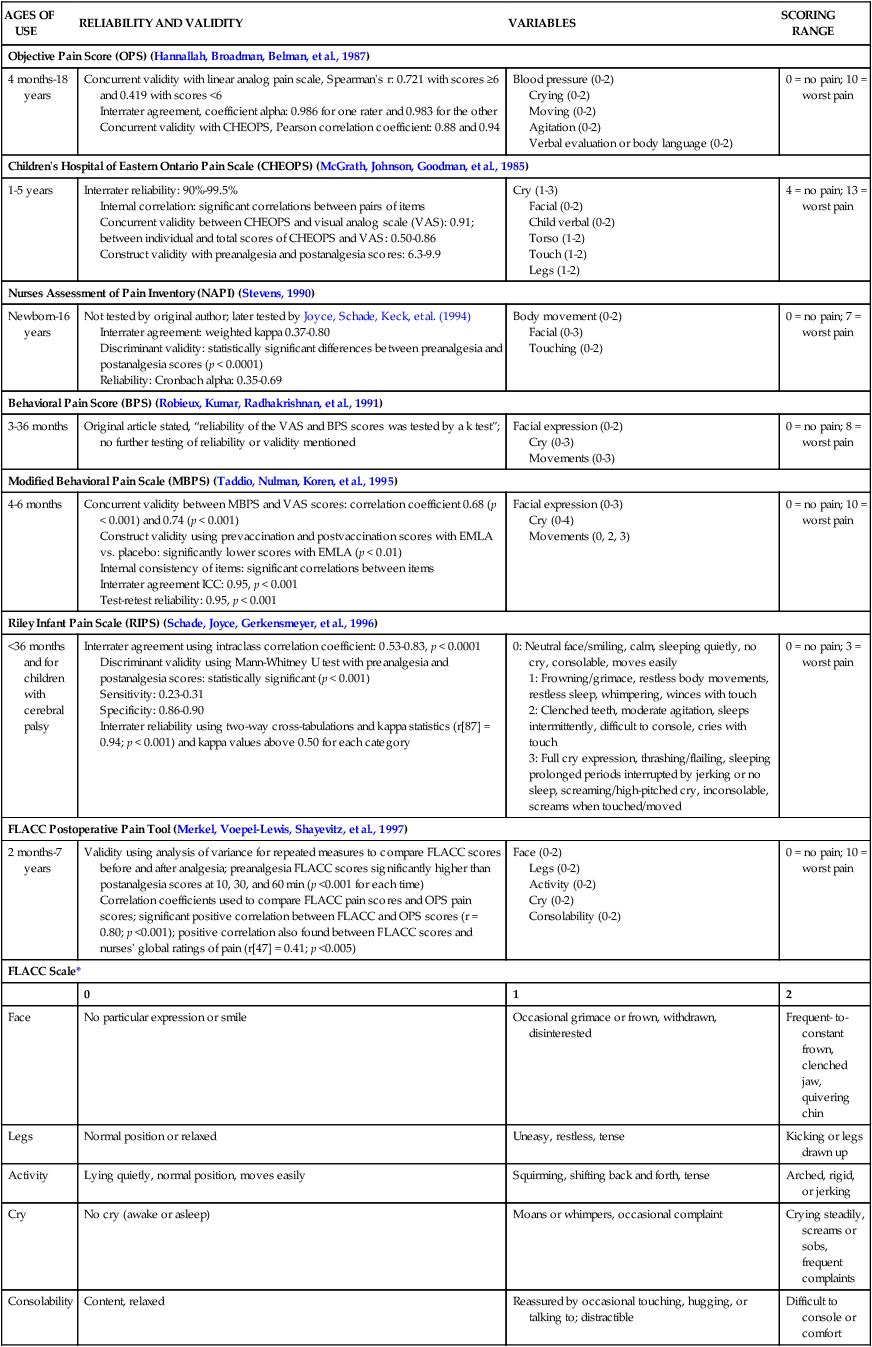
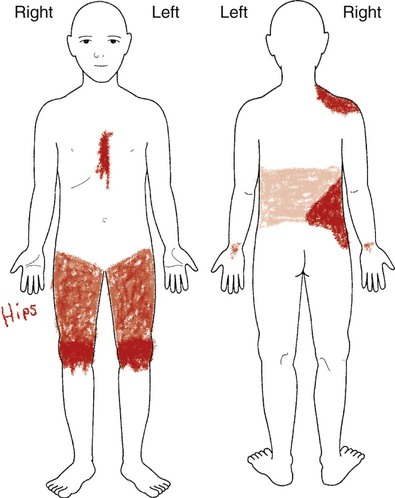
Chapter 30 On completion of this chapter, the reader will be able to: • Identify measures to assess pain in children. • List various types of pain-assessment tools for use with children. • Outline essential pain-management strategies to reduce pain in children. • Review common types of pain experienced by children. • Discuss evidence to support specific pain-management strategies. Many children and adolescents continue to suffer from inadequately treated pain of all types (Perquin, Hazebroek-Kampschreur, Hunfeld, et al., 2000). Several research studies suggest that the undertreatment of pain in children is related to inconsistent practice in pain assessment, administration of analgesics at subtherapeutic levels, prolonged intervals between medications (Jacob and Puntillo, 2000), and lack of systematic monitoring and evaluation of relief (Jacob, Miaskowski, Savedra, et al., 2003a, 2003b; Jacob and Mueller, 2008). Optimal pain management begins with thorough assessment, which guides the selection of treatments. Acute pain assessment is easier to perform than complex pain that may be chronic, recurrent, or persistent. Traditionally assessment measures are defined as behavioral measures, physiologic measures, and measures of self-reports. These measures predominantly address the domain of pain intensity. The behavioral measures of pain (for infants and children younger than 4 years; Table 30-1) and self-reports of pain (for children 4 years and older; Table 30-2) have been developed, validated, and widely used. Self-report measures are not sufficiently valid for children below 3 years of age because many are not able to accurately self-report their pain. Distress behaviors such as vocalization, facial expression, and body movement have been associated with pain (Figs. 30-1 and 30-2; Box 30-1). These behaviors are helpful in evaluating pain in infants and children with limited communication skills. However, discriminating between pain behaviors and reactions from other sources of distress such as hunger, anxiety, or other types of discomfort is not always easy. These factors decrease the specificity and sensitivity of behavioral measures (see Table 30-1). TABLE 30-1 SUMMARY OF SELECTED BEHAVIORAL PAIN ASSESSMENT SCALES FOR YOUNG CHILDREN *From Merkel SI, Voepel-Lewis T, Shayevitz JR, et al: The FLACC: a behavioral scale for scoring postoperative pain in young children, Pediatr Nurs 23(3):293–297, 1997. Used with permission of Jannetti Publications, Inc., and the University of Michigan Health System. Can be reproduced for clinical and research use. TABLE 30-2 PAIN-RATING SCALES FOR CHILDREN *Wong-Baker FACES Pain Rating Scale reference manual describing development and research of the scale is available from City of Hope Pain/Palliative Care Resource Center, 1500 East Duarte Road, Duarte, CA 91010; (626) 359-8111, ext. 3829; fax (626) 301-8941; www.elsevierhealth.com/WOW/. Use of FACES with children is demonstrated in Whaley and Wong’s Pediatric Nursing Video Series, “Pain Assessment and Management,” narrated by Donna Wong, PhD, RN. Available from Elsevier, 3251 Riverport Lane, Maryland Heights, MO, 63043; (800) 426-4545; fax (800) 535-9935; www.elsevierhealth.com. †Instructions for Word-Graphic Rating Scale from Acute Pain Management Guideline Panel: Acute pain management in infants, children, and adolescents: operative and medical procedures; quick reference guide for clinicians, ACHPR Pub No 92-0020, Rockville, MD, 1992, Agency for Health Care Research and Quality, US Department of Health and Human Services. Word-Graphic Rating Scale is part of the Adolescent Pediatric Pain Tool and is available from Pediatric Pain Study, University of California, School of Nursing, Department of Family Health Care Nursing, San Francisco, CA 94143-0606; (415) 476-4040. The most commonly used behavioral pain measure is the FLACC. The FLACC Pain Assessment Tool (Manworren and Hynan, 2003; Merkel, Voepel-Lewis, Shayevitz, et al., 1997) is an interval scale that includes five categories of behavior: facial expression (F), leg movement (L), activity (A), cry (C), and consolability (C). It measures pain by quantifying pain behaviors with scores ranging from 0 (no pain behaviors) to 10 (most possible pain behaviors). Other behavioral measures (see Table 30-1) include the (1) Children’s Hospital of Eastern Ontario Pain Scale (CHEOPS), which was developed in collaboration with experienced recovery room nurses who were queried about which behaviors they most frequently observed to determine whether a child is in pain (McGrath, Johnson, Goodman, et al., 1985; Suraseranivongse, Montapaneewat T, Manon J, 2005); (2) Toddler-Preschooler Postoperative Pain Scale (TPPPS), which is an observational scale developed for measuring postoperative pain in children ages 1 to 5 years (Suraseranivongse, Montapaneewat T, Manon J, 2005; Tarbell, Cohen, and Marsh, 1992); (3) the Parent’s Postoperative Pain Rating