Nurse Staffing Ratios
Policy Options
Joanne Spetz
“The problems of the world cannot possibly be solved by skeptics or cynics whose horizons are limited by the obvious realities.”
—John F. Kennedy
The importance of nursing to the delivery of high-quality health care has been recognized since the inception of the practice of nursing. Various factors contribute to the quality of nursing care, including the expertise of nursing staff, availability of supportive personnel and other health professionals, good communication among the care team, and the nurse/patient ratio. The relative importance of each of these factors has been debated through the years, and it was not until the past decade that high-quality empirical research found consistent relationships between licensed nurse staffing and the quality of patient care (e.g., Needleman et al., 2002; Aiken et al., 2002; Lang et al., 2004; Kane et al., 2007; Unruh, 2008).
Concerns about the effects of changes in nurse staffing levels in the 1990s, combined with the increasing influence of nursing unions, resulted in the passage of California Assembly Bill (AB) 394 in 1999—the first comprehensive legislation in the United States to establish minimum staffing levels for registered nurses (RNs) and licensed vocational nurses (LVNs) working in hospitals. This bill required that the California Department of Health Services (DHS) establish the specific staffing ratios. These were announced in 2002 and implemented beginning in 2004. In May 2009, federal legislation was introduced in the Senate (S.1031) by Barbara Boxer (D-CA), largely based on California’s regulations. Since then, other states and the federal government have considered, and are considering, their own regulations for nurse staffing in hospitals.
The Context in Which Ratios were Implemented
Throughout the late 1990s and early 2000s, there was substantial debate about changes that occurred in hospital staffing in the 1990s and the effects of such changes on the quality of care (Wunderlich, Sloan, & Davis, 1996; Aiken, Sochalski, & Anderson, 1996; Spetz, 1998; Unruh and Fottler, 2006). In some states, legislators and regulatory agencies considered staffing requirements to increase the numbers of nurses and other health care personnel working in hospitals and other settings. In 1996, California’s DHS implemented regulations that require hospitals to use patient classification systems (PCSs) to measure the acuity of patients and determine nurse staffing needs for inpatient units on a shift-by-shift basis. These regulations augmented regulations implemented in the 1976-1977 fiscal year that required hospitals to staff a minimum of 1 licensed nurse per 2 patients in intensive and coronary care units.
The PCS requirements did not satisfy some nursing advocates, and the California Nurses Association (CNA) and the Service Employees International Union (SEIU) continued to press for fixed staffing ratios in both ballot propositions and legislation (Spetz, 2001). Nurse unions alleged that hospitals created PCSs to meet budget requirements rather than patient needs, and that compliance with PCSs was low (Spetz, et al., 2000). At the same time, there was widespread agreement that the fixed minimum staffing requirements that applied to intensive and coronary care units were successful in ensuring adequate nursing care.
As the 1990s ended, a shortage of RNs emerged, and concern about poor staffing in hospitals continued (Kilborn, 1999). It was in this environment that AB 394 was passed by the legislature. Previous Republican governors had vetoed similar legislation; union-friendly Democratic Governor Gray Davis signed AB 394 and satisfied the union efforts to pass minimum-ratio legislation. AB 394 charged the California DHS with determining specific unit-by-unit nurse/patient ratios (Table 53-1).
Regulations
The DHS launched an extensive effort to determine the new minimum nurse staffing ratios. At the time, there was relatively little research that linked nurse staffing to the quality of patient care (Spetz et al., 2000; Kravitz et al., 2002); moreover, none of the published studies identified an ideal staffing ratio for hospitals (Lang et al., 2004). The DHS received recommendations about the ratios from stakeholders. The California Hospital Association (CHA) proposed a ratio of 1 licensed nurse per 10 patients in medical-surgical units and somewhat richer ratios in other units. The CNA recommended a ratio of 1 licensed nurse per 3 patients in medical-surgical units and richer ratios in other units. The SEIU recommended a ratio of 1 licensed nurse per 4 patients in medical-surgical units, and also made recommendations for staffing ratios for other health care workers. To help develop proposed ratios, the DHS commissioned a study by researchers at the University of California, Davis (Kravitz et al., 2002).
