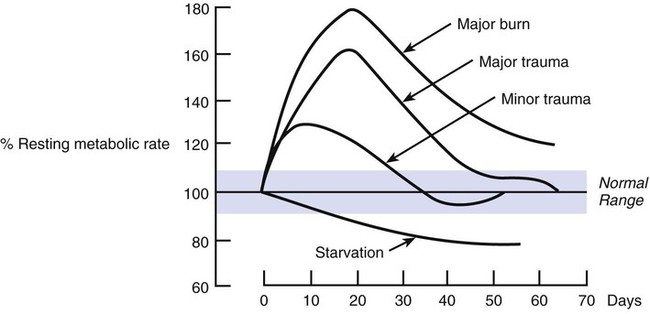
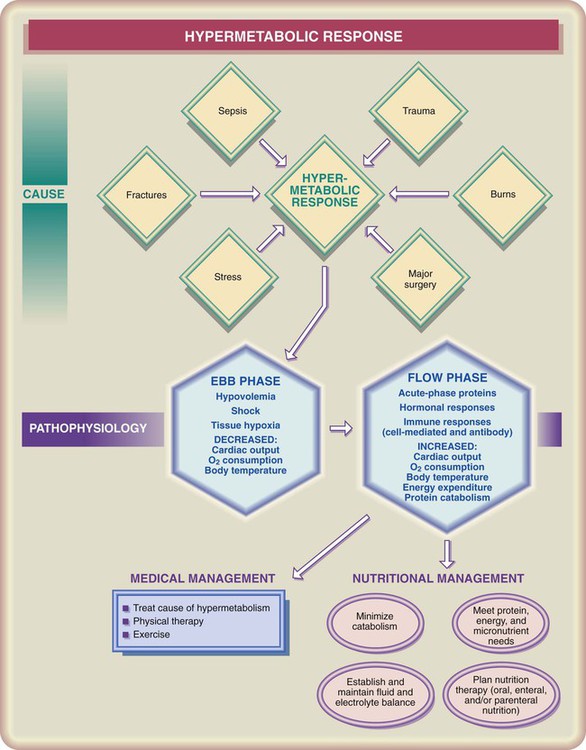
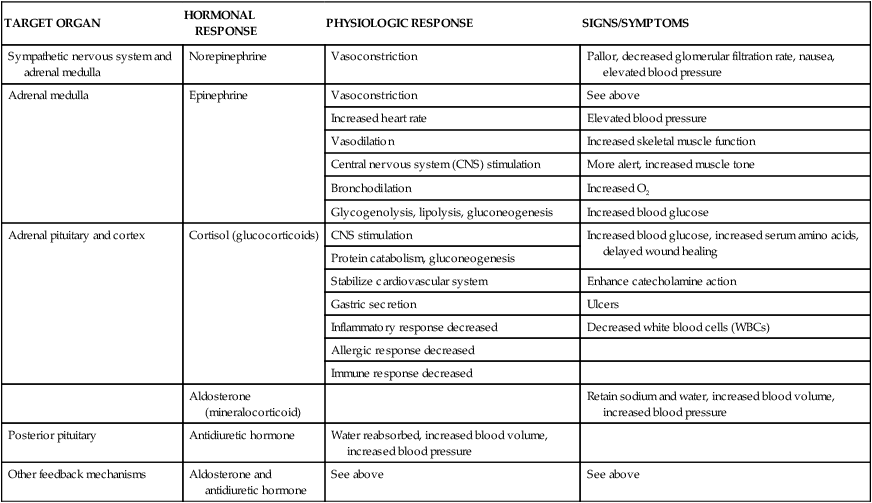
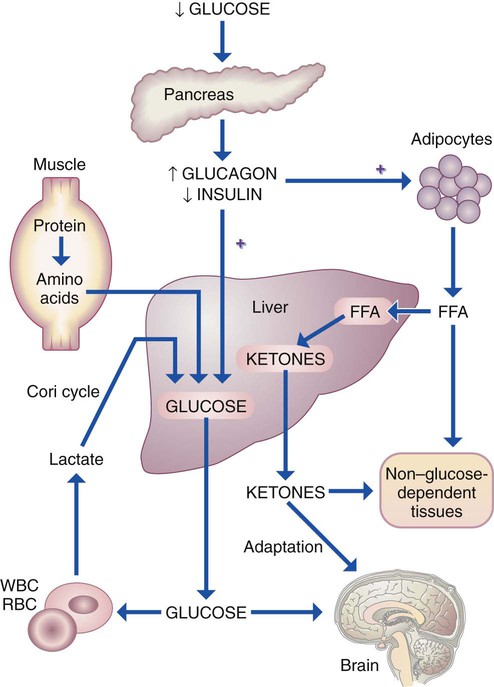
Compromised nutritional status creates a vulnerable immune system by making it difficult to mount both a stress response and an immune response when confronted with a metabolic stress. A number of nutrients are known to affect immune system functioning. It is difficult to determine which specific nutrient factor results in symptoms when a patient is malnourished because of overlapping nutrient deficiencies combined with illness and accompanied by weakness, anorexia, and infection.1 Immune system components affected by malnutrition include mucous membrane, skin, gastrointestinal tract, T-lymphocytes, macrophages, granulocytes, and antibodies. The effects on the mucous membrane are that the microvilli become flat, which reduces nutrient absorption and decreases antibody secretions. Integrity of the skin may be compromised as it loses density, and wound healing is slowed. Injury to the gastrointestinal tract because of malnutrition may increase risk of infection-causing bacteria spreading from inside the tract to outside the intestinal system. T-lymphocytes are affected as the distribution of T cells is depressed. The effect on macrophages and granulocytes requires that more time is needed for phagocytosis kill time and lymphocyte activation to occur. Antibodies may be less available because of damage to the antibody response1. Table 15-1 outlines how specific nutrient deficiencies affect immune system functions; note that fat and water-soluble vitamins, fatty acids, minerals, and protein are important for adequate functioning of most immune system components. TABLE 15-1 ROLE OF NUTRIENTS AND NUTRITIONAL STATUS ON IMMUNE SYSTEM COMPONENTS According to Gould,2 the body’s constant response to minor changes brought about by needs or environment was first noted in 1946 by Hans Selye when he described the “fight or flight” response, or general adaptation syndrome (GAS). The body constantly responds to minor changes to maintain homeostasis. Research following Selye’s work has identified that the stress response involves an integrated series of actions that include the hypothalamus and hypophysis, sympathetic nervous system, adrenal medulla, and adrenal cortex.2 Significant effects of this response to stress are outlined in Table 15-2. These responses to stress produce multiple changes in metabolic processes throughout the body. The effect of different levels of stress on metabolic rate is illustrated in Figure 15-1. TABLE 15-2 EFFECTS OF THE STRESS RESPONSE* *Possible complications include hypertension, tension headaches, insomnia, diabetes mellitus, infection, heart failure, peptic ulcer, and fatigue. Data from Gould BE: Pathophysiology for the health-related professions, ed 3, Philadelphia, 2006, Saunders. Liver glycogen is used to maintain normal blood glucose levels to provide energy for cells. Although readily available, this source of energy is limited, and glycogen stores are usually depleted after 8 to 12 hours of fasting. Unlike glycogen stores, lipid (triglyceride) stores may be substantial, and the body also begins to mobilize this energy source. As the amount of liver glycogen decreases, mobilization of free fatty acids from adipose tissue increases to provide energy needed by the nervous system. After approximately 24 hours without energy intake (especially carbohydrates), the prime source of glucose is from gluconeogenesis.3 Some body cells, brain cells in particular, use mainly glucose for energy. During early starvation (about 2 to 3 days of starvation), the brain uses glucose produced from muscle protein. As muscle protein is broken down for energy, the level of branched-chain amino acids (BCAA) consisting of leucine, isoleucine, and valine increases in circulation, although