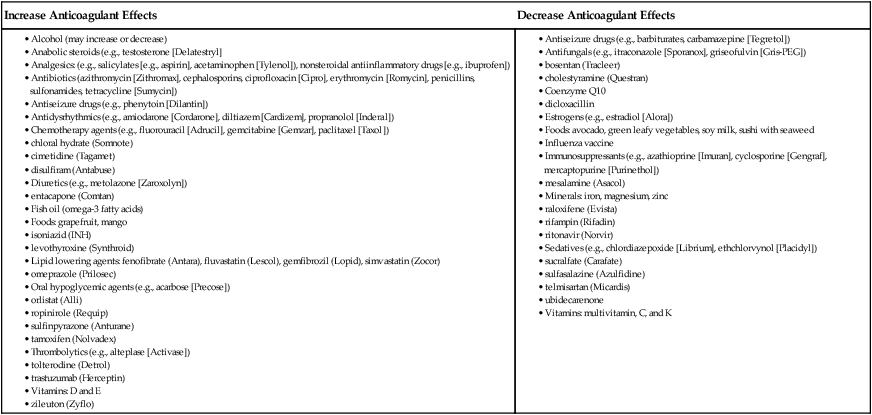
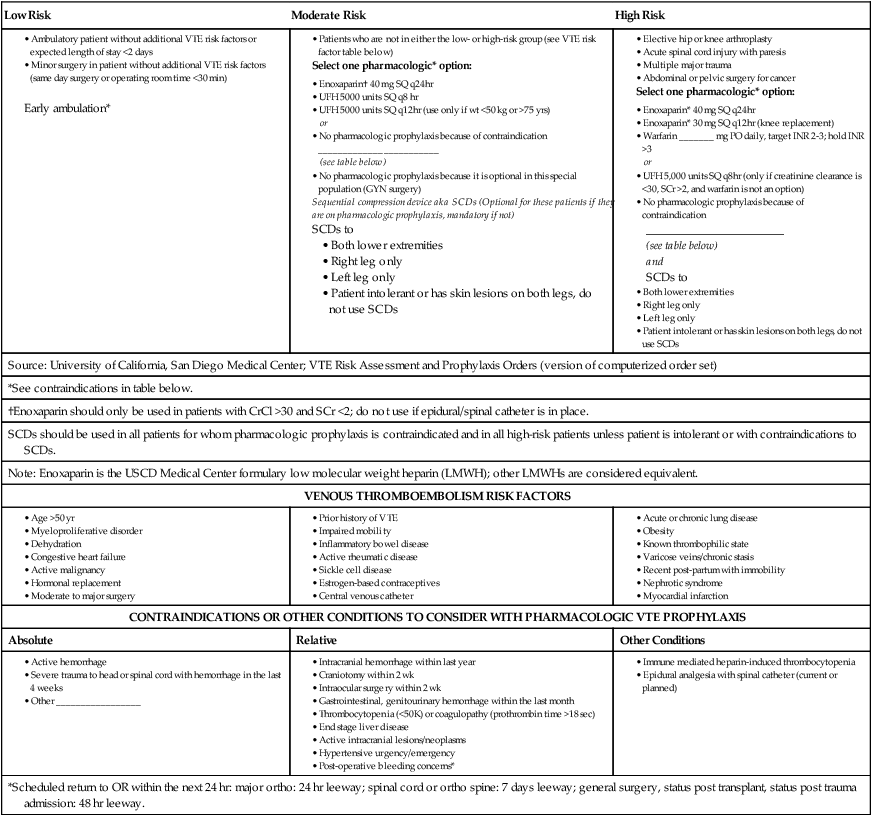
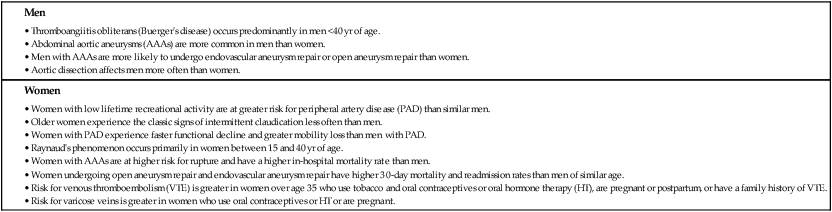
Chapter 38 Deirdre D. Wipke-Tevis and Kathleen A. Rich 1. Relate the major risk factors to the etiology and pathophysiology of peripheral artery disease (PAD). 2. Describe the clinical manifestations, collaborative care, and surgical and nursing management of PAD of the lower extremities. 3. Plan appropriate nursing care for the patient with acute arterial ischemic disorders of the lower extremities. 4. Differentiate the pathophysiology, clinical manifestations, collaborative care, and nursing management of thromboangiitis obliterans (Buerger’s disease) and Raynaud’s phenomenon. 5. Differentiate the pathophysiology, clinical manifestations, and collaborative care of different types of aortic aneurysms. 6. Select appropriate nursing interventions for a patient undergoing an aortic aneurysm repair. 7. Describe the pathophysiology, clinical manifestations, collaborative care, and nursing management of aortic dissection. 8. Evaluate the risk factors predisposing patients to the development of superficial vein thrombosis and venous thromboembolism (VTE). 9. Differentiate between the clinical characteristics of superficial vein thrombosis and VTE. 10. Compare and contrast the collaborative care and nursing management of patients with superficial vein thrombosis and VTE. 11. Prioritize the key aspects of nursing management of the patient receiving anticoagulant therapy. 12. Relate the pathophysiology and clinical manifestations to the collaborative care of patients with varicose veins, chronic venous insufficiency, and venous leg ulcers. Problems of the vascular system include disorders of the arteries, veins, and lymphatic vessels. Arterial disorders are classified as atherosclerotic, aneurysmal, and nonatherosclerotic vascular diseases. Atherosclerotic vascular disease is divided into coronary, cerebral, peripheral, mesenteric, and renal artery disease.1 This chapter discusses peripheral artery disease; aortic aneurysm and dissection; and venous diseases, specifically venous thromboembolism and chronic venous insufficiency. eTABLE 38-1 DRUGS, VITAMINS, MINERALS, AND SUPPLEMENTS THAT INTERACT WITH ORAL ANTICOAGULANTS* eTABLE 38-2 SAMPLE VENOUS THROMBOEMBOLISM PROTOCOL/ORDER SET
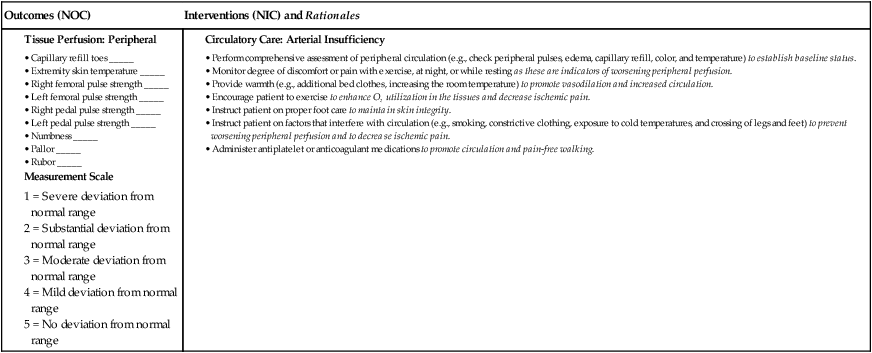
Nursing Management
Vascular Disorders