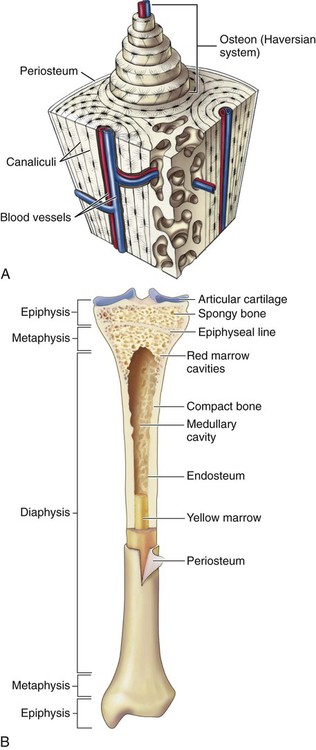
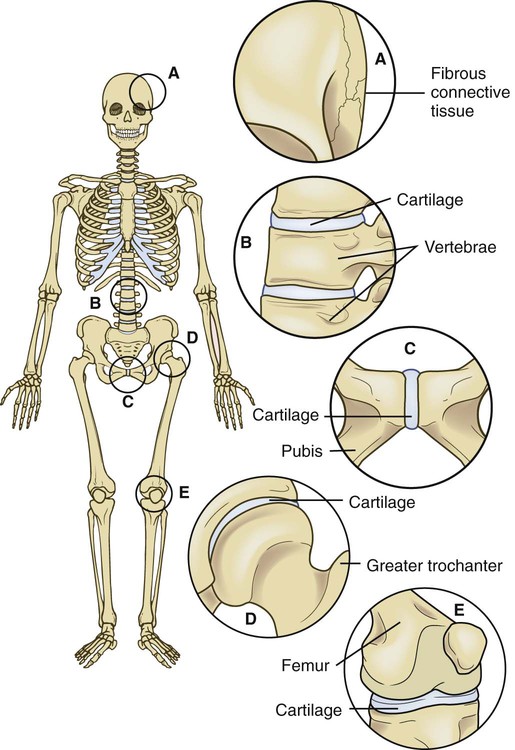
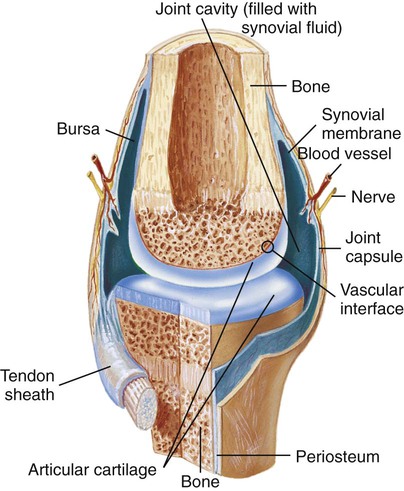
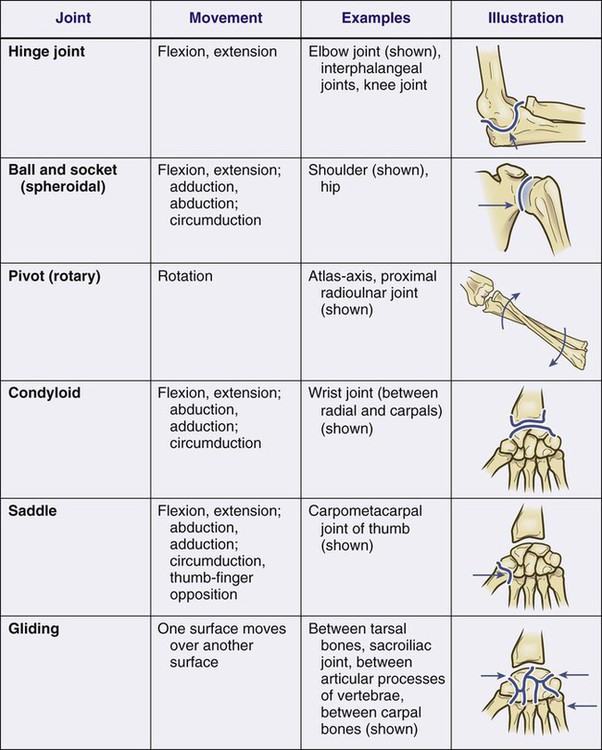
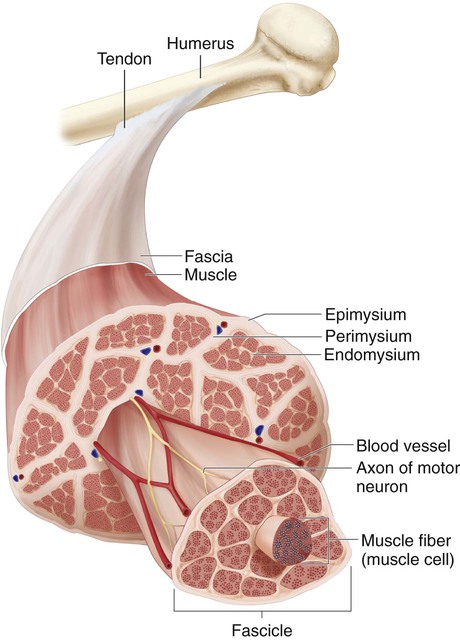
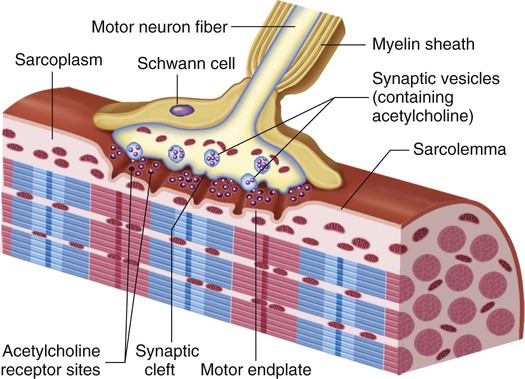
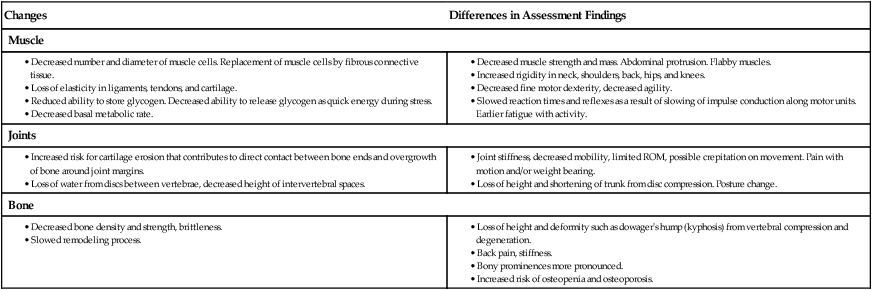
Chapter 62 1. Describe the gross anatomic and microscopic composition of bone. 2. Explain the classification system for joints and movements at synovial joints. 3. Compare and contrast the types and structure of muscle tissue. 4. Describe the functions of cartilage, muscles, ligaments, tendons, fascia, and bursae. 5. Link age-related changes in the musculoskeletal system to the differences in assessment findings. 6. Select significant subjective and objective data related to the musculoskeletal system that should be obtained from a patient. 7. Select appropriate techniques to use in the physical assessment of the musculoskeletal system. 8. Differentiate normal from abnormal findings of a physical assessment of the musculoskeletal system. 9. Describe the purpose, significance of results, and nursing responsibilities related to diagnostic studies of the musculoskeletal system. The main functions of bone are support, protection of internal organs, voluntary movement, blood cell production, and mineral storage.1 Bones provide the supporting framework that keeps the body from collapsing and also allows the body to bear weight. Bones also protect underlying vital organs and tissues. For example, the skull encloses the brain, the vertebrae surround the spinal cord, and the rib cage contains the lungs and heart. Bones serve as a point of attachment for muscles, which are connected to bones by tendons. Bones act as a lever for muscles, and movement occurs as a result of muscle contractions applied to these levers. Bones contain hematopoietic tissue for the production of red and white blood cells. Bones also serve as a site for storage of inorganic minerals such as calcium and phosphorus. Bone is classified according to structure as cortical (compact and dense) or cancellous (spongy). In cortical bone, cylindric structural units called osteons (Haversian systems) fit closely together, creating a dense bone structure (Fig. 62-1, A). Within the systems, the Haversian canals run parallel to the bone’s long axis and contain the blood vessels that travel to the bone’s interior from the periosteum. Surrounding each osteon are concentric rings known as lamellae, which characterize mature bone. Smaller canals (canaliculi) extend from the Haversian canals to the lacunae, where mature bone cells are embedded. The three types of bone cells are osteoblasts, osteocytes, and osteoclasts.2 Osteoblasts synthesize organic bone matrix (collagen) and are the basic bone-forming cells. Osteocytes are the mature bone cells. Osteoclasts participate in bone remodeling by assisting