they are primarily metabolized directly inside muscle.3 The body does not store any amino acids as it does glucose and triglycerides; therefore, the only sources of amino acids are lean body mass (muscle tissue), vital organs including heart muscle, or other protein-based body constituents such as enzymes, hormones, immune system components, or blood proteins. By the second or third day of starvation, approximately 75 g of muscle protein can be catabolized daily, a level inadequate to supply full energy needs of the brain.3 At this point, other sources of energy become more available. Fatty acids are hydrolyzed from the glycerol backbone, and both free fatty acids and glycerol are released into the bloodstream. Free fatty acids are used as indicated earlier, and glycerol can be used by the liver to generate glucose via the process of gluconeogenesis. As starvation is prolonged, the body preserves proteins by mobilizing more and more fat for energy (Figure 15-2). Ketone body production from fatty acids is accelerated, and the body’s requirement for glucose decreases. Although some glucose is still vital for brain cells and red blood corpuscles, these and other body tissues obtain the major proportion of their energy from ketone bodies. Muscle protein is still being catabolized but at a much lower rate, which prolongs survival. The body’s response to stress can be summarized by two phases: ebb phase and flow phase (Figure 15-3). The ebb phase, or early phase (Table 15-3), begins immediately after the injury and is identified by decreased oxygen consumption, hypothermia (lowered body temperature), and lethargy. The major medical concern during this time is to maintain cardiovascular effectiveness and tissue perfusion. As the body responds to injury, the ebb phase evolves into the flow phase, usually about 36 to 48 hours after injury.4 The flow phase is characterized by increased oxygen consumption, hyperthermia (increased body temperature), and increased nitrogen excretion, as well as expedited catabolism of carbohydrate, protein, and triglycerides to meet the increased metabolic demands.4 The flow stage will last for days, weeks, or months until the injury is healed. TABLE 15-3 METABOLIC RESPONSES TO SEVERE STRESS Nutrients affected by hypermetabolic stress include protein, vitamins, and minerals, as well as related nutritional concerns for total energy and fluid intake. During moderate metabolic stress, protein requirements have been reported to increase from 0.8 g/kg body weight (amount recommended for an average healthy adult) to 1 to 1.5 g/kg body weight and for severe stress (e.g., thermal injuries exceeding 20% total body surface area) can rise to 1.5 to 2 g/kg body weight.1 These levels are based on sufficient energy consumption to allow for protein synthesis. Requirements of vitamins and minerals all increase during stress. Tissue repair especially depends on adequate intakes of vitamin C, zinc, calcium, magnesium, manganese, and copper. At the least, Dietary Reference Intake (DRI) levels of nutrients should be consumed, preferably from foods rather than from vitamin or mineral supplements. Achieving requirements through food intake also supports provision of sufficient kcal to meet increased energy demands during critical illness. Several formulas have been used to determine the energy needs of patients experiencing hypermetabolic stress. The Mifflin-St. Jeor equation best predicts resting metabolic rate (RMR)5. Total energy expenditure can be determined by multiplying RMR by activity level and an injury factor.6 Activity level considers energy required if the patient is confined to bed or is ambulatory. Severity of injury is a factor based on whether the injury is caused by major or minor surgery, mild to severe infection, skeletal or blunt trauma, or burns (based on percentage of body surface area affected) (Box 15-1).
