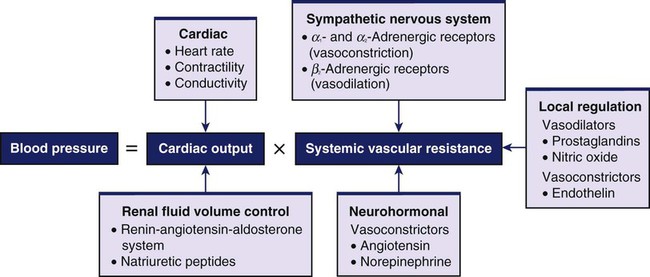
Chapter 33 1. Relate the pathophysiologic mechanisms associated with primary hypertension to the clinical manifestations and complications. 2. Select appropriate strategies for the prevention of primary hypertension. 3. Describe the collaborative care for primary hypertension, including drug therapy and lifestyle modifications. 4. Explain the collaborative care of the older adult with primary hypertension. 5. Prioritize the nursing management of the patient with primary hypertension. 6. Describe the collaborative care of a patient with hypertensive crisis. Hypertension, or high blood pressure (BP), is an important medical and public health problem. There is a direct relationship between hypertension and cardiovascular disease (CVD). As BP increases, so does the risk of myocardial infarction (MI), heart failure, stroke, and renal disease.1 This chapter discusses the nursing care and collaborative management of patients at risk for or who have hypertension. One in three adults in the United States has hypertension. Additionally, 30% of adults have prehypertension,2 and approximately 8% have undiagnosed hypertension.3 Healthy People 2020 lists the number of adults with hypertension whose BP is under control as one of the 26 high-priority, leading health indicators for the coming decade.4 The National Health and Nutrition Examination Survey (NHANES) tracks prevention, treatment, and control of hypertension. Data from NHANES show that most people 20 years of age and older with hypertension (82%) were aware that they had high BP, and 75% were being treated. However, 53% did not have their BP controlled.2 The American College of Cardiology Foundation and the American Heart Association (AHA) provide performance measures for hypertension management that address not only treatment, but also control of BP to target goals. To achieve the measures, patients with hypertension must have a BP of less than 140/90 mm Hg or, if their BP is higher, have at least two antihypertensive medications prescribed.5 National guidelines are designed to apply to all racial and ethnic groups. However, certain groups have a higher incidence of risk factors2,6–8 (see boxes on Cultural & Ethnic Health Disparities and Gender Differences). eTABLE 33-2 DRUG THERAPY Blood pressure (BP) is the force exerted by the blood against the walls of the blood vessel. It must be adequate to maintain tissue perfusion during activity and rest. The maintenance of normal BP and tissue perfusion requires the integration of both systemic factors and local peripheral vascular effects. BP is primarily a function of cardiac output (CO) and systemic vascular resistance (Fig. 33-1). The neurotransmitter norepinephrine (NE) is released from SNS nerve endings. NE activates receptors located in the sinoatrial node, myocardium, and vascular smooth muscle. The response to NE depends on the type of receptors present. SNS receptors are classified as α1, α2, β1, and β2 (Table 33-1). The smooth muscle of the blood vessels has α-adrenergic and β2-adrenergic receptors. α-Adrenergic receptors located in the peripheral vasculature cause vasoconstriction when stimulated by NE. β1-Adrenergic receptors in the heart respond to NE and epinephrine with increased HR (chronotropic), increased force of contraction (inotropic), and increased speed of conduction (dromotropic). β2-Adrenergic receptors are activated primarily by epinephrine released from the adrenal medulla and cause vasodilation (see Fig. 33-1). TABLE 33-1 SYMPATHETIC NERVOUS SYSTEM RECEPTORS AFFECTING BLOOD PRESSURE The vascular endothelium is a single-cell layer that lines the blood vessels. It produces several vasoactive substances and growth factors. Nitric oxide and prostacyclin help maintain low arterial tone, inhibit growth of the smooth muscle layer, and inhibit platelet aggregation. Endothelin (ET) is an extremely potent vasoconstrictor. It also causes adhesion and aggregation of neutrophils and stimulates smooth muscle growth (see