The proposed ratios were between those recommended by the CHA and the unions, with a 1 : 6 ratio in medical-surgical units starting January 1, 2004, and a 1 : 5 ratio in medical-surgical units commencing in January 2005. Other units have richer minimum-ratio requirements, as presented in Table 53-1. These minimum ratios do not replace the requirement that hospitals staff according to a PCS; if a hospital’s PCS indicates that richer staffing is needed, the hospital should staff accordingly. However, the problems with the PCS requirements have not been remedied.
TABLE 53-1
California Minimum Licensed Nurse/Patient Ratios
| Type of Unit | Ratio in 2004 | Ratio in 2005 | Ratio in 2008 |
| Intensive or critical care | 1 : 2 | 1 : 2 | 1 : 2 |
| Neonatal intensive care | 1 : 2 | 1 : 2 | 1 : 2 |
| Operating room | 1 : 1 | 1 : 1 | 1 : 1 |
| Postanesthesia recovery | 1 : 2 | 1 : 2 | 1 : 2 |
| Labor and delivery | 1 : 2 | 1 : 2 | 1 : 2 |
| Antepartum | 1 : 4 | 1 : 4 | 1 : 4 |
| Postpartum couplets | 1 : 4 | 1 : 4 | 1 : 4 |
| Postpartum women only | 1 : 6 | 1 : 6 | 1 : 6 |
| Pediatrics | 1 : 4 | 1 : 4 | 1 : 4 |
| Emergency room | 1 : 4 | 1 : 4 | 1 : 4 |
| ICU patients in the ER | 1 : 2 | 1 : 2 | 1 : 2 |
| Trauma patients in the ER | 1 : 1 | 1 : 1 | 1 : 1 |
| Step-down | 1 : 4 | 1 : 4 | 1 : 3 |
| Telemetry | 1 : 5 | 1 : 5 | 1 : 4 |
| Medical-surgical | 1 : 6 | 1 : 5 | 1 : 5 |
| Other specialty care | 1 : 5 | 1 : 5 | 1 : 4 |
| Psychiatric | 1 : 6 | 1 : 6 | 1 : 6 |
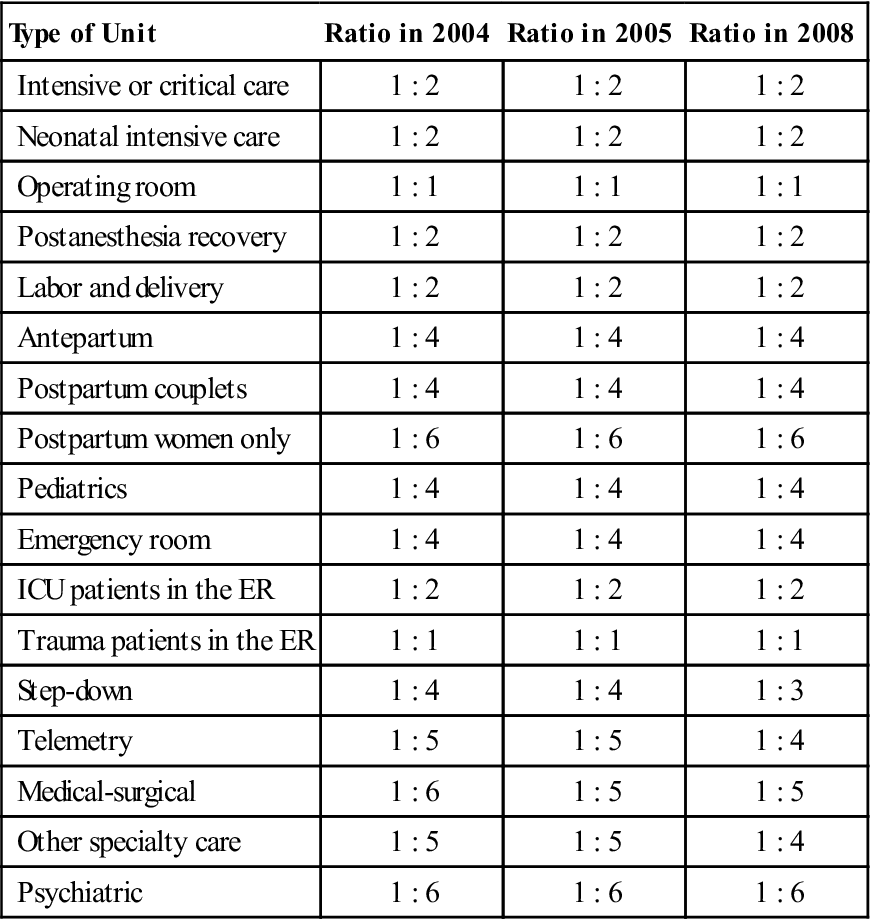
Sources: California Nurses Association. Retrieved from www.calnurses.org/nursing-practice/ratios/ratios_index.html; Spetz, J. (2004). California’s minimum nurse-to-patient ratios: The first few months. Journal of Nursing Administration, 34(12), 571-578.
What has Happened As a Result of the Ratios?
The implementation of California’s minimum nurse staffing ratio legislation has led to legal challenges and state government efforts to expand RN education. It also drove increases in hospital nurse staffing and wages in California. Whether the ratios have improved patient safety is still up for debate.
Legal Challenges
