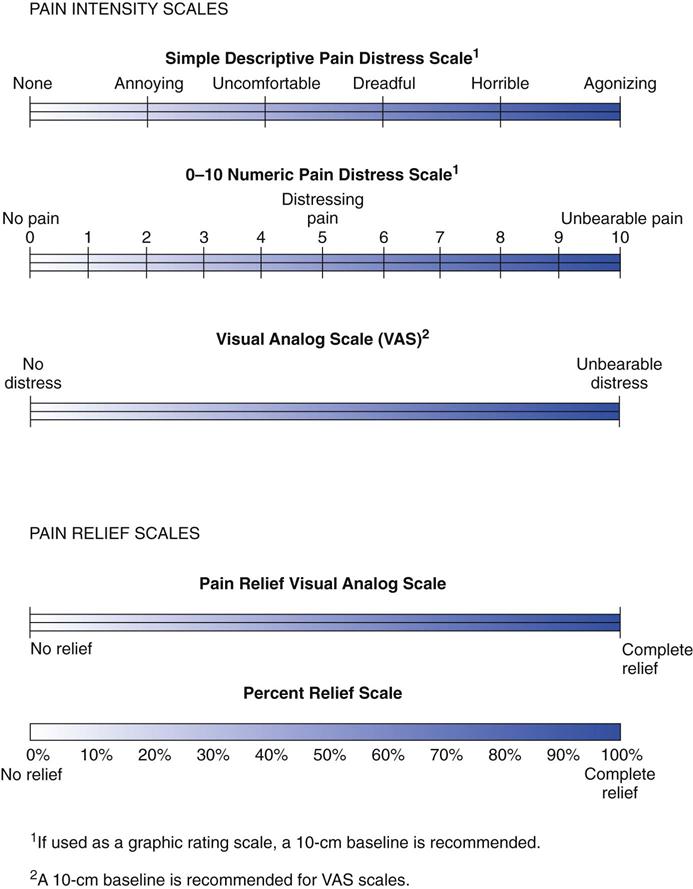
Subjective measurements of pain intensity are more reliable and accurate than observable qualities of pain. Only the patient can determine the amount or severity of pain being experienced. Various visual analog scales (VASs), number rating scales (NRSs), descriptive word scales, and other measures have been designed to help patients communicate the magnitude or severity of pain and to help nurses quantify the pain (Fig. 5-3).
Use pain intensity scales to measure pain in the clinical or home setting and to assess and determine the effectiveness of pain relief interventions. For most pain scales, the patient is asked to rate the amount of painful stimuli. Patients with more than one discrete painful site may wish to specify their pain levels by location. Some scales also assess the emotional aspect of pain. Be sure to use the same scale over time for the patient, and assess pain intensity both with and without activity.
Verbal descriptive scales typically group words such as “none,” “moderate,” or “severe” and permit an intensity rating of pain. However, the 0-to-10 or 1-to-10 NRS is used most commonly in clinical practice for adult patients who can communicate in English (see Fig. 5-3). For culturally diverse patients with language barriers, the Wong-Baker FACES Pain Rating Scale (pain rating scale of smile to frown) may be helpful. This scale is also used for children, older adults, and developmentally disabled populations (Flaherty, 2008).
Assessing Pain in Cognitively Impaired or Critically Ill Nonverbal Patients.
Although it seems obvious, nonverbal, intubated, and cognitively impaired patients do feel pain! It is important to be proactive and assume pain is present, or “APP.”
In 2006, the American Society for Pain Management Nursing published its classic position statement on evidence-based recommendations when performing pain assessments for nonverbal patients (Herr et al., 2006). Five general recommendations for pain assessment were presented:
• Use self-report (when possible).
• Search for potential causes of pain.
• Recognize the value of surrogate reporting (e.g., family member or life partner).
Nurses and other clinicians have recently been researching assessment tools to measure observable nonverbal behaviors that indicate the patient is in pain. A variety of valid and reliable tools are published in the literature (Federico, 2009). Most of them are designed to be used for patients with severe dementia. Examples of commonly used assessment tools that can be used for patients with acute confusion or dementia include:
• Pain Assessment Tool for Confused Older Adults (used for hospitalized patients)
• Pain Assessment in Advanced Dementia Scale (PAINAD)
• Discomfort in Dementia of the Alzheimer’s Type Scale
• Faces, Legs, Activity, Crying and Consolability Tool
• Non-Communicative Patient’s Pain Assessment Instrument (NOPPAIN)
The Checklist of Nonverbal Pain Indicators is based on the work of The American Geriatrics Society (AGS) Panel on Persistent Pain in Older Persons. The panel found six common pain indicators that you can observe and document to indicate pain (AGS, 2002):
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree