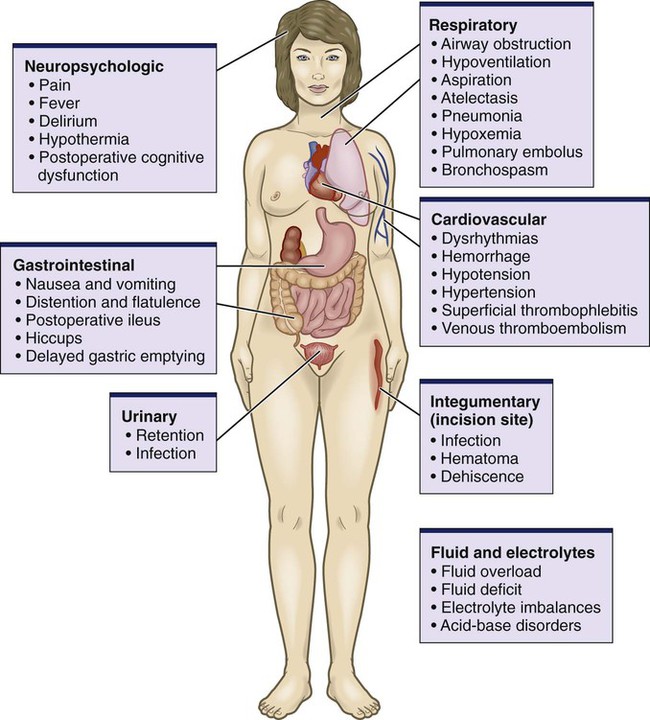
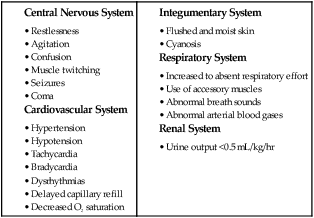
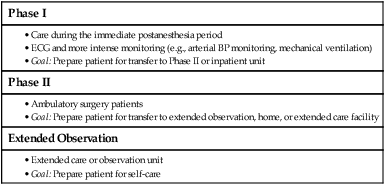
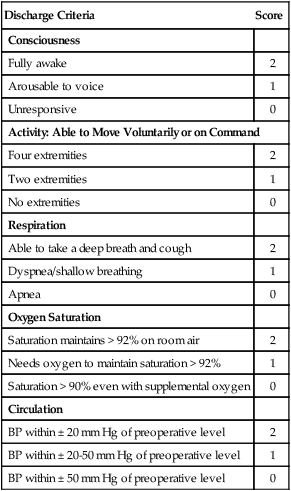
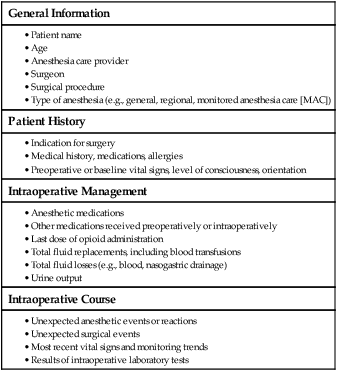
Chapter 20 1. Prioritize nursing responsibilities in admitting patients to the postanesthesia care unit (PACU). 2. Prioritize nursing responsibilities in the prevention of postoperative complications of patients in the PACU. 3. Apply data from the initial nursing assessment to the management of the patient after transfer from the PACU to the general care unit. 4. Select appropriate nursing interventions to manage potential problems during the postoperative period. 5. Differentiate discharge criteria from Phase I and Phase II postanesthesia care. The patient’s immediate recovery period is managed in a postanesthesia care unit (PACU), which is located adjacent to the operating room (OR). This location minimizes transportation of the patient immediately after surgery and provides ready access to anesthesia and OR personnel. During the three phases of postanesthesia care, different levels of care are provided depending on the patient’s needs1 (Table 20-1). TABLE 20-1 Source: American Society of PeriAnesthesia Nurses: Perianesthesia nursing standards and practice recommendations 2010-2012, Cherry Hill, NJ, 2010, The Society. eTABLE 20-1 MODIFIED ALDRETE SCORING SYSTEM Sources: Ead H: From Aldrete to PADSS: Reviewing discharge criteria after ambulatory surgery, J Perianesth Nurs 21:259, 2006; Aldrete JA: The post-anesthesia recovery score revisited, J Clin Anesth 7:89, 1995. How patients move through the phases of care in the PACU is determined by their condition. If a patient assigned to Phase I care on admission to the PACU is stable and recovering well, the patient may rapidly progress through Phase I to discharge to either Phase II care or an inpatient unit. This accelerated progress is called rapid postanesthesia care unit progression (RPP). Another accelerated system of care is fast-tracking, which involves admitting ambulatory surgery patients directly to Phase II care.1 Although both RPP and fast-tracking can potentially result in time and cost savings, the patient’s safety is the primary determining factor of where and at what level postoperative care is provided.2,3 On admission of the patient to the PACU, the ACP gives you a complete postanesthesia admission report (Table 20-2). The goal of PACU care is to identify actual and potential patient problems that may occur as a result of anesthesia and surgery and to intervene appropriately. Potential problems in the postoperative period are identified in Fig. 20-1. Table 20-3 identifies key