Two days before the ratios went into effect, the CHA filed a lawsuit arguing that the regulatory phrase “at all times” should not require that nursing coverage must comply any time a nurse leaves the work environment, such as during a break or restroom visit. The DHS contended that if the ratios were to have any meaning, they must be effective “at all times.” The judge hearing the case agreed with the DHS in a May 2004 ruling (Berestein, 2004). The second major legal challenge to the ratio regulations came from Governor Arnold Schwarzenegger, who sought to delay the implementation of the stricter 1-licensed nurse to 5-patient ratio scheduled for January 2005. The DHS stated that the severe shortage of licensed nurses made it overly onerous for hospitals to meet stricter staffing requirements and therefore issued an emergency regulation suspending the change 2 months before it was to have occurred. The DHS also proposed changes to the regulations for emergency departments (Rapaport, 2004).
The CNA filed suit against the DHS in December 2004, alleging that the emergency order had illegally bypassed the legislature (LaMar, 2005). In early March, a Superior Court judge tentatively ruled that the DHS indeed had not followed the law when issuing the emergency regulation (Salladay & Chong, 2005). After attempts by the governor’s administration to override and appeal the initial ruling, the judge’s decision was finalized in May 2005 (Benson, 2005a; Benson, 2005b; Gledhill, 2005). The denial of the emergency order to delay the enrichment of the ratios forced hospitals to scramble to meet the new requirements.
Expansion of Nursing Education
To assist hospitals in meeting the staffing ratio rules, both former Governor Davis and Governor Schwarzenegger dedicated funds to expanding nursing education and reducing attrition from nursing programs. The 2008 Annual Report reported that there had been a 54% increase in California RN graduates over the previous 4 years, and a 56% increase in nursing faculty (California Labor and Workforce Development Agency, 2009). In May 2009, it was announced that the Nurse Education Initiative would continue for a second round of 5-year grants, with an additional $60 million of Workforce Investment Act funds (Wasserman, 2009).
Enforcement Issues
The inspection and enforcement mechanisms of the DHS are relatively weak. The ability of the DHS to conduct inspections is hindered by ongoing state budget shortfalls. The DHS does not have the authority to impose fines or monetary penalties on hospitals that are found to violate the ratios, but instead requests and monitors plans submitted by hospitals to remedy the problem.
