Nursing Assessment
Objectives
• Discuss the relationship between critical thinking and nursing assessment.
• Explain the process of data collection.
• Differentiate between subjective and objective data.
• Describe the methods of data collection.
• Discuss the process of conducting a patient-centered interview.
• Describe the components of a nursing history.
• Explain the differences among comprehensive, problem-oriented, and focused assessments.
• Explain the relationship between data interpretation and validation.
Key Terms
Assessment, p. 207
Back channeling, p. 213
Closed-ended questions, p. 214
Concomitant symptoms, p. 215
Cue, p. 208
Database, p. 207
Functional health patterns, p. 208
Inference, p. 208
Nursing health history, p. 214
Nursing process, p. 206
Objective data, p. 210
Open-ended questions, p. 213
Review of systems (ROS), p. 216
Subjective data, p. 210
Validation, p. 217
![]()
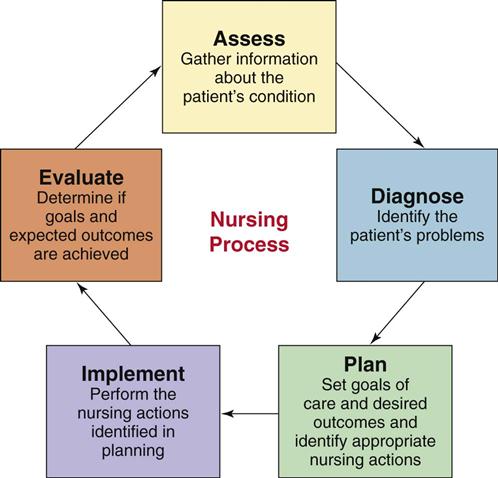
The nursing process is a critical thinking process that professional nurses use to apply the best available evidence to caregiving and promoting human functions and responses to health and illness (American Nurses Association, 2010). It is the fundamental blueprint for how to care for patients. The nursing process is also a standard of practice, which, when followed correctly, protects nurses against legal problems related to nursing care (Austin, 2008). As a nursing student, you learn the five steps of the nursing process—assessment, diagnosis, planning, implementation, and evaluation—as if they were a linear process (Fig. 16-1). However, in fact the nursing process is dynamic and continuous; and, after more experience in practice, you learn to move back and forth among the various steps (Potter et al., 2005). Consider the following scenario that was also described in Chapter 15:
Mr. Jacobs is a 58-year-old patient who had a radical prostatectomy (removal of prostate gland) for prostate cancer yesterday. He is married to Martha, who has been at his bedside most of the morning. His nurse, Tonya Moore, just started the day shift on the surgical unit and finds the patient lying flat in bed with arms tensed and extended along his sides. When Tonya checks the surgical wound and drainage device, she notes that Mr. Jacobs winces when she gently places her hands to palpate around the incisional area. She asks Mr. Jacobs when he last turned onto his side, and he responds, “Not since last night some time.” Tonya asks Mr. Jacobs if he is having incisional pain, and he nods yes, saying, “It hurts too much to move.” Tonya clarifies, “On a scale of 0 to 10 with 0 being no pain and 10 being the worst pain you have ever had, rate how you feel now.” Mr. Jacobs states, “Oh, this is at least a 7.” Tonya considers the information she has observed and learned from Mr. Jacobs to determine that he is in pain and has reduced mobility because of it. She decides that she needs to take action to relieve Mr. Jacobs’ pain so she can turn him more frequently and begin to get him out of bed for his recovery.
Each time you meet a patient, you apply the nursing process, as Tonya did while caring for Mr. Jacobs, to provide appropriate and effective nursing care. The process begins with the first step, assessment, the gathering and analysis of information about the patient’s health status. You then make clinical judgments from the assessment to identify the patient’s response to health problems in the form of nursing diagnoses. Once you define appropriate nursing diagnoses, you create a plan of care. Planning includes setting goals and expected outcomes for your care and selecting interventions (nursing and collaborative) individualized to each of the patient’s nursing diagnoses. The next step, implementation, involves performing the planned interventions. After performing interventions, you evaluate the patient’s response and whether the interventions were effective. The nursing process is central to your ability to provide timely and appropriate care to your patients.