Fig. 33-1). The kidneys contribute to BP regulation by controlling sodium excretion and extracellular fluid (ECF) volume (see Chapter 45). Sodium retention results in water retention, which causes an increased ECF volume. This increases the venous return to the heart and the stroke volume. Together, these increase CO and BP. The renin-angiotensin-aldosterone system (RAAS) also plays an important role in BP regulation (see Fig. 33-1). The juxtaglomerular apparatus in the kidney secretes renin in response to SNS stimulation, decreased blood flow through the kidneys, or decreased serum sodium concentration. Renin is an enzyme that converts angiotensinogen to angiotensin I. Angiotensin-converting enzyme (ACE) converts angiotensin I into angiotensin II (A-II). A-II increases BP by two different mechanisms (see Fig. 45-4). First, A-II is a potent vasoconstrictor and increases SVR. This results in an immediate increase in BP. Second, over a period of hours or days, A-II increases BP indirectly by stimulating the adrenal cortex to secrete aldosterone (discussed below). Prostaglandins (PGE2 and PGI2) secreted by the renal medulla have a vasodilator effect on the systemic circulation. This results in decreased SVR and lowering of BP. (Prostaglandins are discussed in Chapter 12.) The natriuretic peptides (atrial natriuretic peptide [ANP] and b-type natriuretic peptide [BNP]) are secreted by heart cells. They antagonize the effects of antidiuretic hormone (ADH) and aldosterone. This results in natriuresis (excretion of sodium in urine) and diuresis, resulting in reduced blood volume and BP. Hypertension is defined as a persistent systolic BP (SBP) of 140 mm Hg or more, diastolic BP (DBP) of 90 mm Hg or more, or current use of antihypertensive medication.1 Prehypertension is defined as SBP of 120 to 139 mm Hg or DBP of 80 to 89 mm Hg. Isolated systolic hypertension (ISH) is defined as an average SBP of 140 mm Hg or more, coupled with an average DBP of less than 90 mm Hg.9 SBP increases with aging. DBP rises until approximately age 55 and then declines. Control of ISH decreases the incidence of stroke, heart failure, and death. The classification of BP is based on the average of two or more properly measured BP readings on two or more office visits. Table 33-2 presents the BP classification for people 18 years of age and older. TABLE 33-2 CLASSIFICATION OF HYPERTENSION DBP, Diastolic blood pressure; SBP, systolic blood pressure. From the National Heart, Lung, and Blood Institute: Seventh report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7), NIH Publication No. 04-5230, Bethesda, Md, 2004, The Institute. Retrieved from www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf. Hypertension can be classified as either primary or secondary. Secondary hypertension is elevated BP with a specific cause that often can be identified and corrected (Table 33-3). This type of hypertension accounts for 5% to 10% of hypertension in adults. Secondary hypertension should be suspected in people who suddenly develop high BP, especially if it is severe. Clinical findings that suggest secondary hypertension relate to the underlying cause. For example, an abdominal bruit heard over the renal arteries may indicate renal disease. Treatment of secondary hypertension is aimed at removing or treating the underlying cause. Secondary hypertension is a contributing factor to hypertensive crisis (discussed later in this chapter). TABLE 33-3 CAUSES OF SECONDARY HYPERTENSION* BP rises with any increase in CO or SVR. Increased CO is sometimes found in the person with prehypertension. Later in the course of hypertension, the SVR rises and the CO returns to normal. The hemodynamic hallmark of hypertension is persistently increased SVR. This persistent elevation in SVR may occur in various ways. Table 33-4 presents factors that relate to the development of primary hypertension or contribute to its consequences. Abnormalities of any of the mechanisms involved in the maintenance of normal BP can result in