On completing this chapter, you will be able to do the following: 1. Provide one reason for the development of nursing theories. 2. Briefly describe each of the following theories as they relate to the nursing process: • Maslow’s Hierarchy of Human Needs Theory • Rosenstock’s Health Belief Model • Orem’s Self-Care Deficit Theory • Leininger’s Culture Care Theory • Peplau’s Interpersonal Relations Theory • Sister Callista Roy’s Adaptation Model • Nightingale’s Environmental Model • Jean Watson’s Theory of Human Care 3. Briefly explain the importance of nursing research. 4. Compare and contrast quantitative and qualitative research studies. 5. Define evidence-based-practice. 6. Explain the three elements of evidence-based practice (EBP). 7. Briefly describe how best evidence for practice is determined by systematic reviews of research studies. 8. Discuss how your site of clinical experience adopts evidence-based guidelines for nursing interventions. 9. Explain the LPN/LVN’s role in nursing research and evidence-based practice. 1. Abraham Maslow’s theory states that certain internal, external, physical, and psychological needs are common to all people. 2. Common needs are arranged in a hierarchy. 3. Unmet needs create tension, which motivates the person to react to meet the need. 4. When needs are met, the person is no longer aware of the need, and the need (now met) no longer motivates them. Figure 10-1 provides examples in identifying patient care priorities and responding to the needs according to the patient level of functioning. It is important to remember that a person may be functioning on more than one level of needs at the same time. Read the list on the lowest level of needs again. Individuals go back to the physiologic level periodically to satisfy basic needs—for example, nutrition. The first data collection (assessment) of a patient is the lowest level of needs: • Physiologic needs: Oxygen, food, water, elimination, safety, sleep, activity, mental stimulation, sexual procreation (e.g., the nurse collects data on whether the patients are eating enough to maintain their strength and health, if they have relief from pain, and if interventions are planned with the patients to meet the need). Once physiologic needs are met, data can be collected on safety and security needs. • Safety needs: Security, freedom from harm, protection (e.g., data are collected on real or imagined safety needs—for example, do you need more than one nurse to move the patient safely from the bed to the toilet?). The primary areas that involve hospital nursing care are the first two levels: physiologic and safety needs. • Love and belonging needs: Love, affection, and companionship (e.g., data are collected on whether the patient has a support system to assist with care once hospitalization is over). This is a part of discharge planning to be sure the patient has support meeting needs posthospitalization. The nurse may be involved in doing follow-up care in the home after hospitalization (home health, visiting nurse service, etc.). • Esteem needs: Respect and recognition (e.g., data are collected on what the patient is doing or can do that will assist in earning a positive sense of self). Is the person able to do volunteer work or join a Senior Center that has activities, provides an opportunity to help others, and offers meals at a reasonable price)? Once esteem needs are met, the individual may be ready to focus on self-actualization. A parish nurse, for example, may be providing care at this level. • Self-actualization: This is the highest level of needs, and not everyone attains this level. This involves maximum realization and fulfillment of the individual’s potential. Dorothea Orem’s Self-Care Deficit Theory is a general theory that consists of three subtheories: 1. Self-care: This involves a goal that is directed toward a safer environment for life, health, and well-being. (Ideally, individuals learn to respond to health cues in themselves or the environment as a way to maintain personal health.) 2. Self-care deficit: Personal care does not meet therapeutic self-care demands. (The individual does not recognize or know what to do in regard to personal health situations.) 3. Nursing system: Nurses empower the patient through their interpersonal relationship to help meet their self-care demands. (Nursing responds to the person’s care needs totally, partially, or in a supportive role according to the need.) Leininger proposed three modes to guide nursing decisions when providing care: 1. Cultural care preservation or maintenance. This means assisting persons of particular cultures to maintain care values that help them to maintain health or restore health. As an example, some cultures use periodic “cupping” (bloodletting) as a way to relieve symptoms of hemochromatosis (excess iron deposits throughout the body). A method in other cultures is to periodically give blood at a blood blank to reduce the hematocrit (the percentage of your blood that is made up of red blood cells). 2. Cultural care accommodation or negotiation. In some cultures, Vicks VapoRub is placed in the nostrils, which can potentially be aspirated and lead to pneumonia. The visiting nurse demonstrated placing the Vicks on the chest and neck and rubbing it in a soothing manner. A warm cloth was placed on the chest for the night. The vapor’s fumes relieved the congestion. 3. Culture care repatterning or restructuring. Leininger’s theory is concerned with respecting cultural differences and yet providing a safe and protective environment (e.g., in some cultures, mud is placed on the infant’s umbilicus after delivery). Because of concern for local and systemic infection, the visiting nurse provided clean pads. The nurse demonstrated their use, how to clean the area, and how to leave the area uncovered for a period so the umbilicus could be exposed to the air. Peplau describes four overlapping phases: • Orientation: The patient seeks assistance because of a felt need. A problem has been identified, and the nurse works with the patient to help him or her recognize the problem. The process is often complex, but personal and social growth can develop during this step. • Identification: During this phase, the patient understands the situation and responds to the nurse who supplies the needed help. • Exploitation: During this phase, the patient begins to depend on the nurse and uses the help offered, exploring all possibilities. • Resolution: The dependent behavior that developed must now be given up as the therapeutic relationship comes to an end. How the nurse handles this phase is crucial because faulty resolution can possibly end with vague physical symptoms.
Nursing Theory, Research, and Evidence-Based Practice
Nursing theories
Rationale for Theories
Abraham maslow’s Human needs theory
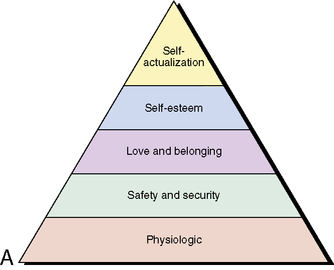
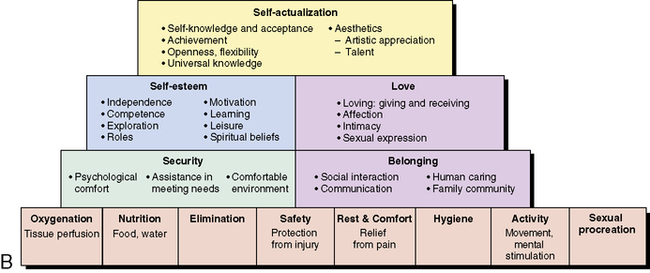
Applying Maslow’s Human Needs Theory to the Nursing Process
Orem’s self-care deficit theory
Madeline Leininger’s Culture Care Theory
Hildegard Peplau’s Interpersonal Relations Theory
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nursing Theory, Research, and Evidence-Based Practice
Get Clinical Tree app for offline access