The nursing process is a variation of scientific reasoning. Practicing the five steps of the nursing process allows you to be organized and conduct your practice in a systematic way. You learn to make inferences about the meaning of a patient’s response to a health problem or generalize about the patient’s functional state of health. Through assessment a pattern begins to form. For example, if Mr. Jacobs is having incisional pain, the data allow Tonya to infer that his mobility is limited. Tonya gathers more information (e.g., palpating gently over the incision, having Mr. Jacobs rate the severity of discomfort, and noting that he limits movement) until an accurate classification of the patient’s problem is determined such as the following nursing diagnosis: acute pain related to trauma of incision and the diagnosis of impaired physical mobility related to incisional pain. Clearly defining your patients’ problems provides the basis for planning and implementing nursing interventions and evaluating the outcomes of care.
Critical Thinking Approach to Assessment
Assessment is the deliberate and systematic collection of information about a patient to determine his or her current and past health and functional status and his or her present and past coping patterns (Carpenito-Moyet, 2009). Nursing assessment includes two steps:
The purpose of assessment is to establish a database about the patient’s perceived needs, health problems, and responses to these problems. In addition, the data reveal related experiences, health practices, goals, values, and expectations about the health care system.
When a plumber comes to your home to repair a problem you describe as a “leaking faucet,” the plumber checks the faucet, its attachments to the water line, and the water pressure in the system to determine the real problem. A patient presents an initial health problem to you. For example, Mr. Jacobs presents with signs of pain following surgery. You then proceed to observe his behaviors, ask questions about the nature of the problem, listen to the cues he provides, and conduct a physical examination (see Chapter 30). You also usually interview family members who are familiar with the patient’s health problems and any existing medical record data. The data you collect fall into different sets or patterns of information that point to a diagnostic conclusion. Once a plumber knows the source of the leaking faucet, he is able to repair it. Once you know the nature and source of a patient’s specific health problems (such as Mr. Jacob’s incisional pain), you are able to provide interventions that will restore, maintain, or improve the patient’s health.
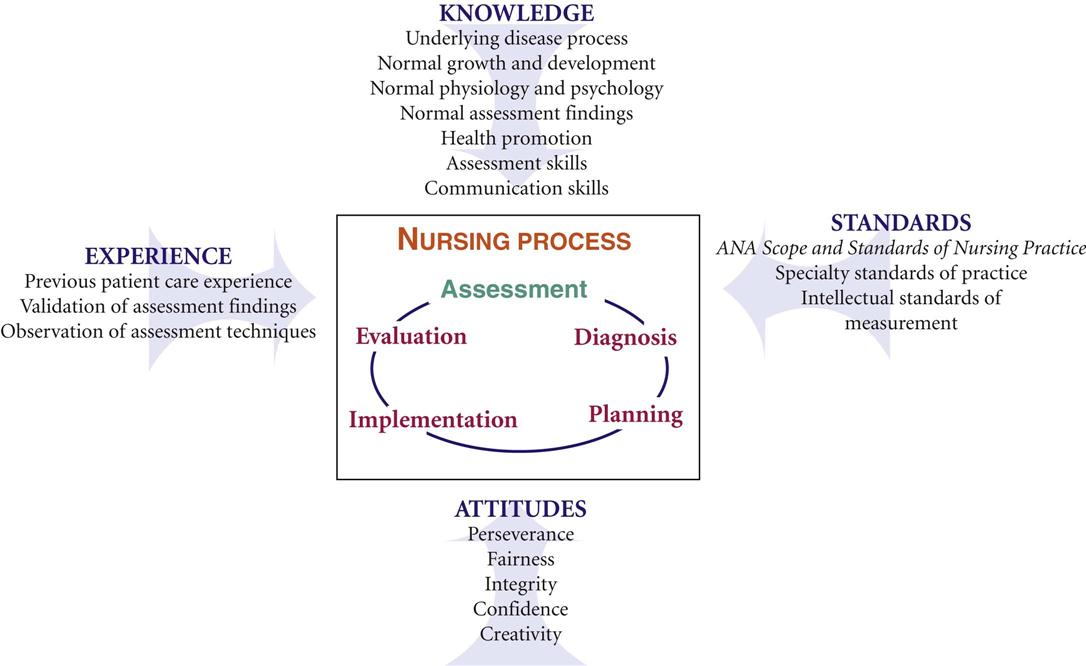
Critical thinking is a vital part of assessment (see Chapter 15). It allows you to see the big picture when you form conclusions or make decisions about a patient’s health condition. While gathering data about a patient, you synthesize relevant knowledge, recall prior clinical experiences, apply critical thinking standards and attitudes, and use standards of practice to direct your assessment in a meaningful and purposeful way (Fig. 16-2). Your knowledge from the physical, biological, and social sciences allows you to ask relevant questions and collect relevant history and physical assessment data related to the patient’s presenting health care needs. For example, Tonya knows that Mr. Jacobs had his prostate gland removed. She reviewed her medical-surgical textbook and learned that a radical prostatectomy involves removal of a lot of tissue, including the prostate gland, seminal vesicles, part of the bladder neck, and lymph nodes. This knowledge helps her to recognize that considerable swelling can potentially create acute pain; thus she decides to inspect and palpate around Mr. Jacob’s incisional area. She also questions Mr. Jacobs about how the discomfort affects his ability to turn or move in bed. Using good communication skills through interviewing and applying critical thinking intellectual standards (such as being precise and accurate in using a pain scale) enables Tonya to collect complete, accurate, and relevant data.
