Nursing Care During Obstetric Procedures
Learning Objectives
After studying this chapter, you should be able to:
• Identify clinical situations in which specific obstetric procedures are appropriate.
• Explain risks, precautions, and contraindications for each procedure.
• Identify nursing considerations for each procedure.
• Identify methods to provide effective emotional support to the woman having an obstetric procedure.
• Apply the nursing process to plan care for the woman having a cesarean birth.
![]()
http://evolve.elsevier.com/McKinney/mat-ch/
Although labor is a normal process, special procedures are sometimes needed to help the mother or fetus. A physician or nurse-midwife performs these procedures while nurses provide supportive care. Descriptions of procedures and nursing considerations for each are addressed.
Amniotomy
Indications
Amniotomy (artificial rupture of the amniotic sac) is often done in conjunction with induction or stimulation of labor or to permit internal electronic fetal monitoring (see Chapter 17). Although it is a common procedure, amniotomy implies a commitment to delivery (Cunningham Leveno, Bloom, et al., 2010; Hobel & Zakowski, 2010).
Risks
Amniotomy is seen by many professionals and expectant mothers as harmless, and it usually is, but the nurse must observe for three major associated risks, and assist in any emergency procedures needed.
Prolapse of the Umbilical Cord
An immediate and continuing risk is that the umbilical cord will slip down in the gush of fluid. The cord can be compressed between the fetal presenting part and the woman’s pelvis, obstructing blood flow to and from the placenta and reducing fetal gas exchange.
Infection
With interruption of the membrane barrier, vaginal organisms have free access to the uterine cavity and may cause chorioamnionitis, or infection of the amniotic sac. The risk is low at first but increases as the interval between membrane rupture and birth increases. Birth within 24 hours of amniotomy is desirable in the term pregnancy, although there is no absolute time when infection occurs.
Abruptio Placentae
Abruptio placentae (premature separation of a normally implanted placenta) may occur if the uterus is distended when the membranes rupture. The risk is greater if there is excessive amniotic fluid in the uterus (hydramnios), because of greater uterine distention. As the uterus collapses with discharge of the amniotic fluid, the area of placental attachment shrinks. The placenta then no longer fits its implantation site and partially separates. A large area of placental disruption reduces fetal oxygenation, nutrition, and waste disposal.
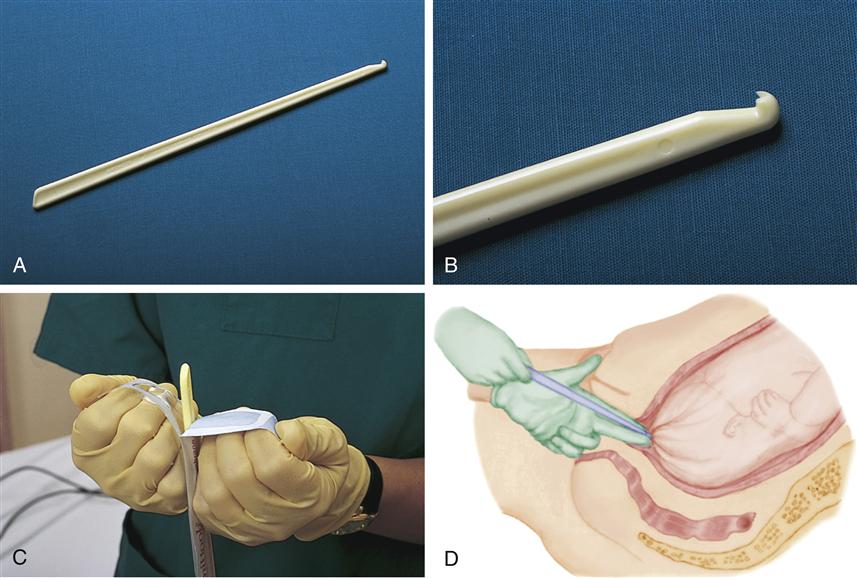
Technique
A disposable plastic hook (Amnihook) is commonly used to perforate the amniotic sac (Figure 19-1). The physician or nurse-midwife does a vaginal examination to determine cervical dilation and effacement, fetal station, and fetal presenting part. Amniotomy is deferred if the fetal presenting part is high in the pelvis or if the presentation is not cephalic. The risk for a prolapsed cord is greater in these situations because more room is available for the cord to slip down. In addition, a cesarean, or surgical, birth is usually performed for a noncephalic presentation.