hypertension (see Fig. 33-1). TABLE 33-4 RISK FACTORS FOR PRIMARY HYPERTENSION DBP, Diastolic blood pressure; SBP, systolic blood pressure. Different sets of genes may regulate BP at different times throughout the life span.2 Genetic abnormalities associated with a rare form of hypertension characterized by excess levels of potassium have been identified. To date, the known contribution of genetic factors to BP in the general population remains very small.1 In clinical practice, there is not an easy or simple test to identify individuals whose BP will rise with even a small increase in salt intake (salt sensitive) versus those who can ingest large amounts of sodium without much change in BP (salt resistant). In general, the effect of sodium on BP is greater in African Americans and in middle-aged and older adults.10 High plasma renin activity (PRA) results in the increased conversion of angiotensinogen to angiotensin I (see Fig. 45-4). This alteration in the RAAS may contribute to the development of hypertension. Any rise in BP inhibits the release of renin from the renal juxtaglomerular cells. Based on this feedback loop, low levels of PRA would be expected in patients with primary hypertension. However, only about 30% have low PRA, 50% have normal levels, and 20% have high PRA. These normal or high PRA levels may be related to excess renin secretion from ischemic nephrons. Hypertension is often called the “silent killer” because it is frequently asymptomatic until it becomes severe and target organ disease occurs. A patient with severe hypertension may experience a variety of symptoms secondary to the effects on blood vessels in the various organs and tissues or to the increased workload of the heart. These secondary symptoms include fatigue, dizziness, palpitations, angina, and dyspnea. In the past, symptoms of hypertension were thought to include headache and nosebleeds. Unless BP is very high, these symptoms are no more frequent in people with hypertension than in the general population. However, patients with hypertensive crisis (discussed later in the chapter) may experience severe headaches, dyspnea, anxiety, and nosebleeds.11 The most common complications of hypertension are target organ diseases occurring in the heart (hypertensive heart disease), brain (cerebrovascular disease), peripheral vessels (peripheral vascular disease), kidneys (nephrosclerosis), and eyes (retinal damage) (Table 33-5). TABLE 33-5 MANIFESTATIONS OF TARGET ORGAN DISEASE • One or more major pulses in the extremities (except for dorsalis pedis) reduced or absent • Abdominal or carotid bruits or thrills
Nursing Management
Hypertension
Hypertension (expanded)
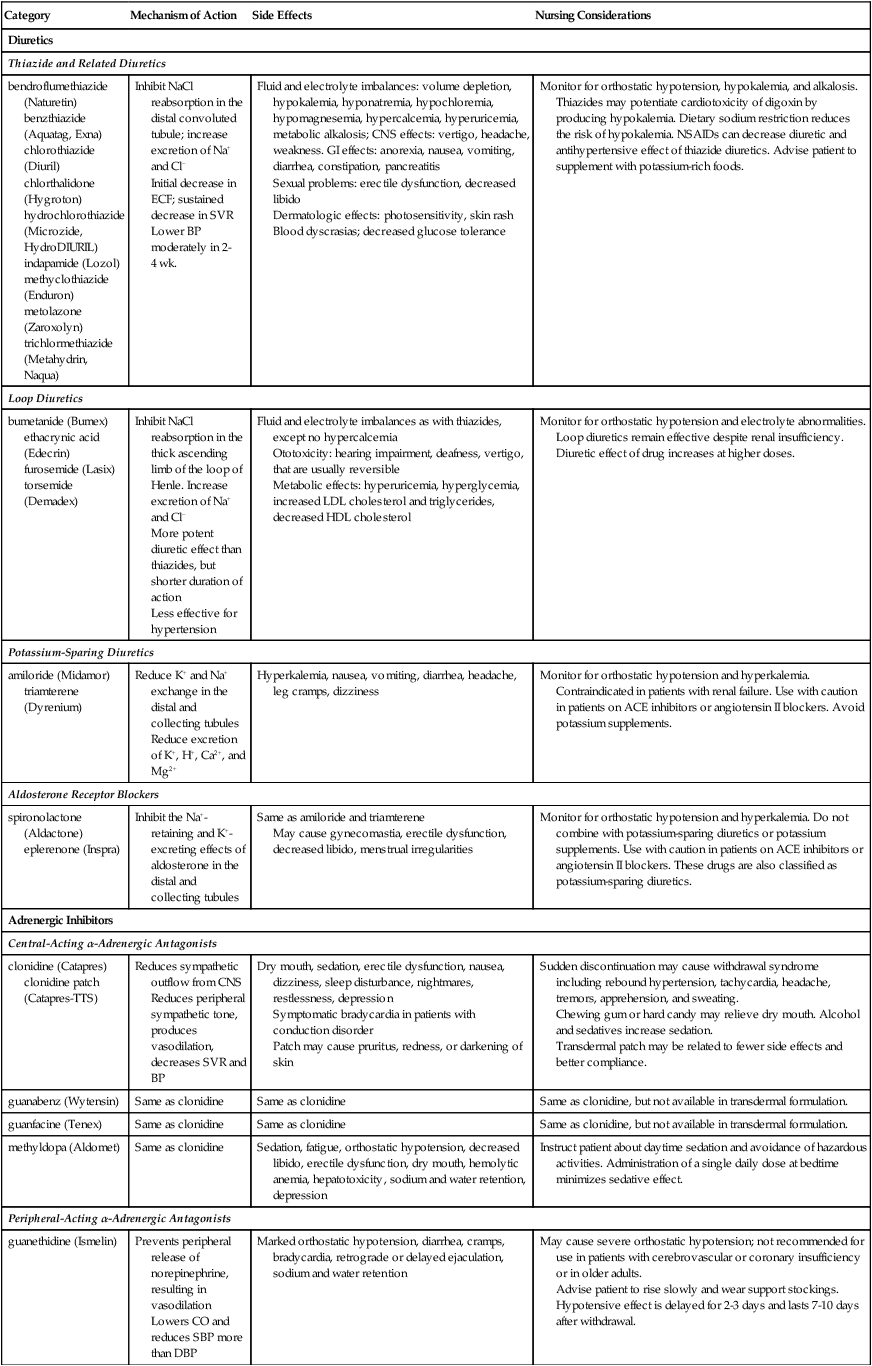
Category
Mechanism of Action
Side Effects
Nursing Considerations
Diuretics
Thiazide and Related Diuretics
bendroflumethiazide (Naturetin)
benzthiazide (Aquatag, Exna)
chlorothiazide (Diuril)
chlorthalidone (Hygroton)
hydrochlorothiazide (Microzide, HydroDIURIL)
indapamide (Lozol)
methyclothiazide (Enduron)
metolazone (Zaroxolyn)
trichlormethiazide (Metahydrin, Naqua)
Inhibit NaCl reabsorption in the distal convoluted tubule; increase excretion of Na+ and Cl−
Initial decrease in ECF; sustained decrease in SVR
Lower BP moderately in 2-4 wk.
Fluid and electrolyte imbalances: volume depletion, hypokalemia, hyponatremia, hypochloremia, hypomagnesemia, hypercalcemia, hyperuricemia, metabolic alkalosis; CNS effects: vertigo, headache, weakness. GI effects: anorexia, nausea, vomiting, diarrhea, constipation, pancreatitis
Sexual problems: erectile dysfunction, decreased libido
Dermatologic effects: photosensitivity, skin rash
Blood dyscrasias; decreased glucose tolerance
Monitor for orthostatic hypotension, hypokalemia, and alkalosis. Thiazides may potentiate cardiotoxicity of digoxin by producing hypokalemia. Dietary sodium restriction reduces the risk of hypokalemia. NSAIDs can decrease diuretic and antihypertensive effect of thiazide diuretics. Advise patient to supplement with potassium-rich foods.