Prior clinical experience contributes to the skills of assessment. For example, Tonya cared for a patient with surgical incision pain in the past and knows that pain is often disabling and limits a patient’s normal motion. This experience allows Tonya to thoroughly assess the extent to which pain affects the patient’s ability to move and eventually get out of bed, an important step in Mr. Jacob’s recovery. Validation of any abnormal assessment findings and personal observation of assessments performed by skilled professionals help you become competent in assessment. You also learn to apply standards of practice and accepted standards of “normal” for physical assessment data when assessing patients. Use of critical thinking attitudes such as curiosity, perseverance, and confidence ensure you complete a comprehensive database.
Data Collection
You perform assessment to gather information needed to make an accurate judgment about a patient’s current condition (Magnan and Maklebust, 2009). Your information comes from:
• The patient, through interview, observations, and physical examination.
• Family members or significant others’ reports and response to interviews.
• Other members of the health care team.
• Scientific literature (evidence about assessment techniques and standards).
As you begin a patient assessment, think critically about what to assess for that specific patient. Determine which questions or measurements are appropriate based on your clinical knowledge and experience and your patient’s health history and responses. When you first meet a patient, perform a quick screening. Usually your screening is based on a treatment situation. For example, a community health nurse assesses the patient’s neighborhood and community; an emergency department nurse uses the ABC (airway-breathing-circulation) approach; and a surgical nurse focuses on the patient’s symptoms following surgery, the expected healing response, and potential complications. For Mr. Jacobs, Tonya first focuses on the nature and severity of his pain, the risk of limited postoperative mobility, and the possibility that the wound is infected. She later expands her assessment to determine how Mr. Jacobs is adjusting emotionally to his surgery.
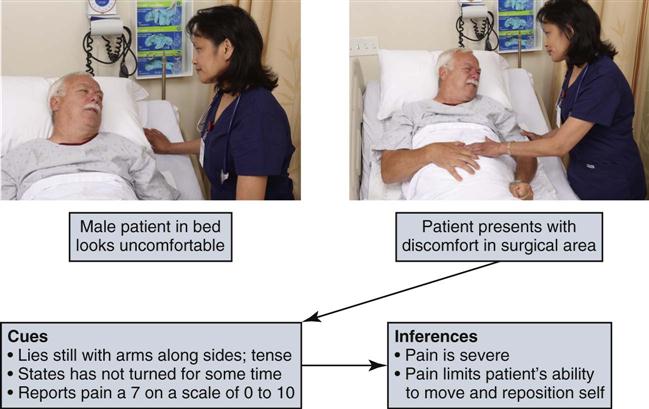
You learn to differentiate important data from the total data collected. A cue is information that you obtain through use of the senses. An inference is your judgment or interpretation of these cues (Fig. 16-3). For example, a patient crying is a cue that possibly implies fear or sadness. You ask the patient about any concerns and make known any nonverbal expressions you notice in an effort to direct the patient to share his or her feelings. It is possible to miss important cues when you conduct an initial overview. However, always try to interpret cues from the patient to know how in depth to make your assessment. Remember, thinking is human and imperfect. You acquire appropriate thinking processes when conducting assessments but expect to make mistakes in missing important cues (Lunney, 2006). Assessment is dynamic and allows you to freely explore relevant patient problems as you discover them.