Scale (PPPRS), which is a scale that parents may use to rate their children’s pain by noting changes in the frequency of a number of behaviors (Chambers, 2003; Chambers, Finley, McGrath, et al., 2003; Chambers and Craig, 1998; Finley, Chambers, and McGrath, et al., 2003); and (4) Parents’ Postoperative Pain Measure (PPPM), which was developed based on cues parents reported observing in their children following surgery (e.g., changes in appetite, activity level). In critical care settings the COMFORT scale (Ambuel, Hamlett, Marx, 1992) is recommended. The COMFORT scale is a behavioral, unobtrusive method of measuring distress in unconscious and ventilated patients. It has eight indicators: alertness, calmness/agitation, respiratory response, physical movement, blood pressure, heart rate, muscle tone, and facial tension. Each indicator is scored between 1 and 5 based on the behaviors exhibited by the patient. Patients are observed unobtrusively for 2 minutes, and the total score is derived by adding the scores of each indicator. The total scores can range between 8 and 40. A score of 17 to 26 generally indicates adequate sedation and pain control. Because of the complexity of measuring blood pressure and heart rate, this scale is used primarily for patients in a critical care setting. For children 3 to 4 years the most frequently used measure of pain intensity is the Faces Pain Scale. There are many different “faces” scales. Faces scales provide a series of facial expressions depicting gradations of pain. They are appealing to children and easy to use because children can simply point to the face that represents how they feel. Two faces scales, the Bieri Faces Pain Scale—Revised (Hicks, von Baeyer CL, Spafford PA, et al., 2001) and the Wong-Baker FACES Pain Scale (Wong and Baker, 1988), are the most widely used. The Bieri scale is made up of six faces depicting increasing gradation of pain severity from 0 = “no pain” on the left face to 5 = “most pain possible” on the right face. In developing this scale the authors did not include a smiling face at the “no pain” end or tears at the “most pain” end and validated it so it is equivalent to a 0-to-10 metric system. The Wong-Baker FACES Pain Scale consists of six cartoon faces ranging from a smiling face for “no pain” to a tearful face for “worst pain.” The child is asked to choose a face that describes his or her pain. For children 8 years and older the numeric rating scale (NRS), specifically the 0-to-10 scale, is most widely used in clinical practice because it is easy to use and document. However, there is little research to support the reliability and validity of the NRS, except in the context of the Oucher Pain Scale (Beyer, Turner, Jones, 2005). The visual analog scale (VAS), a 10-centimeter line anchored by numbers or words “no pain” on the left, and “worst pain” on the right is another measure of pain intensity with established reliability and validity (Tesler, Savedra, and Holzemer, et al., 1991). It requires a higher degree of abstraction than the NRS, but it cannot be used in telephone follow-up. The domain of emotional response includes all aspects of negative affect or distress secondary to pain such as anxiety, depression, fear, distress, dysphoria, or unhappiness. Behaviors indicating avoidance, withdrawal, or resistance need to be assessed. In children 8 years and older the PedIMMPACT group recommends the use of the Adolescent Pediatric Pain Tool (APPT) (Savedra, Holzemer, and Tesler, 1993), which allows children to describe the quality of the pain using a word list. The 56 words are grouped according to sensory, affective, and evaluative qualities of pain; it has been validated and can be used for children 8 years of age and over Pain that persists for 3 months or more or beyond the expected period of healing is defined as chronic pain (Merskey and Bogduk, 1994). Complex regional pain syndrome and chronic daily headache are the most common chronic pain conditions in children. Pain that is episodic and recurs is defined as recurrent pain. The time frame within which episodes of pain recur is at least 3 months. Recurrent pain in children includes migraine headache, episodic sickle cell pain, recurrent abdominal pain, and recurrent limb pain. van Dijk, McGrath, Pickett, et al (2006) reported that 57% of school-age children were having at least one recurrent pain (headaches, stomach pains, growing pains), and at least 6% had one or more chronic pain (disease related, back pain). Chronic and recurrent pain adversely affects the psychosocial and physical well-being of children. The domains for the assessment of chronic or recurrent pain are the same for acute pain (pain intensity global judgment of satisfaction with treatment, symptoms and adverse events, physical functioning, emotional functioning, economic factors) and two additional domains (role functioning and sleep). Because the time course of chronic and recurrent pain is different from that of acute pain, measures used to assess