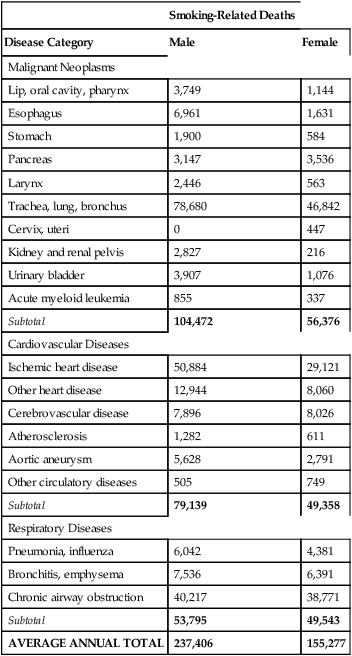
CHAPTER 39 Cigarette smoking remains the greatest single cause of preventable illness and premature death. In the United States, smoking kills more than 443,000 adults each year—about 1 of every 5 deaths. Around the world, tobacco kills over 5 million people each year. On average, male smokers die 13.2 years prematurely, and females die 14.5 years prematurely. As shown in Table 39–1, most deaths result from lung cancer (125,522), heart disease (101,009), and chronic airway obstruction (79,898). Not only do cigarettes kill people who smoke, every year, through secondhand smoke, cigarettes kill about 50,000 nonsmoking Americans, and about 600,000 nonsmokers worldwide. The direct medical costs of smoking exceed $95 billion a year. Indirect costs, including lost time from work and disability, add up to an additional $97 billion. In the United States, the prevalence of smoking among adults fell steadily from 1965 (42%) through the 1980s and 1990s, but has now leveled off, remaining constant between 2004 (20.9%) and 2008 (20.6%). TABLE 39–1 Average Annual Smoking-Attributable Mortality (United States, 2000–2004)* *Data are for adults ages 35 and older, and do not include deaths caused by burns or secondhand smoke. Data were obtained online at apps.nccd.cdc.gov/sammec/—the web site of the Centers for Disease Control and Prevention: Smoking-Attributable Mortality, Morbidity, and Economic Costs (SAMMEC). • Strengthen advertising restrictions, including the prohibition on marketing to youth. • Require revised and more prominent warning labels. • Require disclosure of all ingredients in tobacco products and restrict harmful additives. • Monitor nicotine yields, and mandate gradual nicotine reduction to nonaddictive levels. Nicotine exposure during gestation can harm the fetus, and nicotine in breast milk can harm the nursing infant. Nonetheless, as discussed in Box 39–1, since pharmaceutical nicotine is safer than tobacco smoke, it is reasonable to consider using nicotine therapy during pregnancy to help a woman quit smoking. According to a 2004 report from the U.S. Surgeon General, the adverse consequences of smoking are more extensive than previously understood. It is now clear that chronic smoking can injure nearly every organ of the body. We already knew that smoking could cause cardiovascular disease, chronic lung disease, and cancers of the larynx, lung, esophagus, oral cavity, and bladder. New additions to the list include leukemia, cataracts, pneumonia, periodontal disease, type 2 diabetes, abdominal aortic aneurysm, and cancers of the cervix, kidney, pancreas, and stomach. Smoking during pregnancy increases the risk of low birth weight, preterm labor, stillbirth, miscarriage, spontaneous abortion, perinatal mortality, and sudden infant death. As shown in Table 39–1, the leading causes of smoking-related death are lung cancer, ischemic heart disease, and chronic airway obstruction.
Drug abuse III: nicotine and smoking

Smoking-Related Deaths
Disease Category
Male
Female
Malignant Neoplasms
Lip, oral cavity, pharynx
3,749
1,144
Esophagus
6,961
1,631
Stomach
1,900
584
Pancreas
3,147
3,536
Larynx
2,446
563
Trachea, lung, bronchus
78,680
46,842
Cervix, uteri
0
447
Kidney and renal pelvis
2,827
216
Urinary bladder
3,907
1,076
Acute myeloid leukemia
855
337
Subtotal
104,472
56,376
Cardiovascular Diseases
Ischemic heart disease
50,884
29,121
Other heart disease
12,944
8,060
Cerebrovascular disease
7,896
8,026
Atherosclerosis
1,282
611
Aortic aneurysm
5,628
2,791
Other circulatory diseases
505
749
Subtotal
79,139
49,358
Respiratory Diseases
Pneumonia, influenza
6,042
4,381
Bronchitis, emphysema
7,536
6,391
Chronic airway obstruction
40,217
38,771
Subtotal
53,795
49,543
AVERAGE ANNUAL TOTAL
237,406
155,277
Basic pharmacology of nicotine
Pharmacologic effects
Effects during pregnancy and lactation.
Chronic toxicity from smoking
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Drug abuse III: nicotine and smoking
Only gold members can continue reading. Log In or Register to continue
Get Clinical Tree app for offline access