After your observational screening, focus on the assessment cues and patterns of information that suggest problem areas. There are two approaches to a comprehensive assessment. One involves use of a structured database format, based on an accepted theoretical framework or practice standard. Gordon’s model of 11 functional health patterns (1994) (Box 16-1) is an example. The theory or practice standard provides categories of information for you to assess. Gordon’s functional health patterns model offers a holistic framework for assessment of any health problem. Tonya plans to direct her assessment of Mr. Jacobs to the cognitive-perceptual pattern to learn more about what the patient knows about the surgery and his prognosis and how he prefers to learn and make decisions about his care. Tonya is anticipating his need for education about postoperative recovery. She also plans to assess his sexuality-reproductive pattern to determine how he is accepting the potential change in sexual function resulting from surgery. A theoretical or standard-based assessment provides for a comprehensive review of a patient’s health care problems.
An assessment moves from the general to the specific. For example, you assess all of Gordon’s 11 functional health patterns and then determine if patterns or problems appear in your data. You then ask more focused questions about the health patterns that suggest a problem exists. You organize patterns of behavior and physiological responses that relate to a functional health category. The complete assessment of the 11 functional health patterns represents the interaction of the patient and the environment, which Gordon calls biopsychosocial integration. According to Gordon (1994), you cannot understand one health pattern without knowledge of the other patterns. Ultimately your assessment identifies functional patterns (patient strengths) and dysfunctional patterns (nursing diagnoses) that help you develop the nursing care plan.
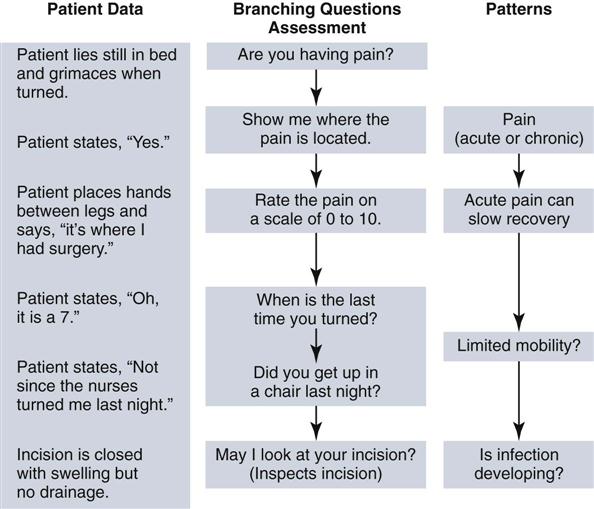
The second approach for conducting a comprehensive assessment is the problem-oriented approach. You focus on the patient’s presenting situation and begin with problematic areas such as incisional pain or limited understanding of postoperative recovery. You ask the patient follow-up questions to clarify and expand your assessment so you can understand the full nature of the problem. Later your physical examination further confirms your observations. Tonya’s assessment of Mr. Jacobs ensures that she knows the type of pain he is having and the extent to which it limits his activities. Table 16-1 offers an example of a problem-focused assessment. Once you complete the assessment, thoroughly analyze the extent and nature of a patient’s problem so you are able to later develop a care plan.
TABLE 16-1
Example of Problem-Focused Patient Assessment: Pain
| PROBLEM AND ASSOCIATED FACTORS | QUESTIONS | PHYSICAL ASSESSMENT |
| Nature of pain | Describe your pain for me. Place your hand over the area that hurts or is uncomfortable. | Observe nonverbal cues. Observe where patient points to pain; note if it radiates or is localized. |
| Precipitating factors | Do you notice if pain worsens during any activities or specific time of day? Is pain associated with movement? | Observe if patient demonstrates nonverbal signs of pain during movement, positioning, swallowing. |
| Severity | Rate your pain on a scale of 0 to 10. | Inspect area of discomfort; palpate for tenderness. |
Whatever approach you use to collect data, you begin to cluster cues, make inferences, and identify emerging patterns and potential problem areas. To do this well you critically anticipate, which means that you try to stay a step ahead of the assessment. Think about what the data tell you. Remember to always have supporting cues before you make an inference. Your inferences direct you to further questions. Once you ask a patient a question or make an observation, patterns form, and the information branches to an additional series of questions or observations (Fig. 16-4). Knowing how to probe and frame questions is a skill that grows with experience. You learn to decide which questions are relevant to a situation and to attend to accurate interpretations of data.