the impact of chronic and recurrent pain must consider timing and duration as key factors. Pain diaries are commonly used to assess pain symptoms and response to treatment in children and adolescents with recurrent and chronic pain (Ely, Dampier, Gilday, et al., 2002; Dampier, Ely, Brodecki, et al., 2002a, 2002b; Palermo and Valenzuela, 2003; Palermo, Valenzuela, and Stork, 2004; Stinson, Stevens, Feldman, et al., 2008; Stone, Broderick, Schwartz, et al., 2003). Most pain diaries use NRSs or VASs with varying anchors such as faces scales or words. Children as young as 6 years have been included in diary studies. Conventional paper-and-pencil measures have been associated with several limitations such as poor compliance, missing data, hoarding responses, and back-and-forward filling (Palermo and Valenzuela, 2003; Stone, Broderick, Schwartz, et al., 2003). An increasing number of studies are converting paper diaries into electronic diaries for use in school-age children and adolescents with recurrent or chronic pain (Palermo, Valenzuela, and Stork, 2004; Stinson, Stevens, Feldman, et al., 2008; Stone, Broderick, Schwartz, et al., 2003). Electronic diaries were found to show higher accuracy of children’s diary responses and higher compliance rates when compared to the paper format. However, electronic diaries are more expensive and may have a number of logistic issues that must be resolved. The PedIMMPACT group recommends the same approach for measuring global judgment of satisfaction with treatment, symptoms, and adverse events. The physical functioning domain in chronic and recurrent pain is focused on activities of everyday life such as sitting or walking or more vigorous activities such as running and other sports. The recommendation is to use a measure such as the Functional Disability Inventory (Walker and Greene, 1991, No. 43) for assessing physical functioning in school-age children and adolescents. The Functional Disability Inventory assesses the child’s ability to perform everyday physical activities and has established psychometric properties with different populations (Claar and Walker, 2006; Reid, Lang, and McGrath, 1997; Vervoort, Gougert, Eccleston, et al., 2006). For younger children (less than 7 years), the PedsQL developed by Varni, Seid, and Rode (1999) is recommended for assessing the physical functioning domain as it relates to pain. The PedsQL is a multidimensional scale with both parent- and child-report versions. It assesses (1) physical functioning, (2) emotional functioning, (3) social functioning, and (4) school functioning. The emotional functioning domain most often refers to depression and anxiety because they are elevated in children with chronic and recurrent pain (Palermo, 2000). However, most of these children do not have clinical levels of anxiety or depression. The Children’s Depression Inventory (Kovacs, 1981) and the Revised Child Anxiety and Depression Scale (Chorpita, Yim, and Moffitt, et al., 2000) have been used to assess anxiety and depression in children and adolescents with chronic or recurrent pain. Chronic and recurrent pain can significantly interfere with the roles that children and adolescents perform such as being a student, friend, and family member. School attendance is used as a measure of role functioning in school-age children with chronic or recurrent pain. Absence from school is an important measure of fulfillment of the role of student. Other measures such as the PedsQL (Varni, Seid, and Rode, 1999) and PedMIDAS (Hershey, Powers, Vockell, et al., 2001; 2004) have been validated for measurement of role functioning in these children. Sleep disruption is also common in chronic and recurrent pain. More than half of children with pain-related conditions (headache, juvenile idiopathic arthritis, or sickle cell disease) report difficulties sleeping (Walters and Williamson, 1999; Palermo and Kiska, 2005). Sleep diaries in which the child (or parent) keeps a record of the time to go to bed, fall asleep, and wake up are useful for assessment of pain interference with sleep. The sleep diary was validated with sleep actigraphy in healthy children ages 13 and 14 years (Gaina, Sekine, and Chen, 2004). In addition, the Sleep Habits Questionnaire (Owens, Spirito, McGuinn, 2000) may be useful for assessing sleep behaviors in school-age children with chronic or recurrent pain. Several cognitive skills such as measurement, classification, and seriation (the ability to accurately place in ascending or descending order) become explicit between approximately 7 and 10 years of age. Older children are able to use the 0-to-10 NRS that is currently used by adolescents and adults. However, the use of the 0-to-10 NRS is only an assessment of pain intensity, which may not change in some pain states (Jacob, Miaskowski, Savedra, et al., 2003a). Other dimensions such as pain quality, pain location, and spatial distribution of pain may change without a change in pain intensity. Two multidimensional assessment tools that