Other mechanisms exist to ensure that hospitals adhere to the ratios. First, government payers such as Medicare and Medi-Cal (the state Medicaid program) require that hospitals meet all state and federal regulations, and can deny payment to violators. Second, California’s cap on malpractice awards does not apply in cases of negligence, and it is possible that a hospital could be determined negligent if it consistently did not adhere to minimum nurse staffing regulations (Robertson, 2004). Third, unions draw public attention to hospitals that do not meet the staffing requirements, resulting in negative publicity for hospitals and increased scrutiny from DHS inspectors. Fourth, labor organizations that represent nurses, such as the CNA and the SEIU, have sought to incorporate staffing standards in their contract negotiations. Recent contractual agreements regarding nurse/patient ratios have come through standard contract negotiations (Gordon, 2005; Osterman, 2005).
Are Hospitals Meeting the Ratios?
Studies of all California hospitals using annual hospital financial data submitted to the California Office of Statewide Health Planning and Development (OSHPD) have found that annual average numbers of RN productive hours and nurse staffing ratios in medical-surgical units increased markedly between 2001 and 2006 (Conway et al., 2008; Cook et al., 2010; Spetz et al., 2009). Most recently, Spetz and colleagues (2009) found that statewide average RN hours per patient day increased 16.2% from 1999 through 2006, to an average of 6.9 hours per patient day. Interviews conducted with hospital leaders by a research team at UCSF revealed that many chief nursing officers and other managers said they hired nurses in order to meet the ratios, and most noted that it is challenging to adhere to the ratios at all times, including during scheduled breaks (Chapman et al., 2009).
Analyses of aggregated data such as those collected by the California Nursing Outcomes Coalition (CalNOC) or OSHPD can indicate general trends in nurse staffing, but cannot determine whether or not specific hospitals are compliant with the staffing ratios. Quarterly or annual data provide only an average number of productive nursing hours over the time period, which does not capture monthly, daily, or hourly variation in nurse staffing or patient census. A hospital might appear to be compliant on average by staffing more richly than required during the day and violating the ratios every night. CalNOC data are further limited because not all hospitals are represented, while OSHPD data are limited by not providing unit-by-unit data. Moreover, the OSHPD staffing data are not limited to nurses who work directly with patients. Researchers and policymakers will need to survey hospitals directly to fully understand how hospital staffing has changed on a shift-by-shift, unit-by-unit basis as a result of the minimum nurse/patient ratios.
Has the Mix of Staff Changed?
There has been concern about the possibility that hospitals eliminated support staff positions because of the minimum licensed nurse staffing requirements (Spetz, 2001). Anecdotal evidence suggests that this occurred among some hospitals. In 2003, the SEIU filed a grievance against Stanford University Medical Center when that hospital issued layoff notices to 113 nursing aides in advance of the implementation of the ratios. The hospital planned to replace those positions with RNs. The SEIU charged that the elimination of the nursing aide positions was contrary to the spirit of the minimum ratios (Ostrov, 2003). In a study conducted by UCSF, some hospital leaders reported that they had laid off ancillary staff to use their personnel budgets to hire more RNs (Chapman et al., 2009). CalNOC analyses of staffing data suggest that the substitution of licensed nurses for unlicensed staff may be widespread; the increase in RN staffing was much larger than the overall staffing increase among their hospitals (Donaldson et al., 2005; Bolton et al., 2007).
Have Hospitals Reduced Services?
The California Hospital Association warned that strict minimum nurse/patient ratio requirements will force hospitals to reduce their services. To maintain the minimum ratios, hospitals might reschedule procedures, close selected units and beds, or shut their doors entirely. These fears seemed warranted when in January 2004, it was announced that Santa Teresita Hospital in Duarte, California, was closing its 39-bed inpatient department and emergency room because of its inability to meet the minimum ratios (Chavez, 2004). However, newspapers subsequently reported that nurses who had worked at the hospital said they were meeting the ratios without difficulty (Allen, 2004), and an analysis of financial data reported by the hospital to OSHPD revealed that the hospital had been suffering severe financial distress for several years before it closed (Spetz, 2004). Given this information, it seems unlikely that the ratios were the primary reason for the hospital’s closure. Statewide, there have been few verified reports of the minimum nurse/patient ratios causing permanent closures of inpatient hospital units or beds. Whether there have been permanent, important effects on health or access to care for Californians is unknown.