The hook is passed through the cervix, and the membranes are snagged. The hole is enlarged with the finger, allowing fluid to drain.
Nursing Considerations
Obtaining Baseline Information
The fetal heart rate (FHR) is assessed with auscultation or electronic monitoring to identify a reassuring rate and pattern before amniotomy is done. A minimum of 20 to 30 minutes is needed for adequate fetal baseline evaluation and can be obtained with other admission information.
Assisting with Amniotomy
Before amniotomy, place underpads under the woman’s buttocks to absorb the fluid. One or more folded bath towels under the buttocks absorb amniotic fluid well. Other supplies needed are a disposable plastic hook, a sterile glove or pair of gloves, and a packet of sterile lubricant.
Providing Care after Amniotomy
Nursing care after amniotomy is the same as that after spontaneous membrane rupture.
Identifying Complications
Assess the FHR for at least 1 full minute after membrane rupture, whether spontaneous or by amniotomy. Nonreassuring rate or other electronic fetal monitor patterns or significant changes from previous assessments are reported promptly to the birth attendant. Cord compression is suspected if deep or prolonged variable decelerations occur during contractions or persistent bradycardia is present after contractions. Other nonreassuring FHR patterns also may occur (see Chapter 17).
Chart the quantity, color, and odor of the amniotic fluid. Refer to Chapter 16 for expected findings and signs of abnormality in the amniotic fluid.
Assess the woman’s temperature every 2 hours after the membranes rupture. Report elevations greater than 38° C
(100.4° F). Fetal tachycardia (sustained rate above 160 beats per minute [bpm]) often precedes maternal fever.
Promoting Comfort
Amniotic fluid leaks from the woman’s vagina after membranes rupture. Change the underpads regularly for comfort and to reduce the moist environment that favors bacterial growth.
Induction and Augmentation of Labor
Induction and augmentation of labor use artificial methods to stimulate uterine contractions. Techniques and nursing care are similar for both induction and augmentation. The U.S. prevalence of labor induction is more than 22% and has more than doubled since 1990. Late preterm births that were induced have more than doubled from 1990 to 2006 (iatrogenic, or the result of treatment ) and the number of cesarean births have increased with the rise in labor inductions. A nullipara who has a cesarean after an unsuccessful induction usually has repeat cesareans for all other babies (American College of Obstetricians and Gynecologists [ACOG], 2009a; Ehrenthal, Jiang, & Strobino, 2010; Hamilton, Martin, & Ventura, 2010; Martin, Kirmeyer, Osterman, et al., 2009). Few women who have regular prenatal care expect to deliver more than a few days past their due date.
Indications
Induction of labor, or artificial initiation of labor, is considered when ending the pregnancy benefits the woman or fetus and when labor and vaginal birth are considered safe. Labor induction is not done if the fetus must be delivered more quickly than the process permits; a cesarean birth would be performed instead. Examples of specific conditions that are indications for induction include (Simpson, 2008a):
• Fetal compromise (such as intrauterine growth restriction, maternal-fetal blood incompatibility)
• Chorioamnionitis (inflammation of the amniotic sac)
• Abruptio placentae (large abruptions require immediate delivery) (see Chapter 27)
Elective induction for convenience of the woman or her physician is not recommended, although it has become common. Factors such as a history of rapid labors and living a long distance from the hospital may be valid reasons for elective induction because of the possibility of birth in uncontrolled circumstances.
Prenatal testing may reveal a fetal anomaly for which specialized neonatal care at a distant facility will be needed. The mother may be transported to that facility for labor induction or cesarean birth, with the necessary equipment and specialists assembled to care for the newborn.
Augmentation of labor with oxytocin is considered when labor has begun spontaneously but progress has slowed or stopped because of poor contractions. The medical provider may use augmentation if progress is slower than expected, even if contractions seem to be adequate (ACOG, 2011a). The rate of oxytocin may be lower than induction.