Types of Data
There are two primary sources of data: subjective and objective. Subjective data are your patients’ verbal descriptions of their health problems. Only patients provide subjective data. For example, Mr. Jacobs’s report of incision pain and his expression of concern about whether the pain means that he will not be able to go home as soon as he hoped are subjective findings. Subjective data usually include feelings, perceptions, and self-report of symptoms. Only patients provide subjective data relevant to their health condition. The data sometimes reflect physiological changes, which you further explore through objective data collection.
Objective data are observations or measurements of a patient’s health status. Inspecting the condition of a surgical incision or wound, describing an observed behavior, and measuring blood pressure are examples of objective data. The measurement of objective data is based on an accepted standard such as the Fahrenheit or Celsius measure on a thermometer, inches or centimeters on a measuring tape, or known characteristics of behaviors (e.g., anxiety or fear). When you collect objective data, apply critical thinking intellectual standards (e.g., clear, precise, and consistent) so you can correctly interpret your findings.
Sources of Data
As a nurse you obtain data from a variety of sources that provide information about the patient’s current level of wellness and functional status, anticipated prognosis, risk factors, health practices and goals, responses to previous treatment, and patterns of health and illness.
Patient
A patient is usually your best source of information. Patients who are conscious, alert, and able to answer questions correctly provide the most accurate information about their health care needs, lifestyle patterns, present and past illnesses, perception of symptoms, responses to treatment, and changes in activities of daily living. Always consider the setting for your assessment and your patient’s condition. A patient experiencing acute symptoms in an emergency department will not offer as much information as one who comes to an outpatient clinic for a routine checkup. An older adult requires more time than someone younger, and often multiple visits are required to gather a complete database (Seidel et al., 2011) (Box 16-2). Always be attentive and show a caring presence with patients (see Chapter 7). Let a patient know you are interested in what he or she has to say. Patients are less likely to fully reveal the nature of their health care problems when nurses show little interest or are easily distracted by activities around them.
Family and Significant Others
Family members and significant others are primary sources of information for infants or children; critically ill adults; and patients who are mentally handicapped, disoriented, or unconscious. In cases of severe illness or emergency situations, families are often the only sources of information for nurses and other health care providers. The family and significant others are also important secondary sources of information. They confirm findings that a patient provides (e.g., whether he takes medications regularly at home or how well he sleeps or eats). Include the family when appropriate. Remember, a patient does not always want you to question or involve the family. You must obtain a patient’s agreement to include family members or friends. Often spouses or close friends sit in during an assessment and provide their view of the patient’s health problems or needs. Not only do they supply information about the patient’s current health status, but they are also able to tell when changes in the patient’s status occurred. Family members are often very well informed because of their experiences living with the patient and observing how health problems affect daily living activities. Family and friends make important observations about the patient’s needs that can affect the way care is delivered (e.g., how a patient eats a meal or how he or she makes choices).
Health Care Team
You frequently communicate with other health care team members in gathering information about patients. In the acute care setting the change-of-shift report is how nurses from one shift communicate information to nurses on the next shift (see Chapter 26). During the report you have the chance to collect the first set of information about patients assigned to your care. Researchers found that bedside rounds, also called bedside handover, promote patient-centered care (Chaboyer, McMurray, and Wallis, 2010). During bedside rounds, the nurse who is completing care for a shift, the patient, and the nurse assuming care for a shift share information about the patient’s condition, status of problems, and treatment plan for the next shift. In some settings other health care team members participate in the rounds. When nurses, physicians, physical therapists, social workers, or other staff consult on a patient’s condition, they share information about how the patient is interacting within the health care environment, the patient’s reactions to treatment, and the result of diagnostic procedures or therapies. Every member of the team is a source of information for identifying and verifying information about the patient.