Nutrition and Metabolic Stress
![]() http://evolve.elsevier.com/Grodner/foundations/
http://evolve.elsevier.com/Grodner/foundations/ ![]() Nutrition Concepts Online
Nutrition Concepts Online
Immune System
Role of Nutrition
IMMUNE SYSTEM COMPONENT
EFFECTS OF MALNUTRITION
VITAL NUTRIENTS
Mucus
Decreased antibody secretions
Vitamin B12, biotin, vitamins B6 and C
Gastrointestinal tract
Flat microvilli, increased risk of bacterial spread to outside GI tract
Arginine, omega-3 fatty acids
Skin
Integrity compromised, density reduced, wound healing slowed
Protein, vitamins A and C, niacin, zinc, copper, linoleic acid, vitamin B12
T-lymphocytes
Depressed T-cell distribution
Protein, arginine, omega-3 fatty acids, vitamins A, B12, B6, folic acid, thiamine, riboflavin, niacin, pantothenic acid, zinc, iron
Macrophages and granulocytes
Longer time for phagocytosis kill time and lymphocyte activation
Protein, vitamins A, C, B12, B6, folic acid, thiamine, riboflavin, niacin, zinc, iron
Antibodies
Reduced antibody response
Protein, vitamins A, C, B12, B6, folic acid, thiamine, biotin, riboflavin, niacin
The Stress Response
TARGET ORGAN
HORMONAL RESPONSE
PHYSIOLOGIC RESPONSE
SIGNS/SYMPTOMS
Sympathetic nervous system and adrenal medulla
Norepinephrine
Vasoconstriction
Pallor, decreased glomerular filtration rate, nausea, elevated blood pressure
Adrenal medulla
Epinephrine
Vasoconstriction
See above
Increased heart rate
Elevated blood pressure
Vasodilation
Increased skeletal muscle function
Central nervous system (CNS) stimulation
More alert, increased muscle tone
Bronchodilation
Increased O2
Glycogenolysis, lipolysis, gluconeogenesis
Increased blood glucose
Adrenal pituitary and cortex
Cortisol (glucocorticoids)
CNS stimulation
Increased blood glucose, increased serum amino acids, delayed wound healing
Protein catabolism, gluconeogenesis
Stabilize cardiovascular system
Enhance catecholamine action
Gastric secretion
Ulcers
Inflammatory response decreased
Decreased white blood cells (WBCs)
Allergic response decreased
Immune response decreased
Aldosterone (mineralocorticoid)
Retain sodium and water, increased blood volume, increased blood pressure
Posterior pituitary
Antidiuretic hormone
Water reabsorbed, increased blood volume, increased blood pressure
Other feedback mechanisms
Aldosterone and antidiuretic hormone
See above
See above
Starvation
![]() Severe Stress
Severe Stress
EBB PHASE
FLOW PHASE
↓ Oxygen consumption
↑ Oxygen consumption
↓ Cardiac output
↑ Cardiac output
↓ Plasma volume
↑ Plasma volume
Hypothermia
Hyperthermia
↑ Nitrogen excretion
↓ Insulin levels
Normal or elevated insulin levels
Hyperglycemia
Hyperglycemia
Hypovolemia
Hypotension
↑ Lactate
Normal lactate
↑ Free fatty acids
↑ Free fatty acids
↑Catecholamines, glucagon, cortisol
↑ Catecholamines, glucagon, cortisol
Insulin resistance
↑ Insulin resistance

Nutrition and Metabolic Stress
Get Clinical Tree app for offline access