Loop Diuretics
bumetanide (Bumex)
ethacrynic acid (Edecrin)
furosemide (Lasix)
torsemide (Demadex)
Inhibit NaCl reabsorption in the thick ascending limb of the loop of Henle. Increase excretion of Na+ and Cl−
More potent diuretic effect than thiazides, but shorter duration of action
Less effective for hypertension
Fluid and electrolyte imbalances as with thiazides, except no hypercalcemia
Ototoxicity: hearing impairment, deafness, vertigo, that are usually reversible
Metabolic effects: hyperuricemia, hyperglycemia, increased LDL cholesterol and triglycerides, decreased HDL cholesterol
Monitor for orthostatic hypotension and electrolyte abnormalities.
Loop diuretics remain effective despite renal insufficiency. Diuretic effect of drug increases at higher doses.
Potassium-Sparing Diuretics
amiloride (Midamor)
triamterene (Dyrenium)
Reduce K+ and Na+ exchange in the distal and collecting tubules
Reduce excretion of K+, H+, Ca2+, and Mg2+
Hyperkalemia, nausea, vomiting, diarrhea, headache, leg cramps, dizziness
Monitor for orthostatic hypotension and hyperkalemia.
Contraindicated in patients with renal failure. Use with caution in patients on ACE inhibitors or angiotensin II blockers. Avoid potassium supplements.
Aldosterone Receptor Blockers
spironolactone (Aldactone)
eplerenone (Inspra)
Inhibit the Na+-retaining and K+-excreting effects of aldosterone in the distal and collecting tubules
Same as amiloride and triamterene
May cause gynecomastia, erectile dysfunction, decreased libido, menstrual irregularities
Monitor for orthostatic hypotension and hyperkalemia. Do not combine with potassium-sparing diuretics or potassium supplements. Use with caution in patients on ACE inhibitors or angiotensin II blockers. These drugs are also classified as potassium-sparing diuretics.
Adrenergic Inhibitors
Central-Acting α-Adrenergic Antagonists
clonidine (Catapres)
clonidine patch (Catapres-TTS)
Reduces sympathetic outflow from CNS
Reduces peripheral sympathetic tone, produces vasodilation, decreases SVR and BP
Dry mouth, sedation, erectile dysfunction, nausea, dizziness, sleep disturbance, nightmares, restlessness, depression
Symptomatic bradycardia in patients with conduction disorder
Patch may cause pruritus, redness, or darkening of skin
Sudden discontinuation may cause withdrawal syndrome including rebound hypertension, tachycardia, headache, tremors, apprehension, and sweating.
Chewing gum or hard candy may relieve dry mouth. Alcohol and sedatives increase sedation.
Transdermal patch may be related to fewer side effects and better compliance.
guanabenz (Wytensin)
Same as clonidine
Same as clonidine
Same as clonidine, but not available in transdermal formulation.
guanfacine (Tenex)
Same as clonidine
Same as clonidine
Same as clonidine, but not available in transdermal formulation.
methyldopa (Aldomet)
Same as clonidine
Sedation, fatigue, orthostatic hypotension, decreased libido, erectile dysfunction, dry mouth, hemolytic anemia, hepatotoxicity, sodium and water retention, depression
Instruct patient about daytime sedation and avoidance of hazardous activities. Administration of a single daily dose at bedtime minimizes sedative effect.
Peripheral-Acting α-Adrenergic Antagonists
guanethidine (Ismelin)
Prevents peripheral release of norepinephrine, resulting in vasodilation
Lowers CO and reduces SBP more than DBP
Marked orthostatic hypotension, diarrhea, cramps, bradycardia, retrograde or delayed ejaculation, sodium and water retention
May cause severe orthostatic hypotension; not recommended for use in patients with cerebrovascular or coronary insufficiency or in older adults.
Advise patient to rise slowly and wear support stockings.
Hypotensive effect is delayed for 2-3 days and lasts 7-10 days after withdrawal.
guanadrel sulfate (Hylorel)
Same as guanethidine
Similar to guanethidine but less severe
Must be given twice daily.
reserpine (Serpasil)
Depletes central and peripheral stores of norepinephrine
Results in peripheral vasodilation (decreases SVR and BP)
Sedation and inability to concentrate, depression, nasal stuffiness
Contraindicated in patients with history of depression. Monitor mood and mental status regularly. Advise patient to avoid barbiturates, alcohol, and opioids.