components of a PACU assessment. TABLE 20-2 Begin the assessment with an evaluation of the patient’s airway, breathing, and circulation (ABC) status. During the initial assessment, identify signs of inadequate oxygenation and ventilation (Table 20-4). Any evidence of respiratory compromise requires prompt intervention. Pulse oximetry monitoring provides a noninvasive means of assessing oxygenation and can provide an early warning of hypoxemia.4 Transcutaneous carbon dioxide (PTCCO2) and end-tidal CO2 (PETCO2) (capnography) monitoring are used to detect respiratory depression.5–6 (Pulse oximetry, PTCCO2, and PETCO2 are discussed in Chapter 26.) In the immediate postanesthesia period the most common causes of airway compromise include obstruction, hypoxemia, and hypoventilation (Table 20-5). Patients at high risk include those who have had general anesthesia; are older; have a smoking history; have obstructive sleep apnea or lung disease; are obese; or have undergone airway, thoracic, or abdominal surgery. However, respiratory problems may occur with any patient who has been anesthetized. TABLE 20-5 POSTOPERATIVE RESPIRATORY COMPLICATIONS
Nursing Management
Postoperative Care
Postoperative Care of the Surgical Patient
Phase I
Phase II
Extended Observation
Postanesthesia Care Unit Admission
Discharge Criteria
Score
Consciousness
Fully awake
2
Arousable to voice
1
Unresponsive
0
Activity: Able to Move Voluntarily or on Command
Four extremities
2
Two extremities
1
No extremities
0
Respiration
Able to take a deep breath and cough
2
Dyspnea/shallow breathing
1
Apnea
0
Oxygen Saturation
Saturation maintains > 92% on room air
2
Needs oxygen to maintain saturation > 92%
1
Saturation > 90% even with supplemental oxygen
0
Circulation
BP within ± 20 mm Hg of preoperative level
2
BP within ± 20-50 mm Hg of preoperative level
1
BP within ± 50 mm Hg of preoperative level
0
PACU Progression.
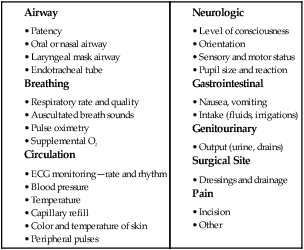
Phase I Initial Assessment.
General Information
Patient History
Intraoperative Management
Intraoperative Course
Respiratory Problems
Etiology
PACU.
Complications
Mechanisms
Manifestations
Interventions
Airway Obstruction
Tongue falling back
Muscular flaccidity associated with ↓ consciousness and muscle relaxants
Retained thick secretions
Laryngospasm
Laryngeal edema
Similar to laryngospasm
Hypoxemia
Atelectasis
Bronchial obstruction caused by retained secretions or ↓ lung volumes
Pulmonary edema
Pulmonary embolism
Thrombus dislodged from peripheral venous system and lodged in pulmonary arterial system
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

Nursing Management: Postoperative Care
Get Clinical Tree app for offline access