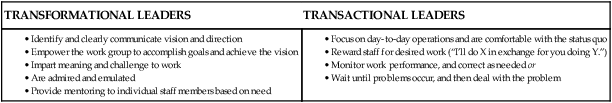
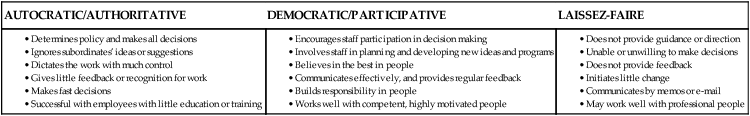
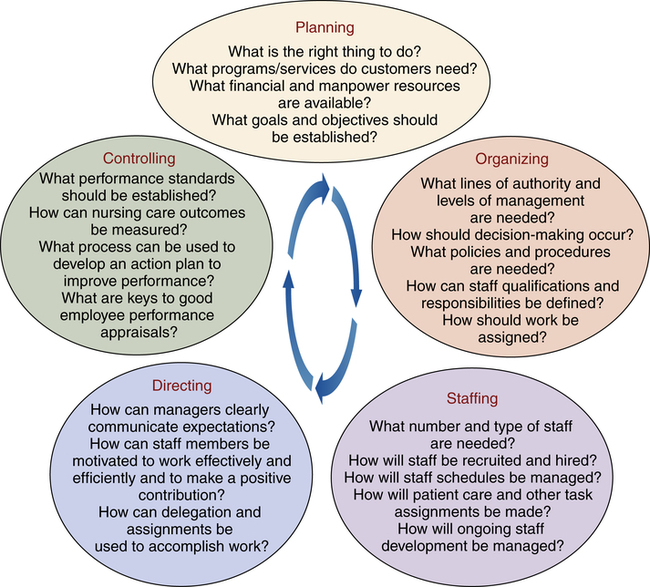
Barbara Cherry, DNSc, MBA, RN, NEA-BC After studying this chapter, the reader will be able to: 1. Relate leadership and management theory to nursing leadership and management activities. 2. Differentiate among the five functions of management and essential activities related to each function. 3. Integrate principles of patient-centered care and customer service in professional nursing practice. 4. Implement effective team-building skills as an essential component of nursing practice. 5. Implement the nursing process as a method of problem solving and planning. 6. Apply principles and strategies of change theory in the management role. 7. Discuss implications of leadership and management challenges of the twenty-first century. The legitimate right to direct others given to a person by the employer through an authorized position, such as manager or administrator. People in need of services from an organization who are not employed by the organization, including patients, family members, physicians, students, payers, discharge planners, and other groups that are a source of patient referrals. Any business, company, institution, or facility (e.g., hospital, home health agency, ambulatory care clinic, health insurance company, nursing home) engaged in providing health care services or products. People who are employed by the organization to provide services to various groups and individuals across the organization (e.g., nurses and other patient care staff, administrators, social workers, dietitians, therapists, housekeeping staff, and clerical support staff). The act of guiding or influencing people to achieve desired outcomes; occurs any time a person attempts to influence the beliefs, opinions, or behaviors of an individual or group (Hersey and Blanchard, 1988). Coordination of resources, such as time, people, and supplies, to achieve outcomes; involves problem-solving and decision-making processes. A visual picture of the organization that identifies lines of communication and authority. The amount of output or work produced (e.g., home visits made) by a specific amount of input or resources (e.g., nursing hours worked). Personnel, time, and supplies needed to accomplish the goals of the organization. Additional resources are available online at: http://evolve.elsevier.com/Cherry/ VIGNETTE The nurse manager begins the orientation program with a discussion about the mission of the organization and the RN’s responsibility to ensure that quality patient care is provided in a safe and cost-effective manner. As Nancy progresses through the orientation program, her confidence quickly fades. She becomes overwhelmed as she listens to a description of her new responsibilities as an RN. The RN’s duties involve much more than the expected physical assessment, identifying nursing diagnoses, and developing and implementing care plans. Some of Nancy’s many new responsibilities as a staff RN are to do the following: Supervise patient care technicians, and manage assignments and supply use for a group of patients. Meet with the interprofessional team including the social worker, dietitian, nephrologist, nurse manager, and the patient and family to develop the patient’s care plan, and then follow up to coordinate and implement the plan. Perform chart audits to review nursing documentation, identify problems, develop recommendations, and report to the quality management committee. Questions to Consider While Reading This Chapter 1. What leadership and management skills will assist Nancy as she begins her new role as a staff RN responsible for supervising a group of patient care technicians, managing assignments and supply use, and serving on a task force to implement a new training program? 3. What type of team-building skills will help Nancy as she learns to work with the interprofessional team and coordinate the patient’s plan of care with a diverse group of health professionals? During nursing school, students are often more concerned with developing clinical knowledge and skills and are less concerned with management and leadership skills. However, immediately after graduation the new nurse is placed in many situations that require leadership and management skills—managing a group of assigned patients, serving on a task force or committee, acting as team leader or charge nurse, or supervising unlicensed assistive personnel and licensed vocational or practical nurses. In addition to providing safe, evidence-based, high-quality clinical care, the challenges for RNs today are to manage nursing units that are constantly admitting and discharging higher-acuity patients, motivate and coordinate a variety of diverse health professionals and nonprofessionals, embrace change to develop work environments that are safer and more conducive to professional nursing practice, and manage limited resources and shrinking budgets. • Make good clinical decisions based on safety, quality, cost, legal, and ethical aspects of care. • Promote evidence-based practice (see Chapter 6). • Promote patient safety and quality improvement in the work environment. • Coordinate patient care activities for the interprofessional team. • Promote staff satisfaction, patient satisfaction, and overall unit productivity. • Create and sustain trust between and among managers and staff. • Actively manage the process of change through good communication, staff involvement, training, sustained attention, and measurement and feedback. • Provide leadership to maintain compliance with governmental regulations and accreditation standards. Throughout this chapter, the term organization is used to refer to the hospital, home health agency, post–acute care facility, long-term care facility, ambulatory clinic, managed care company, or any other area in which a nurse might be employed to practice professional nursing. Legal and ethical issues are a critical component of nursing