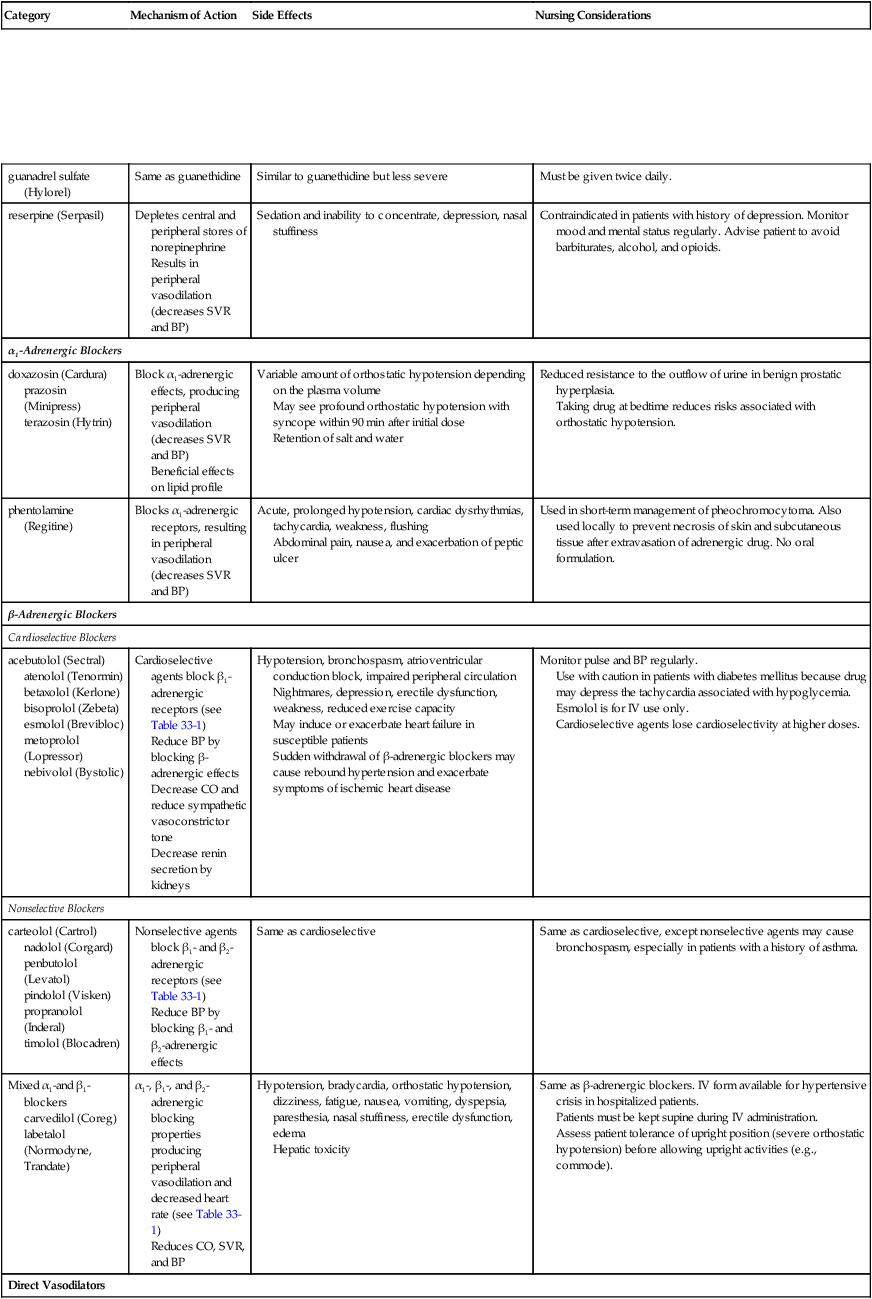
α1-Adrenergic Blockers
doxazosin (Cardura)
prazosin (Minipress)
terazosin (Hytrin)
Block α1-adrenergic effects, producing peripheral vasodilation (decreases SVR and BP)
Beneficial effects on lipid profile
Variable amount of orthostatic hypotension depending on the plasma volume
May see profound orthostatic hypotension with syncope within 90 min after initial dose
Retention of salt and water
Reduced resistance to the outflow of urine in benign prostatic hyperplasia.
Taking drug at bedtime reduces risks associated with orthostatic hypotension.
phentolamine (Regitine)
Blocks α1-adrenergic receptors, resulting in peripheral vasodilation (decreases SVR and BP)
Acute, prolonged hypotension, cardiac dysrhythmias, tachycardia, weakness, flushing
Abdominal pain, nausea, and exacerbation of peptic ulcer
Used in short-term management of pheochromocytoma. Also used locally to prevent necrosis of skin and subcutaneous tissue after extravasation of adrenergic drug. No oral formulation.
β-Adrenergic Blockers
Cardioselective Blockers
acebutolol (Sectral)
atenolol (Tenormin)
betaxolol (Kerlone)
bisoprolol (Zebeta)
esmolol (Brevibloc)
metoprolol (Lopressor)
nebivolol (Bystolic)
Cardioselective agents block β1-adrenergic receptors (see Table 33-1)
Reduce BP by blocking β-adrenergic effects
Decrease CO and reduce sympathetic vasoconstrictor tone
Decrease renin secretion by kidneys
Hypotension, bronchospasm, atrioventricular conduction block, impaired peripheral circulation
Nightmares, depression, erectile dysfunction, weakness, reduced exercise capacity
May induce or exacerbate heart failure in susceptible patients
Sudden withdrawal of β-adrenergic blockers may cause rebound hypertension and exacerbate symptoms of ischemic heart disease
Monitor pulse and BP regularly.
Use with caution in patients with diabetes mellitus because drug may depress the tachycardia associated with hypoglycemia.
Esmolol is for IV use only.
Cardioselective agents lose cardioselectivity at higher doses.
Nonselective Blockers
carteolol (Cartrol)
nadolol (Corgard)
penbutolol (Levatol)
pindolol (Visken)
propranolol (Inderal)
timolol (Blocadren)
Nonselective agents block β1– and β2-adrenergic receptors (see Table 33-1)
Reduce BP by blocking β1– and β2-adrenergic effects
Same as cardioselective
Same as cardioselective, except nonselective agents may cause bronchospasm, especially in patients with a history of asthma.