Determining Whether Induction Is Indicated
The birth attendant evaluates whether labor and birth are safer for the woman or fetus than continuing the pregnancy. Labor is not induced if term gestation and/or fetal lung maturity are not established unless there is a compelling reason. Induction is more likely to be successful at term because prelabor cervical changes favor dilation.
The Bishop scoring system (Table 19-1) uses five factors to estimate cervical readiness for labor: cervical dilation, effacement, consistency, position, and fetal station. The Bishop score remains popular because of its ability to predict probable success of induction. The likelihood of vaginal birth is similar to that of spontaneous labor if the score is greater than 8 (ACOG, 2009b).
TABLE 19-1
BISHOP SCORING SYSTEM TO EVALUATE THE CERVIX
| SCORE | ||||
| FACTOR | 0 | 1 | 2 | 3 |
| Dilation | 0 cm | 1-2 cm | 3-4 cm | 5-6 cm |
| Effacement | 0-30% | 40%-50% | 60%-70% | ≥80% |
| Fetal station | −3 | −2 | −1 or 0 | +1 or +2 |
| Cervical consistency | Firm | Medium | Soft | |
| Cervical position | Posterior | Middle | Anterior | |
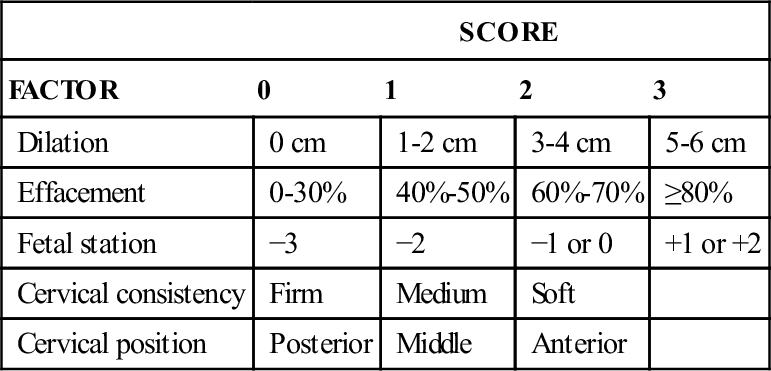
Modified from Bishop, E. H. (1964). Pelvic scoring for elective induction. Obstetrics and Gynecology, 24(2), 266-268.
Contraindications
Any contraindication to labor and vaginal birth is a contraindication to induction or augmentation of labor. These conditions may include:
• Placenta previa (implantation in lower uterus), which may result in hemorrhage during labor
• Abnormal presentation for which vaginal birth is often hazardous
• Umbilical cord prolapse, because immediate birth by cesarean is indicated
• Some uterine surgery, such as classic cesarean (see p. 427 and Figure 19-9) or extensive surgery for uterine fibroids
Other maternal or fetal conditions are not contraindications to induction but require individual evaluation, such as the following:
• One or more previous low transverse cesarean births (see Figure 19-9)
• Maternal heart disease, which varies in severity
• Severe maternal hypertension
• Uterine overdistention such as multifetal pregnancy, especially triplets or higher, and hydramnios
• Nonreassuring FHR patterns that do not yet mandate emergency delivery
Risks
Induction and augmentation of labor are associated with risks of spontaneous labor plus added risks of the procedure (Cunningham et al., 2010; Simpson, 2008a):
Technique
Surgical, medical, or mechanical methods may be used for labor induction or augmentation. Amniotomy is the method of surgical induction and augmentation, because rupturing membranes stimulates uterine contractions if the cervix is favorable (soft, some dilation and/or effacement). Medical methods for induction or augmentation use drugs such as prostaglandins or intravenous (IV) oxytocin (Pitocin), or both, to stimulate contractions. Mechanical methods of induction use a variety of intracervical inserts to gradually stretch and soften the cervix.
Cervical Ripening
Procedures to ripen (soften) the cervix and make it more likely to dilate with the forces of labor are a common adjunct to induction. Cervical ripening may be done the morning of induction or possibly the day before.
Medical Methods
Preparations containing prostaglandin E2 (PGE2, or dinoprostone) may be used to facilitate cervical ripening. Prostaglandin may be given as an intravaginal or intracervical gel or a timed-release vaginal insert (Table 19-2). It is administered in a setting in which fetal monitoring and emergency care, including immediate cesarean birth, are readily available.