management, although it is not within the scope of this chapter to discuss these issues. The reader is encouraged to review Chapter 8 regarding legal issues and Chapter 9 regarding ethical issues. Leadership occurs any time a person attempts to influence the beliefs, opinions, or behaviors of a person or group (Hersey and Blanchard, 1988). Leadership is a combination of intrinsic personality traits, learned leadership skills, and characteristics of the situation. The function of a leader is to guide people and groups to accomplish common goals. For example, an effective nurse leader is able to inspire others on the health care team to make patient-centered care an important aspect of all care activities. • An appointed management position within the organization with responsibilities to perform administrative tasks such as planning staffing, performing employee performance reviews, controlling use of supplies and time, and meeting budget and productivity goals • A formal line of authority and accountability to ensure that safe and effective patient care is delivered in a manner that meets the organization’s goals and standards Leadership and management require power and authority to motivate people to act in a certain way. Authority is the legitimate right to direct others and is given to a person by the organization through an authorized position, such as nurse manager. For example, a nurse manager has the authority to direct staff nurses to work a specific schedule. Whereas authority is the legitimate right to direct others granted by the organization, power is the ability to motivate people to get things done with or without the legitimate right granted by the organization. The primary sources of power are as follows (Hersey et al, 1979): • Reward power comes from the ability to reward others for complying and may include such rewards as money, desired assignments, or acknowledgment of accomplishments. • Coercive power, the opposite of reward power, is based on fear of punishment for failure to comply. Sources of coercive power include withheld pay increases, undesired assignments, verbal and written warnings, and termination. • Legitimate power is based on an official position in the organization. Through legitimate power, the manager has the right to influence staff members, and staff members have an obligation to accept that influence. • Referent power comes from the followers’ identification with the leader. The admired and respected nurse is able to influence other nurses because of their desire to emulate her. • Expert power is based on knowledge, skills, and information. For example, nurses who have expertise in areas such as physical assessment or technical skills, or who keep up with current information on important topics will gain respect from others. • Information power is based on a person’s possession of information that is needed by others. • Connection power is based on a person’s relationship or affiliation with other people who are perceived as being powerful. • Identify the informal leaders in the work team, and develop an understanding of their source of power (see sources of power in the previous section). • Involve the informal leaders and other staff members in decision-making and change-implementation processes. • Clearly communicate the goals and work expectations to all staff members. • Do not ignore an informal leader’s attempt to undermine teamwork and change processes. Coaching and counseling the person and setting clear expectations may be required. Early leadership theory centered on describing the qualities or traits of leaders and has been commonly referred to as trait theory (Stogdill, 1974). Leadership trait theory was based on the assumption that leaders were born with certain leadership characteristics. Traits found to be associated with leadership include intelligence, alertness, dependability, energy, drive, enthusiasm, ambition, decisiveness, self-confidence, cooperativeness, and technical mastery (Stogdill, 1974). Although trait theories have been important in identifying qualities that distinguish today’s leaders, these theories have neglected the interaction between other elements of the leadership situation. Trait theories also have failed to recognize the possibility that leadership traits can be learned and developed through experience. However, by keeping in mind these traits associated with effective leadership, the new nurse can identify areas in which he or she should improve and develop. Researchers progressed from developing trait theory to studying the interaction between the leader and other variables of the leadership situation. Contemporary theories of leadership, such as situational and behavioral theories, have attempted to integrate the dynamics of the interaction among the leader, the worker, and elements of the leadership situation, arguing that effective leadership depends on several variables, including (1) organizational culture, (2) values of the leader and values of the followers, (3) influence of the leader or manager, (4) complexities of the situation, (5) work to be accomplished, and (6) environment (Marquis and Huston, 2012). In a contemporary concept of leadership, Burns (1978) identified and defined transformational leadership. Burns contends that there are two types of leaders: (1) the transactional leader, who is concerned with the day-to-day operations of the facility and (2) the transformational leader, who is committed to organizational goals, has a vision, and is able to empower others with that vision. The transformational leader is able to guide employees to feel pride in the work of the organization and to inspire them to be actively engaged to achieve the mission and goals of the organization. Transformational leaders spend time teaching and coaching, seek differing perspectives when faced with problems to solve, and seek new ways to improve the work environment. Box 16-1 compares characteristics of Burns’ (1978) transformational and transactional