in the breakdown of bone tissue. Bone remodeling is the removal of old bone by osteoclasts (resorption) and the deposition of new bone by osteoblasts (ossification). The inner layer of bone is composed primarily of osteoblasts with a few osteoclasts. The anatomic structure of bone is best represented by a typical long bone such as the tibia (see Fig. 62-1, B). Each long bone consists of the epiphysis, diaphysis, and metaphysis. The epiphysis, the widened area found at each end of a long bone, is composed primarily of cancellous bone. The wide epiphysis allows for greater weight distribution and provides stability for the joint. The epiphysis is also the location of muscle attachment. Articular cartilage covers the ends of the epiphysis to provide a smooth surface for joint movement. The diaphysis is the main shaft of the bone. It provides structural support and is composed of compact bone. The tubular structure of the diaphysis allows it to more easily withstand bending and twisting forces. The metaphysis is the flared area between the epiphysis and the diaphysis. Like the epiphysis, it is composed of cancellous bone. The medullary (marrow) cavity is in the center of the diaphysis and contains either red or yellow bone marrow.3 In the growing child, red bone marrow is actively involved in blood cell production (hematopoiesis). In the adult, the medullary cavity of long bones contains yellow bone marrow, which is mainly adipose tissue. Yellow marrow is involved in hematopoiesis only in times of great blood cell need. In adults, red marrow is found mainly in the flat bones, such as the pelvis, skull, sternum, cranium, ribs, vertebrae, and scapulae, and in the cancellous (“spongy”) material at the epiphyseal ends of long bones such as the femur and the humerus. Long bones are characterized by a central shaft (diaphysis) and two widened ends (epiphyses) (see Fig. 62-1, B). Examples include the femur, humerus, and tibia. Short bones are composed of cancellous bone covered by a thin layer of compact bone. Examples include the carpals in the hand and the tarsals in the foot. A joint (articulation) is a place where the ends of two bones are in proximity and move in relation to each other. Joints are classified by the degree of movement that they allow (Fig. 62-2). The most common joint is the freely movable diarthrodial (synovial) type. Each joint is enclosed in a capsule of fibrous connective tissue, which joins the two bones together to form a cavity (Fig. 62-3). The capsule is lined by a synovial membrane, which secretes a thick synovial fluid to lubricate the joint, reduce friction, and allow opposing surfaces to slide smoothly over each other. The end of each bone is covered with articular (hyaline) cartilage. Supporting structures (e.g., ligaments, tendons) reinforce the joint capsule and provide limits and stability to joint