assess not only pain intensity but also pain location and pain quality have been well validated in children 8 years and older. Modeled after the McGill Pain Questionnaire (Melzack, 1975), the APPT is a multidimensional pain instrument for children and adolescents that is used to assess three dimensions of pain: location, intensity, and quality (Fig. 30-3). The APPT is a one-page, two-sided instrument with a front and back body outline on one side (Savedra, Tesler, Holzemer, et al., 1989; Savedra, Holzemer, Tesler, et al., 1993). On the back side is a 100-mm word-graphic rating scale (Tesler, Savedra, Holzemer, et al., 1991) and a pain descriptor list (Wilkie, Holzemer, Tesler, et al., 1990). Each of the three components of the APPT is scored separately. The body outline is scored by placing a clear plastic template overlay with 43 body areas on the body outline diagram. An estimate of the pervasiveness of the pain is made by counting the number of body areas marked. A ruler or micrometer preprinted on the APPT is used to score the word-graphic rating scale. The number of millimeters from the left side of the scale to the point marked by the child is measured; the numeric value provides an overall evaluation of the amount of pain the child is experiencing. The total number of words on the descriptor list is counted; scores range from 0 to 56. The clinician then counts the number of words selected in each of three categories—evaluative (0-8), sensory (0-37), and affective (0-11)—and calculates a percentage score for each one (Savedra, Holzemer, Tesler, et al., 1993). An advantage to using the APPT is that in some pain states pain-intensity ratings do not change, but pain location and spatial distribution of pain may decrease over time (Jacob, Miaskowski, Savedra, et al., 2003a). The total surface area may decrease, but some children may perceive the remaining sites as equal in pain intensity. In addition to pain location, assessments of pain quality may be able to distinguish the presence of the different dimensions of pain (temporal, affective, evaluative, and sensory). Words may not be quantifiable on NRSs yet represent the pain experience such as horrible and terrible from the evaluative dimension, screaming and terrifying from the affective dimension, or sharp and stabbing from the sensory dimension. The different qualities of pain may also represent whether pain is of an ischemic and inflammatory nature in the cutaneous, subcutaneous, and musculoskeletal tissues, as opposed to pain that is more neuropathic, which may be described using words such as shooting, burning, or shocklike (McCaffery and Pasero, 1999). The Pediatric Pain Questionnaire (PPQ) is a multidimensional pain instrument to assess patient and parental perceptions of the pain experience in a manner appropriate for the cognitive-developmental level of children and adolescents. The PPQ represents an attempt to assess the complexities of pediatric chronic, recurrent pain and targeted chronic musculoskeletal pain in children with juvenile rheumatoid arthritis. It consists of eight questions: (1) the pain history, (2) pain language, (3) the colors children associate with pain, (4) the emotions they experience, (5) their worst pain experiences, (6) the ways they cope with pain, (7) the positive aspects of pain, and (8) the location of their current pain. The PPQ includes three components: (1) VASs; (2) color-coded rating scales; and (3) verbal descriptors to provide information about the sensory, affective, and evaluative dimensions of chronic pain (Varni, Thompson, and Hanson, 1987). It also has information about the child’s and family’s pain history, symptoms, pain-relief interventions, and socioenvironmental situations that may influence pain. The child, parent, and health care provider complete the form separately. The number of pain measures available for use in infants and young children has increased dramatically and adds a layer of complexity to the assessment of pain in children. The current trend supports a common metric for measurement of pain in children (von Baeyer and Hicks, 2000). Most instruments consist of 0 for no pain to a range of 4 to 160 for the top anchors in pain measures. A pain score of 5 may mean a lot of pain (if a 0 to 5 scale is used) or very little (if a 0 to 100 scale is used), and it may not be clearly specified which score corresponds to which scale. Other health care providers who do not specialize in pediatric pain may be confused by the available instruments and scoring methods and may not be able to determine the effectiveness of interventions by the pain score documented. An advantage to using a common metric is that a certain score may be considered as the point at which an intervention is required or a point at which relief may be considered adequate (von Baeyer and Hicks, 2000). The 0-to-10 system was reported to be preferred by health care providers and would make pain scores easier to read, interpret, and integrate into research and practice.
