1. Explain the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with an imbalance of hormones produced by the anterior pituitary gland. 2. Describe the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with an imbalance of hormones produced by the posterior pituitary gland. 3. Explain the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with thyroid dysfunction. 4. Describe the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with an imbalance of the hormone produced by the parathyroid glands. 5. Identify the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with an imbalance of hormones produced by the adrenal cortex. 6. Describe the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with an excess of hormones produced by the adrenal medulla. 7. List the side effects of corticosteroid therapy. 8. Describe common nursing assessments, interventions, rationales, and expected outcomes related to patient teaching for management of chronic endocrine problems.
Nursing Management
Endocrine Problems
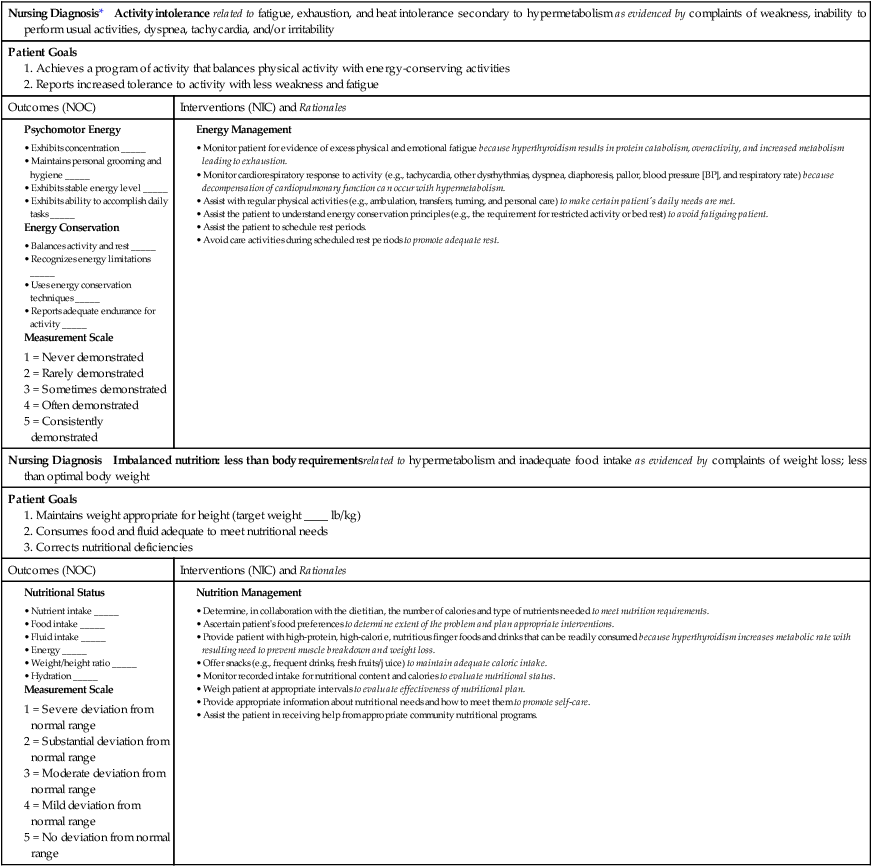
![]() eNursing Care Plan 50-1 Patient With Hyperthyroidism
eNursing Care Plan 50-1 Patient With Hyperthyroidism
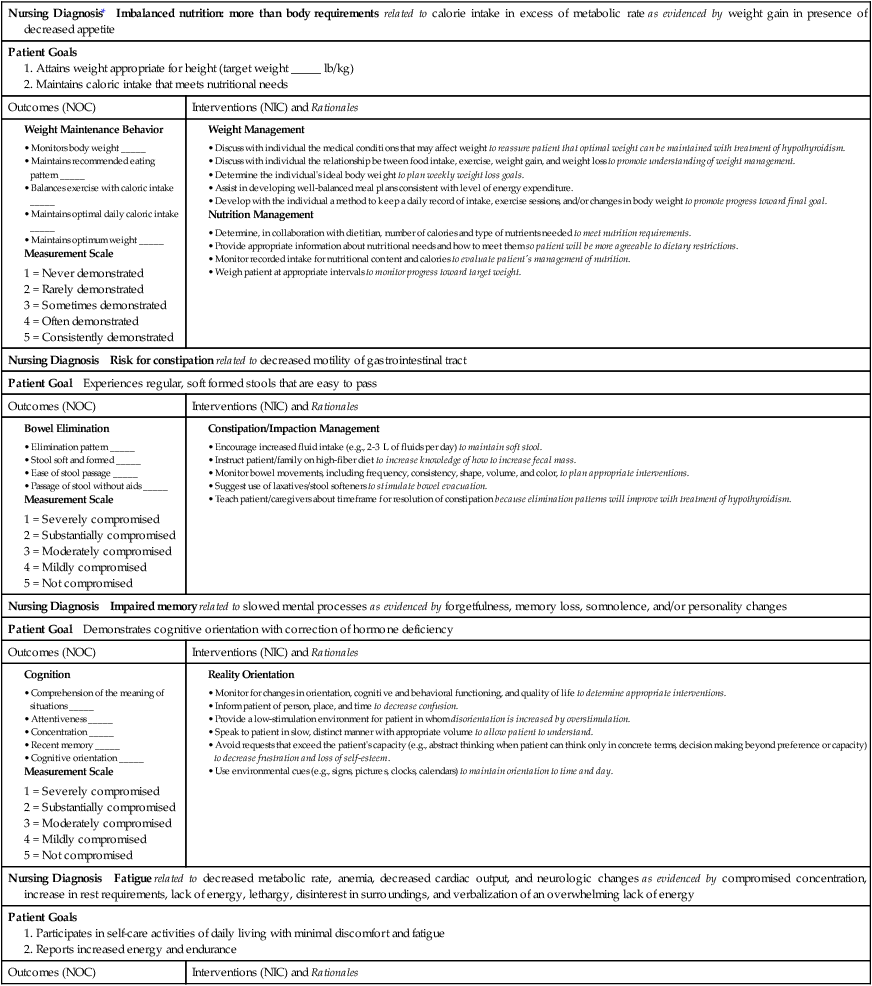
![]() eNursing Care Plan 50-2 Patient With Hypothyroidism