movement. Types of diarthrodial joints are shown in Fig. 62-4. The skeletal muscle is enclosed by the epimysium, a continuous layer of deep fascia. The epimysium helps muscles slide over nearby structures. Connective tissue surrounding and extending into the muscle can be subdivided into fiber bundles, or fasciculi. These bundles are covered by perimysium and an innermost connective tissue layer called the endomysium that surrounds each fiber (Fig. 62-5). Skeletal muscle fibers require a nerve impulse to contract. A nerve fiber and the skeletal muscle fibers it stimulates are called a motor endplate. The junction between the axon of the nerve cell and the adjacent muscle cell is called the myoneural or neuromuscular junction (Fig. 62-6). Ligaments and tendons are both composed of dense, fibrous connective tissue that contains bundles of closely packed collagen fibers arranged in the same plane for additional strength. Tendons attach muscles to bones as an extension of the muscle sheath that adheres to the periosteum. Ligaments connect bones to bones (e.g., tibia to femur at knee joint). They have a higher elastic content than tendons.4 Ligaments provide stability while permitting controlled movement at the joint. Bursae are small sacs of connective tissue lined with synovial membrane and containing viscous synovial fluid. They are typically located at bony prominences or joints to relieve pressure and decrease friction between moving parts.5 For example, bursae are found between the patella and the skin (prepatellar bursae), between the olecranon process of the elbow and the skin (olecranon bursae), between the head of the humerus and the acromion process of the scapula (subacromial bursae), and between the greater trochanter of the proximal femur and the skin (trochanteric bursae). Bursitis is an inflammation of a bursa sac. The inflammation may be acute or chronic. The bone remodeling process is altered in the aging adult. Increased bone resorption and decreased bone formation cause a loss of bone density, contributing to the development of osteopenia and osteoporosis (see Chapter 64). Muscle mass and strength also decrease with aging. Almost 30% of muscle mass is lost by age 70. A loss of motor neurons can cause additional problems with skeletal muscle movement. Tendons and ligaments become less flexible, and movement becomes more rigid. Joints in the aging adult are also more likely to be affected by osteoarthritis6 (see Chapter 65). Perform a musculoskeletal assessment with a particular emphasis on exercise practices. Obtain information on the type of exercise performed, including frequency and warm-up activities. Determine the impact of age-related changes of the musculoskeletal system on the older adult’s functional status. Specifically inquire about changes in self-care habits and ability to be self-sufficient in the