Medical Records
The medical record is a source for the patient’s medical history, laboratory and diagnostic test results, current physical findings, and the primary health care provider’s treatment plan. The record is a valuable tool for checking the consistency and similarities of your personal observations. Data in the records offer a baseline and ongoing information about the patient’s response to illness and progress to date. The Health Insurance Portability and Accountability Act (HIPAA) of 1996 has a privacy rule that came into effect on April 14, 2003 to set standards for the protection of health information (USDHHS, 2003). Information in a patient’s record is confidential. Each health care agency has policies governing how the patient’s health information can be shared among health care providers (see Chapter 26). It is important to know organization policies for reviewing a patient’s medical record for the purpose of assessment.
Other Records and the Scientific Literature
Educational, military, and employment records sometimes contain significant health care information (e.g., immunizations). If a patient received services at a community health center or different hospital, you need written permission from the patient or guardian to access the records. The HIPAA regulations protect access to patients’ health information. The privacy rule allows health care providers to share protected information as long as they use reasonable safeguards. Check the policy of your agency for HIPAA guidelines.
Reviewing nursing, medical, and pharmacological literature about a patient’s illness completes your assessment database. This review increases your knowledge about the patient’s diagnosed problems, expected symptoms, treatment, prognosis, and established standards of therapeutic practice. The scientific literature offers evidence to direct you on how and why to conduct assessments for particular patient conditions. A knowledgeable nurse obtains relevant, accurate, and complete information for the assessment database.
Nurse’s Experience
Through clinical experience a nurse observes other patients; recognizes clinical changes; and learns the types of questions to ask, choosing only the questions that will give the most useful information. A nurse’s expertise develops after testing and refining inferences, questions, and principle- or standard-based expectations. For example, while caring for Mr. Jacobs, Tonya has learned what a prostatectomy incision looks like and how a patient responds to the associated discomfort. In the future Tonya will more quickly recognize the behavior of a patient in acute pain and how it affects normal mobility. Practical experience and the opportunity to make clinical decisions strengthen your critical thinking.
Methods of Data Collection
As a nurse you use patient-centered interviews, the nursing health history, physical examination, and results of laboratory and diagnostic tests to collect data for a patient’s assessment database.
Patient-Centered Interview
A patient-centered interview is an approach for obtaining from patients the data that are needed to foster a caring nurse-patient relationship, adherence to interventions, and treatment effectiveness (Smith et al., 2006). The interview technique is the basis of a conceptual model used by nurse practitioners to form long-term therapeutic relationships with patients (Lein and Wills, 2007). However, the model has aspects that are useful to all nurses when conducting interviews for patient assessment. The partnership that forms in a patient-centered interview empowers a patient, promotes mutual decision making with the nurse, and ensures continuity of care (Dontje et al., 2004).
The expectation in a busy acute care setting such as a hospital nursing unit or clinic is for nurses to complete in a limited amount of time a patient history and nursing assessment. In the home health setting there is usually more time and fewer distractions; this allows a nurse to conduct a thorough interview. Agencies set standards for the type of information to be collected in health histories. However, there is a risk that standard assessments do not capture the patient’s full story. In a patient-centered interview an organized conversation with the patient allows the patient to set the initial focus and initiate discussion about his or her chief problems or reasons for seeking health care (Lein and Wills, 2007).
A successful interview requires preparation. Collect available information about the patient before starting the interview. For example, review the information you learn during a change-of-shift report and then plan to interview the hospitalized patient as you make patient rounds and before you begin to provide ordered interventions. Create a favorable environment for the interview. A good interview environment is free of distractions, unnecessary noise, and interruptions. The patient is more likely to be open and honest if the interview is private (i.e., out of earshot of other patients, visitors, or staff). Timing is important in avoiding interruptions. If possible, set aside a 10- to 15-minute period when no other activities are planned. More time is even better but is difficult to plan when you have multiple patients. During the interview always observe your patient for signs of discomfort or fatigue and plan accordingly. Remember to let a patient decide whether to involve the family in the interview. After an initial interview, follow-up discussions allow you to learn more about a patient’s situation and focus on specific problem areas. An initial patient-centered interview involves: (1) setting the stage, (2) gathering information about the patient’s chief concerns or problems and setting an agenda, (3) collecting the assessment or a nursing health history, and (4) terminating the interview.