Pain Assessment and Management in Children
Pain Assessment
Assessment of Acute Pain
Pain Intensity
AGES OF USE
RELIABILITY AND VALIDITY
VARIABLES
SCORING RANGE
Objective Pain Score (OPS) (Hannallah, Broadman, Belman, et al., 1987)
4 months-18 years
Concurrent validity with linear analog pain scale, Spearman’s r: 0.721 with scores ≥6 and 0.419 with scores <6
Interrater agreement, coefficient alpha: 0.986 for one rater and 0.983 for the other
Concurrent validity with CHEOPS, Pearson correlation coefficient: 0.88 and 0.94
Blood pressure (0-2)
Crying (0-2)
Moving (0-2)
Agitation (0-2)
Verbal evaluation or body language (0-2)
0 = no pain; 10 = worst pain
Children’s Hospital of Eastern Ontario Pain Scale (CHEOPS) (McGrath, Johnson, Goodman, et al., 1985)
1-5 years
Interrater reliability: 90%-99.5%
Internal correlation: significant correlations between pairs of items
Concurrent validity between CHEOPS and visual analog scale (VAS): 0.91; between individual and total scores of CHEOPS and VAS: 0.50-0.86
Construct validity with preanalgesia and postanalgesia scores: 6.3-9.9
Cry (1-3)
Facial (0-2)
Child verbal (0-2)
Torso (1-2)
Touch (1-2)
Legs (1-2)
4 = no pain; 13 = worst pain
Nurses Assessment of Pain Inventory (NAPI) (Stevens, 1990)
Newborn-16 years
Not tested by original author; later tested by Joyce, Schade, Keck, et al. (1994)
Interrater agreement: weighted kappa 0.37-0.80
Discriminant validity: statistically significant differences between preanalgesia and postanalgesia scores (p < 0.0001)
Reliability: Cronbach alpha: 0.35-0.69
Body movement (0-2)
Facial (0-3)
Touching (0-2)
0 = no pain; 7 = worst pain
Behavioral Pain Score (BPS) (Robieux, Kumar, Radhakrishnan, et al., 1991)
3-36 months
Original article stated, “reliability of the VAS and BPS scores was tested by a k test”; no further testing of reliability or validity mentioned
Facial expression (0-2)
Cry (0-3)
Movements (0-3)
0 = no pain; 8 = worst pain
Modified Behavioral Pain Scale (MBPS) (Taddio, Nulman, Koren, et al., 1995)
4-6 months
Concurrent validity between MBPS and VAS scores: correlation coefficient 0.68 (p < 0.001) and 0.74 (p < 0.001)
Construct validity using prevaccination and postvaccination scores with EMLA vs. placebo: significantly lower scores with EMLA (p < 0.01)
Internal consistency of items: significant correlations between items
Interrater agreement ICC: 0.95, p < 0.001
Test-retest reliability: 0.95, p < 0.001
Facial expression (0-3)
Cry (0-4)
Movements (0, 2, 3)