TABLE 19-2
PROSTAGLANDIN PREPARATIONS FOR CERVICAL RIPENING AT TERM
| PROSTAGLANDIN GEL (DINOPROSTONE OR PREPIDIL) | VAGINAL INSERT | |
| DINOPROSTONE OR CERVIDIL | MISOPROSTOL (CYTOTEC) | |
| Dosage | ||
| 0.5 mg applied to cervix. May be repeated 6-12 hr later to a maximum of 1.5 mg (three applications) applied to the cervix; 2.5 mg vaginally. | 10 mg in a timed-release vaginal insert. Remove after 12 hr or at onset of active labor. | One quarter of 100-mcg tablet vaginally (approximately 25 mcg; see cautions below). Also used for labor induction by repeating 25-mcg dose every 3-6 hr. A 50-mcg dose is associated with hypertonic contractions. |
| Actions for Uterine Tachysystole, with or without Nonreassuring Fetal Heart Rate Pattern | ||
| Place woman in side-lying position. Provide oxygen by facemask at 8-10 L/min. Administer tocolytic drug such as terbutaline or magnesium sulfate. Typically begins 1 hr after gel application. Higher incidence with vaginal application. | Same as for dinoprostone gel. Remove insert. Hypertonic uterine activity may occur up to 9½ hr after insert placement. Greater incidence than with lower-dose intracervical dinoprostone gel. | Same as for dinoprostone gel. Higher doses or more frequent administration is more likely to cause excessive contractions, which may be accompanied by a nonreassuring FHR pattern. |
| When Oxytocin Induction May Begin | ||
| Safe interval has not been established. Delaying oxytocin administration for 6-12 hr after total intracervical dose of 1.5- or 2.5-mg vaginal dose recommended. | 30-60 min after removal of insert. | At least 4 hr after last dose. |
| Precautions and Comments | ||
| Limit dinoprostone gel to maximum of 1.5 mg dinoprostone gel in 24 hr. Woman should remain recumbent with lateral uterine displacement for 15-30 min after application. Has increased effect if combined with other oxytocics such as oxytocin (Pitocin). Increases hypertensive effect of the herb ephedra. Use caution in women with asthma, hypertension, glaucoma, or severe renal or hepatic dysfunction, ischemic heart