home environment. Identify any musculoskeletal changes that increase the patient’s risk for falls, and discuss fall prevention strategies. Functional limitations that are accepted by older adults as a normal part of aging can often be halted or reversed with appropriate preventive strategies (see Table 63-1). Diseases such as osteoarthritis and osteoporosis are not a normal part of growing older for many people. These metabolic bone diseases involve the deterioration of bone tissue (osteoporosis) and the destruction of cartilage (osteoarthritis). Carefully differentiate between expected changes and the effects of disease in the aging adult. Symptoms of disease can be treated in many cases, helping the older adult to return to a higher functional level. Age-related changes in the musculoskeletal system and differences in assessment findings are presented in Table 62-1. TABLE 62-1 GERONTOLOGIC ASSESSMENT DIFFERENCES Question the patient regarding prescription and over-the-counter drugs and herbal products and nutritional supplements (see the Complementary & Alternative Therapies box in Chapter 3 on p. 39). Obtain detailed information about each treatment, including its name, the dose and frequency, length of time it was taken, its effects, and any possible side effects. Inquire about the use of skeletal muscle relaxants, opioids, nonsteroidal antiinflammatory drugs, and systemic and topical corticosteroids. Question the patient who has taken antiinflammatory drugs about GI distress or signs of bleeding. In addition to drugs taken for treatment of a musculoskeletal problem, ask the patient about drugs that can have detrimental effects on this system. Some of these drugs and their potential side effects include antiseizure drugs (osteomalacia), phenothiazines (gait disturbances), corticosteroids (avascular necrosis, decreased bone and muscle mass), and potassium-depleting diuretics (muscle cramps and weakness). Question women about their menstrual history. Episodes of premenopausal amenorrhea can contribute to the development of osteoporosis.7 Ask postmenopausal women about their use of hormone therapy. Inquire about calcium and vitamin D supplements for both women and men. The use of functional health patterns assists in organizing the assessment data. Table 62-2 summarizes specific questions to ask in relation to functional health patterns. TABLE 62-2 HEALTH HISTORY
Nursing Assessment
Musculoskeletal System
Structures and Functions of Musculoskeletal System
Bone
Function.
Microscopic Structure.
Gross Structure.
Types.
Joints
Muscle
Structure.
Neuromuscular Junction.
Ligaments and Tendons
Bursae
Gerontologic Considerations
Effects of Aging on Musculoskeletal System
Musculoskeletal System
Assessment of Musculoskeletal System
Subjective Data
Important Health Information.
Medications.
Functional Health Patterns.
Musculoskeletal System