0 = no pain; 10 = worst pain
Riley Infant Pain Scale (RIPS) (Schade, Joyce, Gerkensmeyer, et al., 1996)
<36 months and for children with cerebral palsy
Interrater agreement using intraclass correlation coefficient: 0.53-0.83, p < 0.0001
Discriminant validity using Mann-Whitney U test with preanalgesia and postanalgesia scores: statistically significant (p < 0.001)
Sensitivity: 0.23-0.31
Specificity: 0.86-0.90
Interrater reliability using two-way cross-tabulations and kappa statistics (r[87] = 0.94; p < 0.001) and kappa values above 0.50 for each category
0: Neutral face/smiling, calm, sleeping quietly, no cry, consolable, moves easily
1: Frowning/grimace, restless body movements, restless sleep, whimpering, winces with touch
2: Clenched teeth, moderate agitation, sleeps intermittently, difficult to console, cries with touch
3: Full cry expression, thrashing/flailing, sleeping prolonged periods interrupted by jerking or no sleep, screaming/high-pitched cry, inconsolable, screams when touched/moved
0 = no pain; 3 = worst pain
FLACC Postoperative Pain Tool (Merkel, Voepel-Lewis, Shayevitz, et al., 1997)
2 months-7 years
Validity using analysis of variance for repeated measures to compare FLACC scores before and after analgesia; preanalgesia FLACC scores significantly higher than postanalgesia scores at 10, 30, and 60 min (p <0.001 for each time)
Correlation coefficients used to compare FLACC pain scores and OPS pain scores; significant positive correlation between FLACC and OPS scores (r = 0.80; p <0.001); positive correlation also found between FLACC scores and nurses’ global ratings of pain (r[47] = 0.41; p <0.005)
Face (0-2)
Legs (0-2)
Activity (0-2)
Cry (0-2)
Consolability (0-2)
0 = no pain; 10 = worst pain
FLACC Scale*
0
1
2
Face
No particular expression or smile
Occasional grimace or frown, withdrawn, disinterested
Frequent- to- constant frown, clenched jaw, quivering chin
Legs
Normal position or relaxed
Uneasy, restless, tense
Kicking or legs drawn up
Activity
Lying quietly, normal position, moves easily
Squirming, shifting back and forth, tense
Arched, rigid, or jerking
Cry
No cry (awake or asleep)
Moans or whimpers, occasional complaint
Crying steadily, screams or sobs, frequent complaints
Consolability
Content, relaxed
Reassured by occasional touching, hugging, or talking to; distractible
Difficult to console or comfort
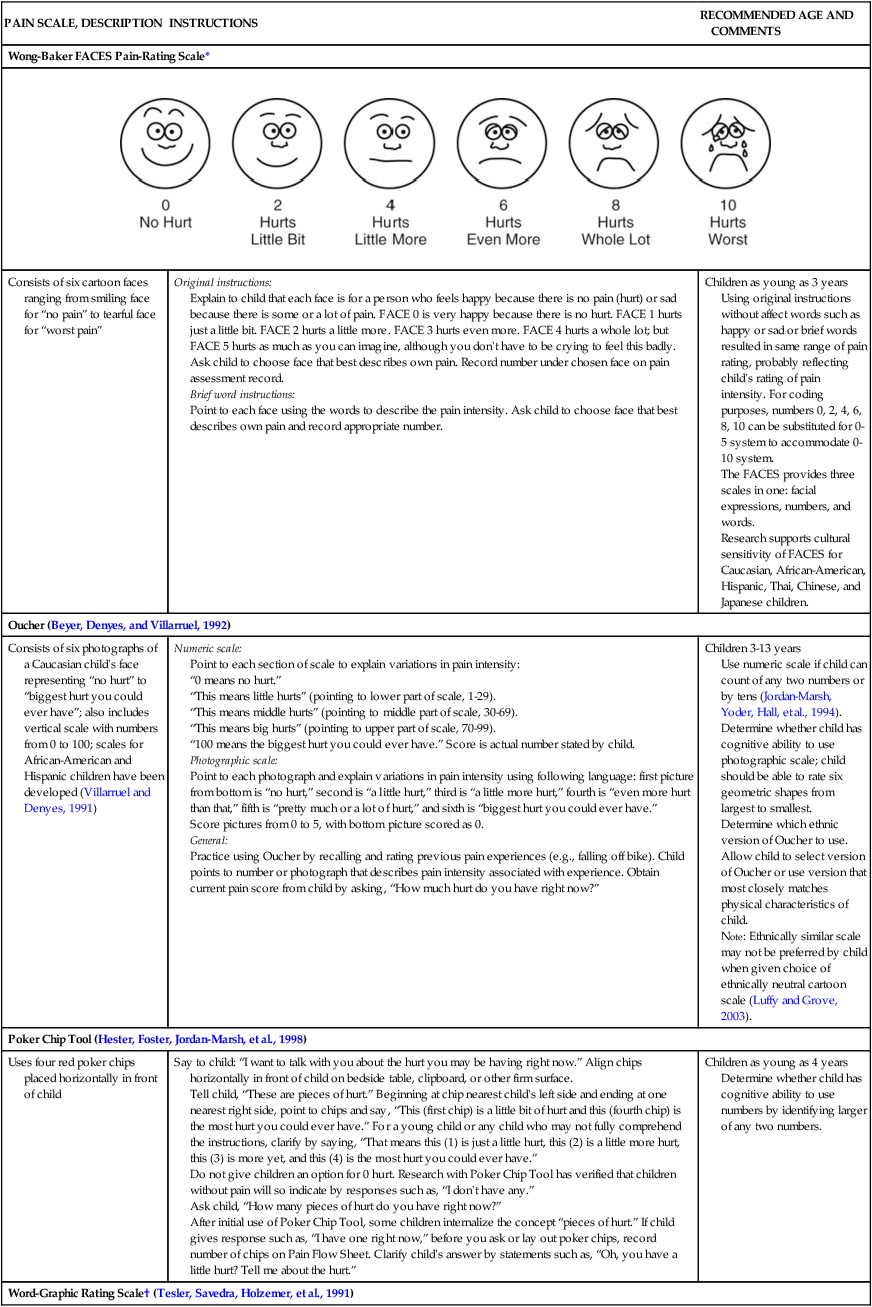
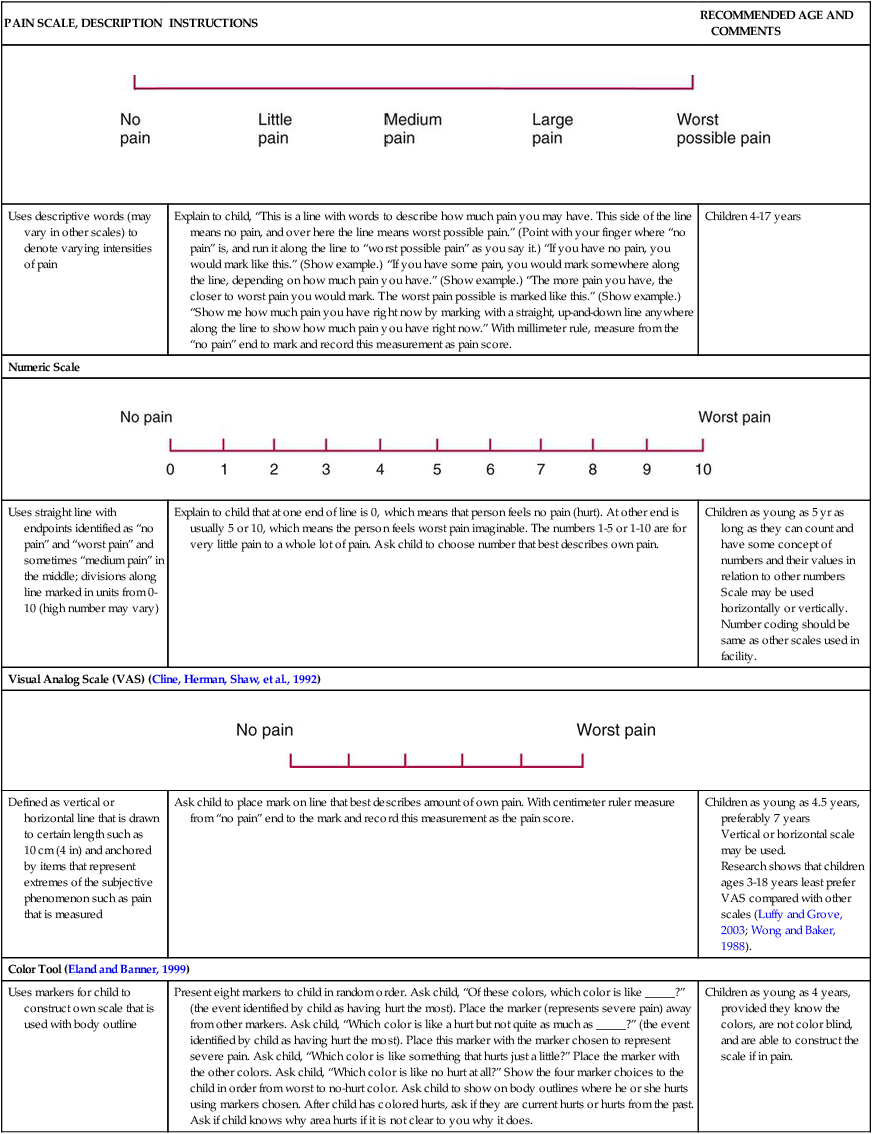
PAIN SCALE, DESCRIPTION
INSTRUCTIONS
