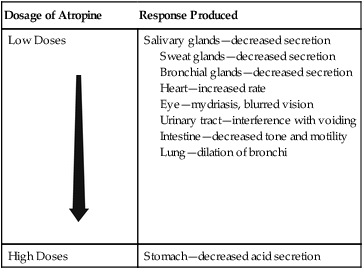
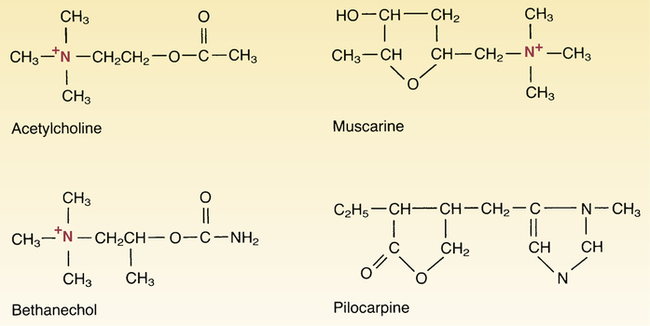
CHAPTER 14 The muscarinic agonists and antagonists produce their effects through direct interaction with muscarinic receptors. The muscarinic agonists cause receptor activation; the antagonists produce receptor blockade. Like the muscarinic agonists, another group of drugs—the cholinesterase inhibitors—can also cause receptor activation, but they do so by an indirect mechanism. These drugs are discussed separately in Chapter 15. Since atropine acts by causing muscarinic receptor blockade, its effects are opposite to those caused by muscarinic activation. Accordingly, we can readily predict the effects of atropine by knowing the normal responses to muscarinic receptor activation (see Table 13–2) and by knowing that atropine will reverse those responses. Like the muscarinic agonists, the muscarinic antagonists exert their influence primarily on the heart, exocrine glands, smooth muscles, and eye. It is important to note that not all muscarinic receptors are equally sensitive to blockade by atropine and most other anticholinergic drugs: At some sites, muscarinic receptors can be blocked with relatively low doses, whereas at other sites much higher doses are needed. Table 14–1 indicates the sequence in which specific muscarinic receptors are blocked as the dose of atropine is increased. TABLE 14–1 Relationship Between Dosage and Responses to Atropine Differences in receptor sensitivity to muscarinic blockers are of clinical significance. As indicated in Table 14–1, the doses needed to block muscarinic receptors in the stomach and bronchial smooth muscle are higher than the doses needed to block muscarinic receptors at all other locations. Accordingly, if we want to use atropine to treat peptic ulcer disease (by suppressing gastric acid secretion) or asthma (by dilating the bronchi), we cannot do so without also affecting the heart, exocrine glands, many smooth muscles, and the eye. Because of these obligatory side effects, atropine and most other muscarinic antagonists are not preferred drugs for treating peptic ulcers or asthma.
Muscarinic agonists and antagonists
Muscarinic agonists
Bethanechol
Muscarinic antagonists (anticholinergic drugs)
Atropine
Pharmacologic effects
Dose dependency of muscarinic blockade.

Dosage of Atropine
Response Produced
Low Doses

Salivary glands—decreased secretion
Sweat glands—decreased secretion
Bronchial glands—decreased secretion
Heart—increased rate
Eye—mydriasis, blurred vision
Urinary tract—interference with voiding
Intestine—decreased tone and motility
Lung—dilation of bronchi
High Doses
Stomach—decreased acid secretion