Mixed α1-and β1-blockers
carvedilol (Coreg)
labetalol (Normodyne, Trandate)
α1-, β1-, and β2-adrenergic blocking properties producing peripheral vasodilation and decreased heart rate (see Table 33-1)
Reduces CO, SVR, and BP
Hypotension, bradycardia, orthostatic hypotension, dizziness, fatigue, nausea, vomiting, dyspepsia, paresthesia, nasal stuffiness, erectile dysfunction, edema
Hepatic toxicity
Same as β-adrenergic blockers. IV form available for hypertensive crisis in hospitalized patients.
Patients must be kept supine during IV administration.
Assess patient tolerance of upright position (severe orthostatic hypotension) before allowing upright activities (e.g., commode).
Direct Vasodilators
fenoldopam (Corlopam)
Activates dopamine receptors, resulting in systemic and renal vasodilation
Tachycardia, angina, headache, nausea, flushing
IV use only for hypertensive crisis in hospitalized patients.
Use cautiously in patients with glaucoma.
Patient should remain supine for 1 hr after administration.
hydralazine (Apresoline)
Reduces SVR and BP by direct arterial vasodilation
Headache, nausea, flushing, palpitation, tachycardia, dizziness, and angina
Hemolytic anemia, vasculitis, and rapidly progressive glomerulonephritis
IV use for hypertensive crisis in hospitalized patients.
Twice-daily oral dosage.
Not used as monotherapy because of side effects.
Contraindicated in patients with coronary artery disease.
minoxidil (Loniten)
Reduces SVR and BP by direct arterial vasodilation
Reflex tachycardia, marked sodium and fluid retention (may require loop diuretics for control), and hirsutism
May cause ECG changes (flattened and inverted T waves) not related to ischemia
Reserved for treatment of severe hypertension associated with renal failure and resistant to other therapy. Once- or twice-daily dosage.
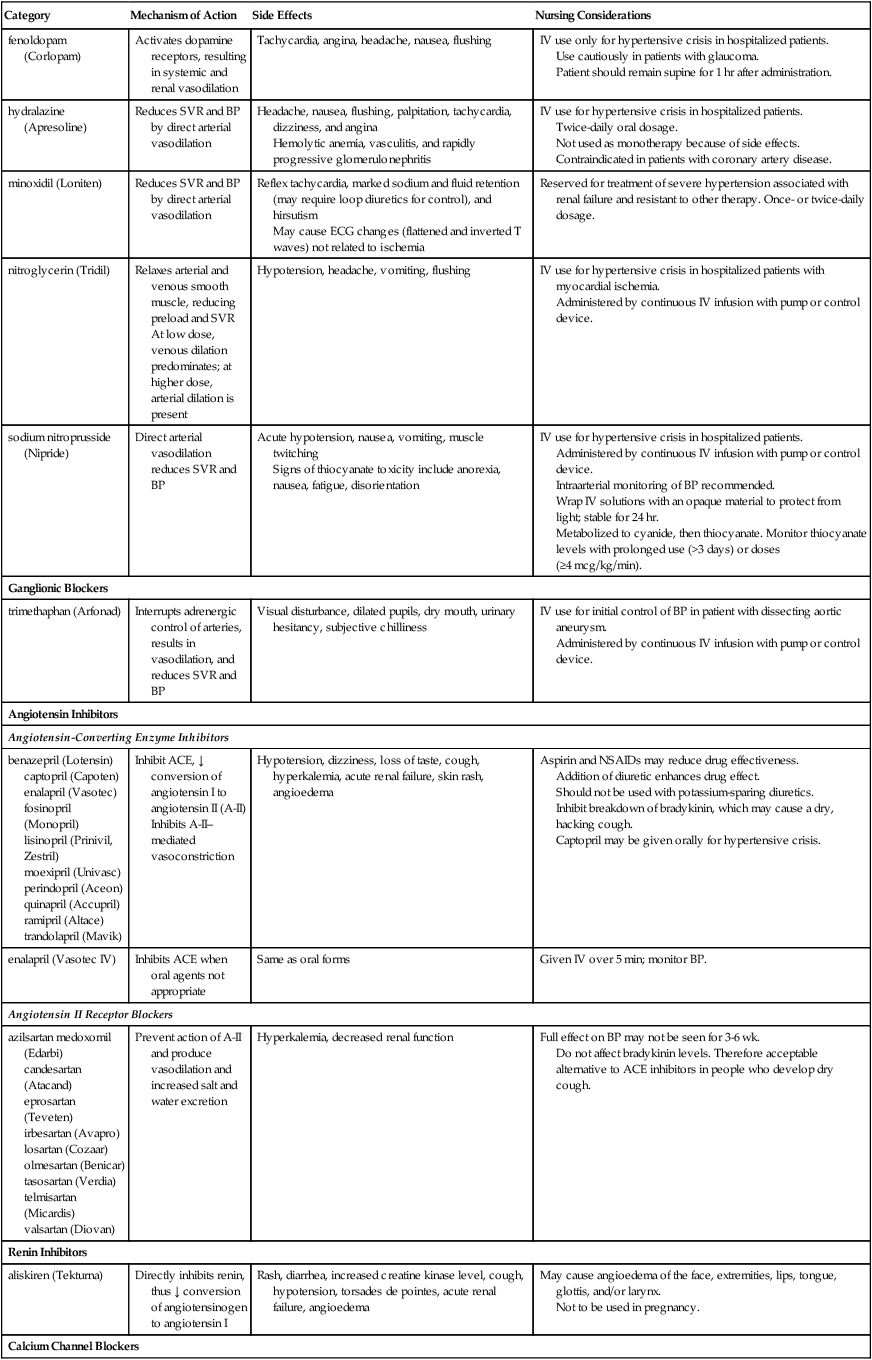
nitroglycerin (Tridil)
Relaxes arterial and venous smooth muscle, reducing preload and SVR
At low dose, venous dilation predominates; at higher dose, arterial dilation is present
Hypotension, headache, vomiting, flushing
IV use for hypertensive crisis in hospitalized patients with myocardial ischemia.