RECOMMENDED AGE AND COMMENTS
Wong-Baker FACES Pain-Rating Scale*
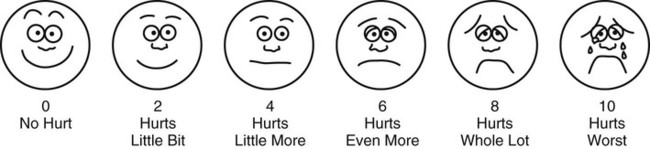
Consists of six cartoon faces ranging from smiling face for “no pain” to tearful face for “worst pain”
Original instructions:
Explain to child that each face is for a person who feels happy because there is no pain (hurt) or sad because there is some or a lot of pain. FACE 0 is very happy because there is no hurt. FACE 1 hurts just a little bit. FACE 2 hurts a little more. FACE 3 hurts even more. FACE 4 hurts a whole lot; but FACE 5 hurts as much as you can imagine, although you don’t have to be crying to feel this badly. Ask child to choose face that best describes own pain. Record number under chosen face on pain assessment record.
Brief word instructions:
Point to each face using the words to describe the pain intensity. Ask child to choose face that best describes own pain and record appropriate number.
Children as young as 3 years
Using original instructions without affect words such as happy or sad or brief words resulted in same range of pain rating, probably reflecting child’s rating of pain intensity. For coding purposes, numbers 0, 2, 4, 6, 8, 10 can be substituted for 0-5 system to accommodate 0-10 system.
The FACES provides three scales in one: facial expressions, numbers, and words.
Research supports cultural sensitivity of FACES for Caucasian, African-American, Hispanic, Thai, Chinese, and Japanese children.
Oucher (Beyer, Denyes, and Villarruel, 1992)
Consists of six photographs of a Caucasian child’s face representing “no hurt” to “biggest hurt you could ever have”; also includes vertical scale with numbers from 0 to 100; scales for African-American and Hispanic children have been developed (Villarruel and Denyes, 1991)
Numeric scale:
Point to each section of scale to explain variations in pain intensity:
“0 means no hurt.”
“This means little hurts” (pointing to lower part of scale, 1-29).
“This means middle hurts” (pointing to middle part of scale, 30-69).
“This means big hurts” (pointing to upper part of scale, 70-99).
“100 means the biggest hurt you could ever have.” Score is actual number stated by child.
Photographic scale:
Point to each photograph and explain variations in pain intensity using following language: first picture from bottom is “no hurt,” second is “a little hurt,” third is “a little more hurt,” fourth is “even more hurt than that,” fifth is “pretty much or a lot of hurt,” and sixth is “biggest hurt you could ever have.”