eNursing Care Plan 50-2 Patient With Hypothyroidism
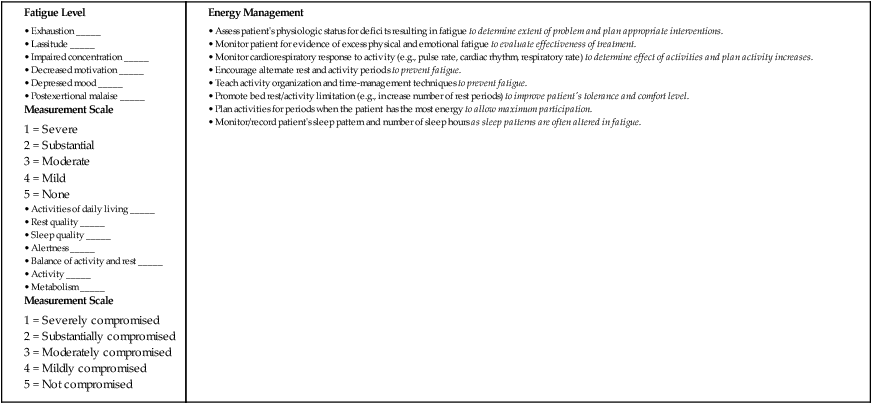
![]() eNursing Care Plan 50-3 Patient With Cushing Syndrome
eNursing Care Plan 50-3 Patient With Cushing Syndrome
Nursing Management: Endocrine Problems
1. Explain the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with an imbalance of hormones produced by the anterior pituitary gland. 2. Describe the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with an imbalance of hormones produced by the posterior pituitary gland. 3. Explain the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with thyroid dysfunction. 4. Describe the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with an imbalance of the hormone produced by the parathyroid glands. 5. Identify the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with an imbalance of hormones produced by the adrenal cortex. 6. Describe the pathophysiology, clinical manifestations, collaborative care, and nursing management of the patient with an excess of hormones produced by the adrenal medulla. 7. List the side effects of corticosteroid therapy. 8. Describe common nursing assessments, interventions, rationales, and expected outcomes related to patient teaching for management of chronic endocrine problems.
Nursing Management
Endocrine Problems