Administered by continuous IV infusion with pump or control device.
sodium nitroprusside (Nipride)
Direct arterial vasodilation reduces SVR and BP
Acute hypotension, nausea, vomiting, muscle twitching
Signs of thiocyanate toxicity include anorexia, nausea, fatigue, disorientation
IV use for hypertensive crisis in hospitalized patients.
Administered by continuous IV infusion with pump or control device.
Intraarterial monitoring of BP recommended.
Wrap IV solutions with an opaque material to protect from light; stable for 24 hr.
Metabolized to cyanide, then thiocyanate. Monitor thiocyanate levels with prolonged use (>3 days) or doses (≥4 mcg/kg/min).
Ganglionic Blockers
trimethaphan (Arfonad)
Interrupts adrenergic control of arteries, results in vasodilation, and reduces SVR and BP
Visual disturbance, dilated pupils, dry mouth, urinary hesitancy, subjective chilliness
IV use for initial control of BP in patient with dissecting aortic aneurysm.
Administered by continuous IV infusion with pump or control device.
Angiotensin Inhibitors
Angiotensin-Converting Enzyme Inhibitors
benazepril (Lotensin)
captopril (Capoten)
enalapril (Vasotec)
fosinopril (Monopril)
lisinopril (Prinivil, Zestril)
moexipril (Univasc)
perindopril (Aceon)
quinapril (Accupril)
ramipril (Altace)
trandolapril (Mavik)
Inhibit ACE, ↓ conversion of angiotensin I to angiotensin II (A-II)
Inhibits A-II–mediated vasoconstriction
Hypotension, dizziness, loss of taste, cough, hyperkalemia, acute renal failure, skin rash, angioedema
Aspirin and NSAIDs may reduce drug effectiveness.
Addition of diuretic enhances drug effect.
Should not be used with potassium-sparing diuretics.
Inhibit breakdown of bradykinin, which may cause a dry, hacking cough.
Captopril may be given orally for hypertensive crisis.
enalapril (Vasotec IV)
Inhibits ACE when oral agents not appropriate
Same as oral forms
Given IV over 5 min; monitor BP.
Angiotensin II Receptor Blockers
azilsartan medoxomil (Edarbi)
candesartan (Atacand)
eprosartan (Teveten)
irbesartan (Avapro)
losartan (Cozaar)
olmesartan (Benicar)
tasosartan (Verdia)
telmisartan (Micardis)
valsartan (Diovan)
Prevent action of A-II and produce vasodilation and increased salt and water excretion
Hyperkalemia, decreased renal function
Full effect on BP may not be seen for 3-6 wk.
Do not affect bradykinin levels. Therefore acceptable alternative to ACE inhibitors in people who develop dry cough.
Renin Inhibitors
aliskiren (Tekturna)
Directly inhibits renin, thus ↓ conversion of angiotensinogen to angiotensin I
Rash, diarrhea, increased creatine kinase level, cough, hypotension, torsades de pointes, acute renal failure, angioedema
May cause angioedema of the face, extremities, lips, tongue, glottis, and/or larynx.
Not to be used in pregnancy.
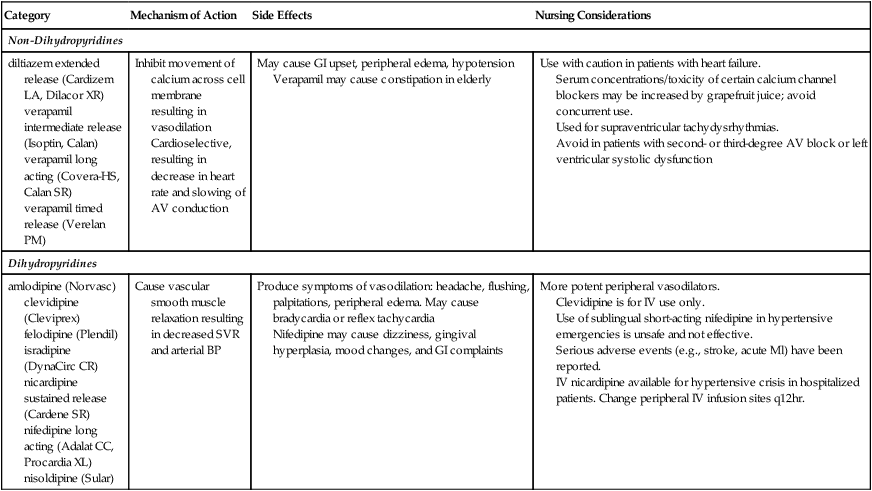
Calcium Channel Blockers
Non-Dihydropyridines
diltiazem extended release (Cardizem LA, Dilacor XR)
verapamil intermediate release (Isoptin, Calan)
verapamil long acting (Covera-HS, Calan SR)
verapamil timed release (Verelan PM)
Inhibit movement of calcium across cell membrane resulting in vasodilation
Cardioselective, resulting in decrease in heart rate and slowing of AV conduction
May cause GI upset, peripheral edema, hypotension
Verapamil may cause constipation in elderly
Use with caution in patients with heart failure.