Have Hospitals Suffered Financial Losses?
In November 2004, the DHS argued that catastrophic financial losses that would result from implementing more stringent ratios in 2005 justified the issuance of an emergency order to delay ratios. However, there is no empiric evidence that staffing ratios have negatively impacted hospitals’ financial status. Since 1999, hospitals have been financially buffeted by numerous factors, most notably changes in Medicare and Medicaid payment policy and requirements that hospital facilities meet seismic standards through retrofitting or new construction (Spetz et al., 2009). Average operating margins of California hospitals hovered between −2% and +2% from 1999 through 2006. Qualitative evidence published by the California HealthCare Foundation reported that hospital CEOs absorbed the costs of the ratios by reducing other budget areas, and some hospitals were able to obtain higher insurance reimbursement rates to cover additional staff expenses (Spetz et al., 2009). In an analysis of OSHPD hospital financial data, Cook and colleagues (2010) found no significant change in total annual labor costs for licensed nurses, total annual hospital costs, or hospital prices. Another study of California hospital data concluded that labor cost increases resulting from the nurse staffing ratios were not large enough to explain increases in hospital prices from 1999 through 2005 (Antwi, Gaynor, & Vogt, 2009).
Are Nurses More Satisfied?
Advocates of staffing ratio regulations link improved staffing to nurse satisfaction, and argue that greater nurse satisfaction will reduce nurse turnover and lead to better patient outcomes (Peter D. Hart Research Associates, 2003; Public Policy Associates, 2004; CNA, 2009). An analysis of nurse survey data collected for the California Board of Registered Nursing found that there were significant improvements in overall job satisfaction among hospital-employed RNs between 2004 and 2006 (Spetz, 2008). Nurse satisfaction also increased with respect to the adequacy of RN staff, time for patient education, benefits, and clerical support. However, these improvements in nurse satisfaction could not be directly linked to changes in nurse staffing at the hospital level or with regional changes in nurse staffing that may have resulted from the ratio regulations.
Other State and Federal Proposals
The only Federal regulation that directly referred to nurse staffing levels in hospitals at this writing is the 42 Code of Federal Regulations (42CFR 482.23[b]), which requires hospitals that participate in Medicare to have “adequate numbers of licensed registered nurses, licensed practical (vocational) nurses, and other personnel to provide nursing care to all patients as needed” (American Nurses Association, 2009). In 2009, Senator Barbara Boxer (D-CA) introduced S 1031, and Representative Janice Schakowsky (D-IL) introduced H.R. 2273, both of which would require that hospitals implement nurse-to-patient staffing plans and meet minimum RN nurse-to-patient ratios for specified patient care units. Hospitals that treat Medicare and Medicaid patients would be required to meet these requirements, and supplementary funding would be made available through Medicare to finance the cost of the additional nursing staff. These bills were referred to committees after introduction, and had not been voted upon by those committees by the end of 2009.
Some states have pursued their own staffing regulations, in part because there is limited regulation at the federal level. State regulations generally take one or more of three approaches: a requirement that hospitals develop and implement nurse staffing plans with input from direct care nurses; requiring public disclosure of staffing levels; and/or establishment of fixed minimum staffing ratios. California is the only state to have implemented a law using this third strategy, although similar legislation has been proposed in other states, and is currently under consideration in Illinois, Michigan, Nevada, New York, and Pennsylvania. Most of these bills have been developed or supported by affiliates of National Nurses United, which is a national RN union spearheaded by the California Nurses Association.