leadership styles. Studies have reported that nurse managers who demonstrate more transformational leadership characteristics achieve higher levels of staff satisfaction and work group effectiveness (Casida and Parker, 2011; Failla and Stichler, 2008; Raup, 2008). The implication for nurse managers is that transformational leadership is very effective in increasing staff satisfaction and work effectiveness. The student is encouraged to read more about transformational leadership and to seek out transformational leaders as mentors. However, it is important to note that even the most effective transformational leader will fail without possessing the day-to-day management skills of transactional leaders (Bass et al, 1987). Three major types of skills are required for effective leadership (Hersey and Blanchard, 1988): 1. Technical skills—for nurses, this includes clinical expertise and nursing knowledge 2. Human skills—the ability and judgment to work with people in an effective leadership role 3. Conceptual skills—the ability to understand the complexities of the overall organization and to recognize how and where one’s own area of management fits into the overall organization At the staff nurse level of management, a considerable amount of technical skill and clinical expertise is needed because the nurse generally is involved in direct supervision of patient care and may be required to help train and mentor nurses and other health care providers. As one advances from lower levels to higher levels in the organization, more conceptual skills are needed. Box 16-2 provides examples of technical, human, and conceptual practices required for nurse leaders. Behavioral theories emerged to explain aspects of management based on behaviors of managers, leaders, and followers. Three prevalent management behavior styles were identified by Lewin (1951) and White and Lippit (1960): authoritarian, democratic, and laissez-faire. Box 16-3 presents characteristics of these management styles, which vary in the amount of control exhibited by the manager and the amount of involvement that the staff has in decision making. At one extreme, the autocratic manager makes all decisions with no staff input and uses the authority of the position to accomplish goals. At the opposite extreme is the laissez-faire manager, who provides little direction or guidance and will forgo decision making. Democratic management is also often referred to as participative management because of its basic premise of encouraging staff members to participate in decision making. The systems theory views the organization as a set of interdependent parts that together form a whole (Thompson, 1967). The interdependent nature of the parts of the organization suggests that anything that affects the functioning of one aspect of the organization will affect the other parts of the organization. Open systems suggest that the organization is affected not only by internal changes among any of its parts, but also external environmental forces that will have a direct influence on the organization and vice versa—the internal forces will affect the external environment. In contrast to open systems theory, closed systems theory views the system as being totally independent of outside influences, which is an unrealistic view for health care organizations. To be successful, today’s health care organizations must be able to continually adapt to internal and external changes. Consider Case Study 16-1 to help explain systems theory. This example demonstrates open systems theory. As internal forces in one department (hospital administration) mandated changes that affected another area (RNs and patient care), internal forces (RNs) pushed for changes from the external environment (state nurses association and state government). The external environment may now force changes to the organization (hospital administration). The chaos theory is a more recently developed organizational theory that attempts to account for the complexity and randomness in organizations. Despite the implications of the word chaos, the theory actually suggests that a degree of order can be attained by viewing complicated behaviors and situations as predictable. Nurse managers may wish for balanced and steady work environments, but in reality they are dealing with, what seems at best, a chaotic system. Chaos theory says that variation is a normal part of managing health care systems. Based on chaos theory, a nurse manager knows that staff absences as a result of illness, sick children, and family emergencies are a fact of life, requiring the nurse manager to have backup plans in place in the event that staff members “call in” and are unable to report for their assigned shift. Other examples of variation in health care are cultural diversity, a constantly fluctuating patient census, and staffing shortages. Until nurses understand that these variations are a normal, predictable state in the organization and should be planned for, they may continue to experience excessive anxiety with the daily events that occur in health care organizations (McGuire, 1999). Classic theories of management suggest that the primary functions of managers are planning, organizing, and controlling (Stogdill, 1974). Leaders in nursing management have added two more functions to this list and now recognize five major management functions (Figure 16-1) as necessary for the management of nursing organizations: (1) planning, (2) organizing, (3) staffing, (4) directing, and (5) controlling (Marquis and Huston, 2012).
Nursing Leadership and Management
Chapter Overview
Leadership and Management Defined and Distinguished
Leadership Defined
Management Defined
Power and Authority
Formal and Informal Leadership
Leadership Theory
Leadership Trait Theory
Interactional Leadership Theories
Transformational Leadership
Leadership Skills
Management Theory
Organizational Theory
Systems Theory
Chaos Theory
Management Functions
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access