Serum concentrations/toxicity of certain calcium channel blockers may be increased by grapefruit juice; avoid concurrent use.
Used for supraventricular tachydysrhythmias.
Avoid in patients with second- or third-degree AV block or left ventricular systolic dysfunction
Dihydropyridines
amlodipine (Norvasc)
clevidipine (Cleviprex)
felodipine (Plendil)
isradipine (DynaCirc CR)
nicardipine sustained release (Cardene SR)
nifedipine long acting (Adalat CC, Procardia XL)
nisoldipine (Sular)
Cause vascular smooth muscle relaxation resulting in decreased SVR and arterial BP
Produce symptoms of vasodilation: headache, flushing, palpitations, peripheral edema. May cause bradycardia or reflex tachycardia
Nifedipine may cause dizziness, gingival hyperplasia, mood changes, and GI complaints
More potent peripheral vasodilators.
Clevidipine is for IV use only.
Use of sublingual short-acting nifedipine in hypertensive emergencies is unsafe and not effective.
Serious adverse events (e.g., stroke, acute Ml) have been reported.
IV nicardipine available for hypertensive crisis in hospitalized patients. Change peripheral IV infusion sites q12hr.
Normal Regulation of Blood Pressure
Sympathetic Nervous System
Receptor
Location
Response When Activated
α1
Vascular smooth muscle
Vasoconstriction
Heart
Increased contractility (positive inotropic effect)
α2
Presynaptic nerve terminals
Inhibition of norepinephrine release
Vascular smooth muscle
Vasoconstriction
β1
Heart
Increased contractility (positive inotropic effect)
Increased heart rate (positive chronotropic effect)
Increased conduction (positive dromotropic effect)
Juxtaglomerular cells of the kidney
Increased renin secretion
β2
Smooth muscle of blood vessels in heart (e.g., coronary arteries), lungs (e.g., bronchi), and skeletal muscle
Vasodilation
Dopamine receptors
Primarily renal blood vessels
Vasodilation
Vascular Endothelium
Renal System
Hypertension
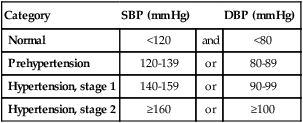
Classification of Hypertension
Category
SBP (mm Hg)
DBP (mm Hg)
Normal
<120
and
<80
Prehypertension
120-139
or
80-89
Hypertension, stage 1
140-159
or
90-99
Hypertension, stage 2
≥160
or
≥100
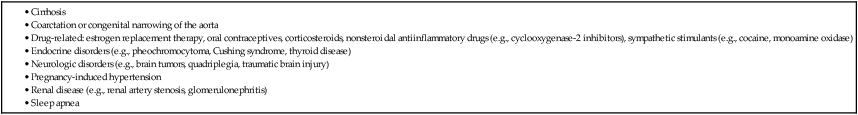
Etiology
Secondary Hypertension.
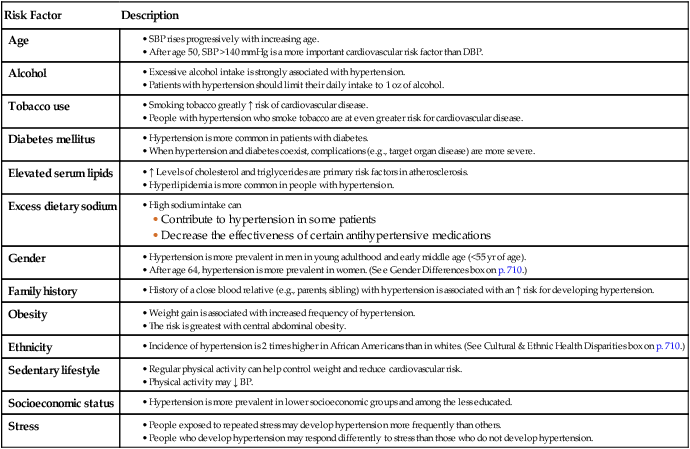
Pathophysiology of Primary Hypertension
Risk Factor
Description
Age
Alcohol
Tobacco use
Diabetes mellitus
Elevated serum lipids
Excess dietary sodium
Gender
Family history
Obesity
Ethnicity
Sedentary lifestyle
Socioeconomic status
Stress
![]() Genetic Link
Genetic Link
Water and Sodium Retention.
Altered Renin-Angiotensin-Aldosterone Mechanism.
Clinical Manifestations
Complications
Organ
Manifestations
Cardiac
Cerebrovascular
Peripheral vascular
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

Nursing Management: Hypertension
Get Clinical Tree app for offline access