Some states have opted to develop staffing regulations that offer hospitals more flexibility than do fixed minimum staffing ratios. Oregon, Texas, Nevada, Ohio, Rhode Island, Connecticut, Washington, and Illinois have signed into law requirements that hospitals implement and enforce a written nurse staffing policy. In most of these states, the staffing policy must be developed by a committee that includes staff nurses. For example, the laws for Oregon, Texas, Nevada, Washington, Illinois, and Connecticut require that the committee be composed of at least 50% direct care nurses. These laws often specify that staffing committees take into account patient acuity, physical configuration of the unit, and other factors when developing staffing plans. Rhode Island requires that hospitals submit a “core staffing plan” to the state department of health annually, with specific staffing for each patient care unit and each shift (American Nurses Association, 2009). In 2009, several states were considering regulations to require that hospitals establish staffing plans, including Florida, Pennsylvania, and Massachusetts.
The third, and least binding, approach to nurse staffing regulation is to mandate reporting of staffing ratios to the public or to a regulatory agency. In New York, for example, facilities must make available to the public information about nurse staffing and patient outcomes. Specific adverse events, such as medication errors and decubitus ulcers, are considered reportable information under this law. Other states with public reporting requirements are Vermont and Illinois. New Jersey’s regulation mandates that hospitals post daily staffing information for each unit and shift, and also provide these data to state regulators, and in 2009 New York added a similar posting requirement to its regulations.
Issues That Need to be Addressed
Two issues central to the success of minimum nurse/patient ratios have not been addressed: Have the ratios improved the quality of patient care, and what was the total cost of the ratio regulations?
Did the Ratios Improve the Quality of Care?
Only a handful of published studies examine the effect of the minimum ratios on the quality of patient care. In the first paper published on this subject, the CalNOC analyzed rates of patient falls and hospital-acquired pressure ulcers between 2002 and 2004 in their sample of 68 hospitals and found that there was no statistically significant change that could be attributed to the ratios (Donaldson et al., 2005). A follow-up study of CalNOC data through 2006 confirmed these results, finding no improvement in rates of patient falls, prevalence of pressure ulcers, or prevalence of restraint use that could be associated with the implementation of staffing ratios (Bolton et al., 2007). Although these studies suggest that the ratios have not improved quality of care, there are several reasons these papers do not provide a definitive verdict on the ratios. First, as noted above, only a fraction of California hospitals was analyzed. Second, the outcomes examined might not be very sensitive to changes in licensed nurse staffing. Research studies that examine whether or not nurse staffing affects rates of hospital-acquired pressure ulcers and postoperative hip fractures (which would be caused by a patient fall) have produced mixed findings (Agency for Healthcare Research and Quality, 2005). Finally, these outcomes might be more sensitive to total staffing than to licensed nurse staffing. In this case, replacement of unlicensed staff with licensed nurses may have no net positive or negative effect.
Two recent studies echo the findings reported by the CalNOC researchers. Spetz and colleagues examined OSHPD patient discharge data for all non-federal, general acute care California hospitals from 1999 through 2006, and could not associate improvements in outcomes to the implementation of the ratios. The research team noted that many of the hospital leaders they interviewed expected that the staffing ratios would improve the quality of care, but few thought the ratios had met this expectation. In a more rigorous analysis of OSHPD data from 2001 to 2005, Cook and colleagues (2010) found no association between changes in nurse staffing and changes in pressure ulcer rates or failure to rescue a patient after a complication.
However, the newest study of the impact of the ratios on the work environment and quality of care finds improvements in nurse job satisfaction, burnout, and quality of care. Aiken and colleagues surveyed nearly 80,000 RNs in California, New Jersey, and Pennsylvania to learn their experiences with staffing, the work environment, and patient safety (Aiken et al., 2010). The survey data were linked to secondary data on patient outcomes collected by state government agencies. The researchers found that nurse workloads, measured as average patients per shift, were lower in California than in New Jersey and Pennsylvania, and that over 80% of California nurses reported that their assigned workloads were in compliance with the state’s regulation. They indicated that improvements in their patient assignments had been achieved by there being more relief nurses to cover breaks, more nurses floating to other units, and greater use of supplemental and agency nurses. They also reported less use of LVNs, unlicensed personnel, and non-nursing support services, suggesting that hospitals compensated for RN staffing increases by reducing staff in other areas.