disease. | Remove after 12 hr or when active labor begins. Adverse effects can be reduced within 15 min of removal. Most expensive of the prostaglandin options. | Misoprostol is currently FDA approved only for treatment of peptic ulcers but is widely used for cervical ripening and induction of labor. Manufacturer does not intend to seek approval, but American College of Obstetricians and Gynecologists supports its use for these purposes. 100-mcg tablet is not scored. Pharmacist should prepare the 25-mcg dose for best accuracy. Cost is about 1%-2% that of other prostaglandin preparations. Contraindicated in the woman with a previous cesarean or other uterine surgery. |
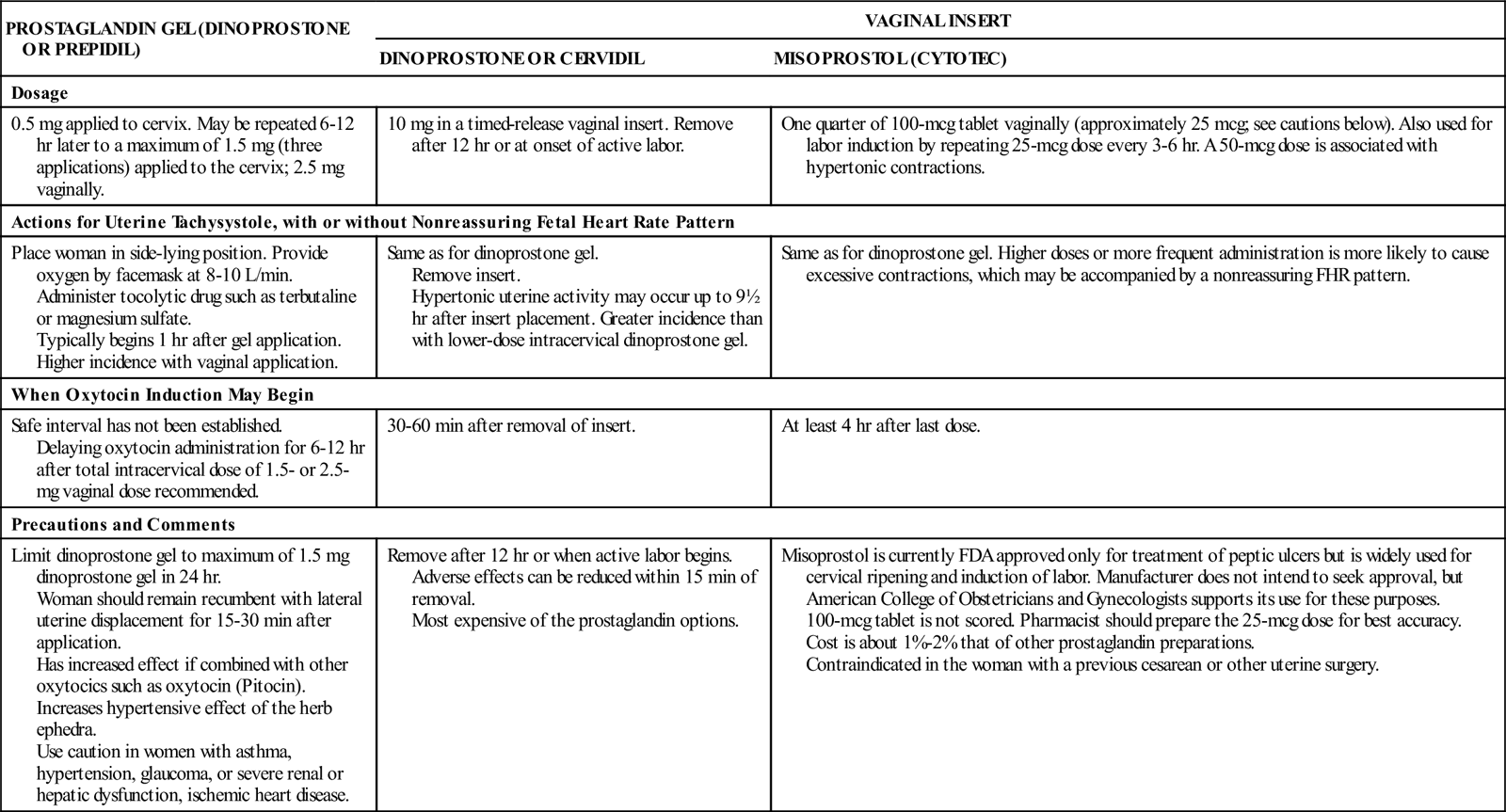
NOTE: Dosages may be higher in cases of fetal death.
FDA, U.S. Food and Drug Administration; FHR, fetal heart rate.
From American Academy of Pediatrics & American College of Obstetricians and Gynecologists. (2007). Guidelines for perinatal care (6th ed.). Elk Grove Village, IL, and Washington, DC: Author; American College of Obstetricians and Gynecologists (ACOG). (2009). Induction of labor (ACOG Practice Bulletin No. 107). Washington, DC: Author; Cunningham, F. G., Leveno, K. J., Bloom, S. L., et al. (2010). Williams obstetrics (23rd ed.). New York: McGraw-Hill.
Prostaglandin should be given cautiously to women who have asthma; glaucoma; ischemic heart disease; or pulmonary, hepatic, or renal disease. The major adverse reaction to prostaglandin for induction is tachysystole that can reduce placental blood flow and fetal oxygen exchange. The FHR and uterine activity should be monitored before prostaglandin insertion for a baseline and at least 30 minutes afterward for nonreassuring FHR patterns or excessive contractions.
Misoprostol (Cytotec) is popular for preinduction cervical ripening and labor induction because of its low cost, stability, and ease of use (see Table 19-2). Misoprostol is a synthetic prostaglandin tablet that is used for prevention of gastric ulcers. It’s use for cervical ripening or labor induction remains an off-label use for misoprostol.