Setting the Stage
Greet the patient using his or her full name, introduce yourself and explain your role (if it is the first time you have met), and remove any barriers to privacy by closing a room curtain or shutting a door. This is the orientation phase of an interview. When you explain the reason for collecting a health history, also assure the patient that any information obtained remains confidential and is used only by health care professionals who provide his or her care. HIPAA regulations require patients to sign an authorization before you collect personal health data (USDHHS, 2003). Refer to your agency policy for the authorization process.
After giving Mr. Jacobs pain medication for his incisional pain, Tonya waits 30 minutes and decides to take the time to assess Mr. Jacobs more fully. She reviews the surgical summary in the chart and the last set of nurses’ notes and enters the patient’s room.
Tonya: Mr. Jacobs, I am Tonya Moore. I did not fully introduce myself earlier when you looked so uncomfortable. You look a bit more comfortable now. Can you rate your pain again for me on a scale of 0 to 10?”
Mr. Jacobs: “Yes, I think the medicine has helped. I would rate the pain a 4.”
Tonya: “Good. If you’re comfortable, I’d like to spend about 10 minutes to better understand what you know about your surgery and discuss it with you. Everything you share will be confidential between you and the persons providing your care. I will let nurses on the next shift know about your care.”
Mr. Jacobs: “Ok, I would appreciate that.”
Set an Agenda
You begin an interview by gathering information about the patient’s current chief concerns or problems and setting an agenda. Remember, the best clinical interview focuses on the patient, not your agenda. Let the patient know your purpose (such as collecting an assessment or a nursing history) and ask the patient for his or her list of concerns or problems. This is the time that allows the patient to feel comfortable speaking with you and become an active partner in decisions about care. The professionalism and the competence that you show when interviewing patients strengthens the nurse-patient relationship.
Tonya: “I’m going to ask you questions about what you know about your surgery and what you need to do once you go home. But first tell me your main concerns.”
Mr. Jacobs: “Concerns, you mean about the surgery?”
Tonya: “Yes, or any other health problems you would like to discuss.”
Mr. Jacobs: “Well, I hope they got all of the cancer. I want to do what I need to do to get out of here as soon as I can.”
Tonya: “Ok, Is there anything else?”
Mr. Jacobs: “I’m worried about my wife and me. My doctor told me that the surgery could change our ability to have sex.”
Tonya: “Ok, your doctor will talk to you about your tumor. Don’t be afraid to ask him questions. Which changes concern you?
Mr. Jacobs: “Well I worry that, you know, I may not be able to have intercourse.”
Tonya: “It’s true; that is a risk of surgery. It’s important to learn from the doctor whether there was any nerve injury during surgery. It’s something you need to ask him. And we can discuss it further when you know the results. Now let me ask you about your expectations after surgery so we can have a teaching plan for you. Does that sound reasonable?”
Mr. Jacobs: “Yes, I’m not sure what to expect before I get out of here.”
Collect the Assessment or Nursing Health History
Start an assessment or a health history with open-ended questions that allow patients to describe more clearly their concerns and problems. For example, you can begin by having the patient explain symptoms or physical concerns, describe what he or she knows about the health problem, or ask him or her to describe health care expectations. Use attentive listening and other therapeutic communication techniques (see Chapter 24) that encourage a patient to tell his or her story. Observe verbal cues the patient expresses. Stay focused and orderly and do not rush. An initial interview (e.g., the one you conduct to collect a complete nursing history) is more extensive. You gather information about the patient’s concerns and then complete all relevant sections of the nursing history (see the following dialogue). Ongoing interviews, which occur each time you interact with your patient, do not need to be as extensive. An ongoing interview allows you to update the patient’s status and concerns, focus on changes previously identified, and review new problems. In the case study Tonya is gathering information to plan her postoperative teaching for Mr. Jacobs.
Tonya: “Mr. Jacobs, tell me what you expect over the next few days before you go home.”
Mr. Jacobs: “Well, the doctor did tell me that I would have this catheter in my bladder after I go home. But I don’t know if I have to do anything with this dressing over my stitches.”
Tonya: “Un huh, go on.”
Mr. Jacobs: “Will I have something to take for this pain as long as I am here, and what will I have to take at home?”
Tonya: “Yes, your doctor has ordered your pain medicine every 4 hours around the clock. You need to tell us when you begin to feel uncomfortable. You’ll have a pain medicine prescribed when you go home. Do you have any other concerns or questions about your surgery?”
Mr. Jacobs: “No, I don’t think so.”