Aiken and colleagues (2010) also reported that nurses were more satisfied with their working conditions. Nurses in California were significantly more likely to report that their workload was reasonable, allowed them to spend adequate time with patients, and that they were able to take breaks during the workday. Nurses with lower workloads were significantly less likely to report that they received complaints from families, faced verbal abuse, were burned out, were dissatisfied, felt quality of care was poor, or were looking for new jobs. Perhaps most importantly, Aiken and colleagues found that across all three states, higher nurse staffing levels were associated with lower rates of 30-day inpatient mortality and failure-to-rescue. These relationships were stronger in California than in other states.
The study by Aiken and colleagues (2010) is limited by its use of cross-sectional data. Research based on a single year of data cannot identify the effect of changes in policy or practice on changes in patient outcomes. While the responses of nurses regarding the patient safety environment suggest that the lower workloads in California are associated with more positive nurse perceptions of patient safety, these perceptions may not lead to true improvements in patient outcomes. And, the analysis of patient outcomes was limited to two outcomes; while these are arguably among the most important, other outcomes should be assessed in the future.
There is a pressing need for more research on the effects of minimum ratios on patient care. Researchers should examine a variety of patient outcomes and sources of data, using various statistical methods. As Cook and colleagues (2010) note, it is not possible with secondary data to easily determine whether or not a hospital reallocated resources so they could increase nurse staffing at the expense of other quality-improving processes. It also is possible that changes in patient outcomes due to the staffing ratios will occur over a longer period of time, and thus empiric research will not measure improvements in outcomes for several more years. Further confounding the research on the quality impact of staffing ratios is the fact that many health systems and hospitals have established quality improvement programs in response to increased public attention to medical errors and patient outcomes. As of 2010, there has been no statewide analysis of the impact of these other quality-improvement programs and how their efforts may have complimented or detracted from the impact of nurse staffing ratios.
What was the Cost of the Ratios?
Any positive impact of minimum staffing ratios should be weighed against the costs of the ratios. At this time, those costs have not been accurately quantified. Numerous studies indicate that hospitals hired more licensed nurses to meet the ratios, and one study reported that nurse wages rose substantially in California (Mark et al., 2009). However, no research has tied these facts to overall increases in hospital costs or declines in hospital operating margins. A careful accounting of the extent to which increases in nurse staffing were necessitated by the ratios, and the cost of such increases, is necessary. Moreover, it is important to quantify the value of other investments hospitals might have made if they were not required to adhere to the staffing ratios. A hospital may have delayed implementation of a new infection-control system that would have reduced infection rates; this “opportunity cost” should be included as part of the overall cost of the staffing regulations.
What Next?
Many states and the federal government are considering legislation to mandate minimum licensed nurse staffing ratios in hospitals (CNA, 2009). Even if these efforts fail, improvements in nurse staffing are likely to propagate across the United States. Recent research suggests that the ratio of cost per life saved associated with increasing nurse staffing is favorable as compared with many other health interventions (Rothberg et al., 2005), and thus hospitals are likely to turn toward improved nurse staffing as a way to meet quality goals at a reasonable price. However, even if more studies demonstrate that nurse staffing is a cost-effective means to producing better health, researchers need to examine the effectiveness of a minimum staffing mandate. If California’s regulation can be shown to have improved patient outcomes at an acceptable cost, it will be easy for other states to follow in California’s footsteps.
For a list of related websites, please refer to your Evolve Resources at http://evolve.elsevier.com/Mason/policypolitics/
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