Mechanical Methods
Any of several techniques use mechanical means to ripen and begin dilation of the cervix:
Oxytocin Administration
Oxytocin is a powerful drug, and it is impossible to predict a woman’s response to it. Several precautions reduce the chance of adverse reactions in the mother and fetus:
• Oxytocin is diluted in an isotonic solution and given as a secondary (piggyback) infusion so that it can be stopped quickly if complications develop (Figure 19-2). Oxytocin solutions are often premixed by the pharmacy.
The woman’s uterus becomes more sensitive to oxytocin as labor progresses. Oxytocin administration is therefore titrated to uterine and fetal response. The rate of oxytocin infusion may be gradually reduced when the woman is in the active phase of labor, about 5 to 6 cm of cervical dilation. It may be stopped or reduced after her membranes rupture. If uterine tachysystole makes it necessary to stop oxytocin, the medical decision about restarting administration must be individualized. When labor is augmented with oxytocin, a lower total dose is usually needed to achieve adequate contractions.
Nursing Considerations
In addition to basic intrapartum care, the nurse observes the woman and fetus for complications and takes corrective actions if abnormalities are noted. Nursing care is similar for the woman who has cervical ripening.
The nurse has a great responsibility when administering oxytocin or other uterine stimulants to a pregnant woman. The nurse must maintain safeguards to both mother and fetus when administering oxytocin and recognize when to start, change, or stop its infusion and when to notify the physician. Facility policies related to oxytocin must clearly support correct nursing and medical actions (Pearson, 2011).
Observing the Fetal Response
Oxytocin stimulates uterine contractions, and they may become too strong (hypertonic). Hypertonic contractions can reduce placental blood flow and therefore reduce exchange of fetal oxygen and waste products. Before induction or augmentation of labor, the nurse determines whether the FHR and patterns are reassuring. The FHR is charted in the labor record at least every 15 minutes during first-stage labor and every 5 minutes during the second stage (Simpson, 2008b).
The nurse remains alert for FHR patterns that suggest reduced placental exchange secondary to contractions that are too strong, too long, or do not relax at least 30 seconds (now termed tachysystole). Examples of these patterns are fetal bradycardia (<110 bpm at term), tachycardia (persistent rate >160 bpm at term), late decelerations (slowing after the peak of the contraction), and decreased FHR variability (reduced rate fluctuations) that is not explained by medications or fetal sleep. Reduced placental exchange also may have causes other than excess uterine activity, such as maternal hypotension or maternal diabetes. The nurse must assess the woman and fetus carefully to identify the most likely cause of the problem and the indicated corrective actions.
If nonreassuring FHR patterns occur or if contractions are hypertonic, the nurse takes steps to reduce uterine activity and increase fetal oxygenation. These steps include:
2. Keeping the woman on her side to prevent aortocaval compression and increase placental blood flow.
The physician may order a drug to reduce uterine activity, such as terbutaline (Brethine) or magnesium sulfate. Terbutaline, 0.25 mg subcutaneously, can be given quickly to reduce uterine contractions.
Observing the Mother’s Response
Uterine activity must be assessed for tachysystole that can reduce fetal oxygenation and contribute to uterine rupture. Contractions are assessed for frequency, duration, and intensity, and uterine resting tone is assessed for relaxation of at least 30 seconds between contractions. Uterine activity observations are charted at the same intervals as the FHR patterns. Corrective actions for tachysystole are the same as those listed in the discussion of the fetal response. In addition, a tocolytic drug such as terbutaline may be given.
The woman’s blood pressure and pulse are taken every 30 minutes or with each oxytocin dose change to identify changes from her baseline. Her temperature is checked every 4 hours (every 2 hours after membrane rupture) to identify infection.
Recording intake and output identifies fluid retention, which precedes water intoxication. Signs and symptoms of water intoxication include headache, blurred vision, behavioral changes, increased blood pressure and respirations, decreased pulse, rales, wheezing, and coughing.
After birth, observe for postpartum hemorrhage caused by uterine relaxation. Postpartum uterine atony is more likely if the woman has received oxytocin for a long time, because the uterine muscle becomes fatigued and does not contract effectively to compress vessels at the placental site. It is manifested by a soft uterine fundus and excess amounts of lochia, usually with large clots. Hypovolemic shock may occur with hemorrhage.