Tonya: “Ok. First you’re right; the catheter will stay in your bladder, probably about 2 weeks. Your surgeon will have you come to the office to have it removed. We’ll talk about how you and your wife can manage the catheter, and we’ll probably recommend a visit by a home health nurse. I want to look at the dressing over your incision more closely. You have a small drain in the incision to make sure fluid drains and the tissues heal well. I want to talk with you and your wife about how to observe for signs of infection.”
Mr. Jacobs: “Is infection common?”
Tonya: “No, but you need to know the signs of an infection; so, if something happens once you return home, you can call your doctor quickly.”
Terminating the Interview
As in the other phases of the interview, termination requires skill. You summarize your discussion with the patient and check for accuracy of the information collected. Give your patient a clue that the interview is coming to an end. For example, say, “I have just two more questions. We’ll be finished in a few more minutes.” This helps the patient maintain direct attention without being distracted by wondering when the interview will end. This approach also gives the patient an opportunity to ask additional questions. End the interview in a friendly manner, telling the patient when you will return to provide care.
Tonya: “Thank you, Mr. Jacobs. I am just about finished with my questions. Can I get you anything?”
Mr. Jacobs: “No, I want to rest a bit.”
Tonya: You have given me a good idea of which topics we need to cover to prepare you for going home. And we’ll include your wife in these discussions. Pain control is our priority right now, and we can talk further about the medicines you’ll be taking when you go home. I want to go over catheter and dressing care after you rest so you feel prepared to go home. I also plan to come back and talk to you more about the surgery and its effects on your sexual function. Is there anything I can do for you now?”
Mr. Jacobs: “No, you’ve been helpful already.”
A skillful interviewer adapts interview strategies based on the patient’s responses. You successfully gather relevant health data when you are prepared for the interview and able to carry out each interview phase with minimal interruption.
Interview Techniques
How you conduct the interview is just as important as the questions you ask. Always use good communication techniques (see Chapter 24). During the interview you are responsible for directing the flow of the discussion so your patient has the opportunity to freely contribute stories about his or her health problems to enable you to get as much detailed information as possible. Some interviews are focused; others are comprehensive. Listen and consider the information shared because this helps you direct the patient to provide more detail or discuss a topic that might reveal a possible problem. Because a patient’s report includes subjective information, validate data from the interview later with objective data. For example, if the patient reports difficulty breathing, this will lead you to further assess respiratory rate and lung sounds during the physical examination.
During an interview obtain information (when appropriate) about a patient’s physical, developmental, emotional, intellectual, social, and spiritual dimensions. Physical and developmental information reflects normal functioning and reveals pathological changes caused by illness, trauma, or developmental crisis. Emotional information includes the patient’s behavioral responses to changes in health and patterns of living. Relevant emotional information includes mood, perceptions, body image, self-concept, and attitudes about sexuality. Intellectual information includes intellectual performance, problem-solving ability, educational level, communication patterns, and attention span. Social information involves environmental, cultural, ethnic, or social patterns that affect the present or future level of wellness. You also collect information about life goals and values and religious practices, part of a patient’s spirituality.
Observe the patient’s nonverbal communication such as use of eye contact, body language, or tone of voice. While observing a patient’s nonverbal behavior, appearance, and interaction with the environment, determine whether the data you obtain are consistent with what the patient states verbally. Your observations lead you to pursue further objective information to form accurate conclusions. Patients also obtain information during interviews. If you establish a trusting nurse-patient relationship, the patient feels comfortable asking you questions about the health care environment, planned treatments, diagnostic testing, and available resources. The patient needs this information to make decisions about goals and the plan of care.
Open-ended Questions
In a patient-centered interview you try to find out, in the patient’s own words, what the health problem is and its probable cause. Remember, patients are usually the best resources in talking about their symptoms or relating their health history. Begin by asking the patient an open-ended question to elicit his or her story (Box 16-3). An open-ended question does not presuppose a specific answer. For example, say, “So, why did you come to the hospital today?” or “Tell me about the problems you’re having.” The use of open-ended questions prompts patients to describe a situation in more than one or two words. This technique leads to a discussion in which patients actively describe their health status. The use of open-ended questions strengthens your relationship with a patient because it shows that you want to hear the patient’s thoughts and feelings. Remember to encourage and let the patient tell the entire story.