Score pictures from 0 to 5, with bottom picture scored as 0.
General:
Practice using Oucher by recalling and rating previous pain experiences (e.g., falling off bike). Child points to number or photograph that describes pain intensity associated with experience. Obtain current pain score from child by asking, “How much hurt do you have right now?”
Children 3-13 years
Use numeric scale if child can count of any two numbers or by tens (Jordan-Marsh, Yoder, Hall, et al., 1994).
Determine whether child has cognitive ability to use photographic scale; child should be able to rate six geometric shapes from largest to smallest.
Determine which ethnic version of Oucher to use. Allow child to select version of Oucher or use version that most closely matches physical characteristics of child.
Note: Ethnically similar scale may not be preferred by child when given choice of ethnically neutral cartoon scale (Luffy and Grove, 2003).
Poker Chip Tool (Hester, Foster, Jordan-Marsh, et al., 1998)
Uses four red poker chips placed horizontally in front of child
Say to child: “I want to talk with you about the hurt you may be having right now.” Align chips horizontally in front of child on bedside table, clipboard, or other firm surface.
Tell child, “These are pieces of hurt.” Beginning at chip nearest child’s left side and ending at one nearest right side, point to chips and say, “This (first chip) is a little bit of hurt and this (fourth chip) is the most hurt you could ever have.” For a young child or any child who may not fully comprehend the instructions, clarify by saying, “That means this (1) is just a little hurt, this (2) is a little more hurt, this (3) is more yet, and this (4) is the most hurt you could ever have.”
Do not give children an option for 0 hurt. Research with Poker Chip Tool has verified that children without pain will so indicate by responses such as, “I don’t have any.”
Ask child, “How many pieces of hurt do you have right now?”
After initial use of Poker Chip Tool, some children internalize the concept “pieces of hurt.” If child gives response such as, “I have one right now,” before you ask or lay out poker chips, record number of chips on Pain Flow Sheet. Clarify child’s answer by statements such as, “Oh, you have a little hurt? Tell me about the hurt.”
Children as young as 4 years
Determine whether child has cognitive ability to use numbers by identifying larger of any two numbers.
Word-Graphic Rating Scale† (Tesler, Savedra, Holzemer, et al., 1991)
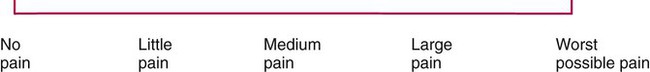
Uses descriptive words (may vary in other scales) to denote varying intensities of pain
Explain to child, “This is a line with words to describe how much pain you may have. This side of the line means no pain, and over here the line means worst possible pain.” (Point with your finger where “no pain” is, and run it along the line to “worst possible pain” as you say it.) “If you have no pain, you would mark like this.” (Show example.) “If you have some pain, you would mark somewhere along the line, depending on how much pain you have.” (Show example.) “The more pain you have, the closer to worst pain you would mark. The worst pain possible is marked like this.” (Show example.) “Show me how much pain you have right now by marking with a straight, up-and-down line anywhere along the line to show how much pain you have right now.” With millimeter rule, measure from the “no pain” end to mark and record this measurement as pain score.
Children 4-17 years
Numeric Scale

Uses straight line with endpoints identified as “no pain” and “worst pain” and sometimes “medium pain” in the middle; divisions along line marked in units from 0-10 (high number may vary)
Explain to child that at one end of line is 0, which means that person feels no pain (hurt). At other end is usually 5 or 10, which means the person feels worst pain imaginable. The numbers 1-5 or 1-10 are for very little pain to a whole lot of pain. Ask child to choose number that best describes own pain.
Children as young as 5 yr as long as they can count and have some concept of numbers and their values in relation to other numbers
Scale may be used horizontally or vertically.
Number coding should be same as other scales used in facility.
Visual Analog Scale (VAS) (Cline, Herman, Shaw, et al., 1992)

Defined as vertical or horizontal line that is drawn to certain length such as 10 cm (4 in) and anchored by items that represent extremes of the subjective phenomenon such as pain that is measured
Ask child to place mark on line that best describes amount of own pain. With centimeter ruler measure from “no pain” end to the mark and record this measurement as the pain score.
Children as young as 4.5 years, preferably 7 years
Vertical or horizontal scale may be used.
Research shows that children ages 3-18 years least prefer VAS compared with other scales (Luffy and Grove, 2003; Wong and Baker, 1988).
Color Tool (Eland and Banner, 1999)
Uses markers for child to construct own scale that is used with body outline
Present eight markers to child in random order. Ask child, “Of these colors, which color is like _____?” (the event identified by child as having hurt the most). Place the marker (represents severe pain) away from other markers. Ask child, “Which color is like a hurt but not quite as much as _____?” (the event identified by child as having hurt the most). Place this marker with the marker chosen to represent severe pain. Ask child, “Which color is like something that hurts just a little?” Place the marker with the other colors. Ask child, “Which color is like no hurt at all?” Show the four marker choices to the child in order from worst to no-hurt color. Ask child to show on body outlines where he or she hurts using markers chosen. After child has colored hurts, ask if they are current hurts or hurts from the past. Ask if child knows why area hurts if it is not clear to you why it does.
Children as young as 4 years, provided they know the colors, are not color blind, and are able to construct the scale if in pain.


Emotional Response
Assessment of Chronic and Recurrent Pain
Multidimensional Measures
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access
