Mobility and Immobility
Objectives
• Discuss physiological and pathological influences on body alignment and joint mobility.
• Identify changes in physiological and psychosocial function associated with mobility and immobility.
• Assess for correct and impaired body alignment and mobility.
• Formulate appropriate nursing diagnoses for impaired body alignment and mobility.
• Develop individualized nursing care plans for patients with impaired body alignment and mobility.
• Discuss the importance of no-lift policies for the patient and health care provider.
• Describe equipment needed for safe patient handling and movement.
• Compare and contrast active and passive range-of-motion exercises.
• Evaluate the nursing plan for maintaining body alignment and mobility.
Key Terms
Activity tolerance, p. 1139
Anthropometric measurements, p. 1141
Atelectasis, p. 1133
Bed rest, p. 1132
Body alignment, p. 1128
Body mechanics, p. 1127
Chest physiotherapy (CPT), p. 1148
Concentric tension, p. 1129
Disuse osteoporosis, p. 1134
Eccentric tension, p. 1130
Embolus, p. 1142
Exercise, p. 1139
Footdrop, p. 1134
Friction, p. 1128
Gait, p. 1139
Gait belt, p. 1158
Hemiparesis, p. 1158
Hemiplegia, p. 1158
Hypostatic pneumonia, p. 1133
Immobility, p. 1132
Instrumental activities of daily living (IADLs), p. 1157
Isometric contraction, p. 1130
Isotonic contraction, p. 1130
Joint contracture, p. 1134
Leverage, p. 1130
Logroll, p. 1165
Mobility, p. 1127
Muscle atrophy, p. 1131
Muscle tone, p. 1130
Negative nitrogen balance, p. 1132
Orthostatic hypotension, p. 1133
Osteoporosis, p. 1134
Pathological fractures, p. 1128
Posture, p. 1130
Pressure ulcer, p. 1135
Range of motion (ROM), p. 1136
Renal calculi, p. 1134
Shear, p. 1128
Thrombus, p. 1133
Trapeze bar, p. 1153
Trochanter roll, p. 1152
Unossified, p. 1129
Urinary stasis, p. 1134
![]()
People use mobility for many purposes (e.g., expression of emotions or satisfaction of basic needs with nonverbal gestures). It is also used to show self-defense, perform activities of daily living (ADLs), and participate in recreational activities. Many functions of the body depend on mobility. Intact musculoskeletal and nervous systems are necessary for optimal physical mobility and functioning.
Clinical nursing practice related to mobility and immobility requires the incorporation of scientific and nursing knowledge and skills to provide competent care. Knowing the movements and functions of muscles in maintaining posture and movement and implementing evidence-based knowledge about safe patient handling are essential to protecting the safety of both the patient and the nurse.
Scientific Knowledge Base
Nature of Movement
Movement is a complex process that requires coordination between the musculoskeletal and nervous systems. Body mechanics is a term used to describe the coordinated efforts of the musculoskeletal and nervous systems. Although nurses need to understand the physics surrounding body mechanics, lifting techniques historically used in nursing practice that emphasize body mechanics often cause debilitating injuries to nursing and other health care staff (de Castro et al., 2006). Today nurses use information about body alignment, balance, gravity, and friction when implementing nursing interventions such as positioning patients, determining the risk of patient falls, and selecting the safest way to move or transfer patients.
Alignment and Balance
The terms body alignment and posture are similar and refer to the positioning of the joints, tendons, ligaments, and muscles while standing, sitting, and lying. Body alignment means that the individual’s center of gravity is stable. Correct body alignment reduces strain on musculoskeletal structures, aids in maintaining adequate muscle tone, promotes comfort, and contributes to balance and conservation of energy. Without balance control the center of gravity is displaced, thus creating a risk for falls and subsequent injuries. Balance is enhanced by keeping the center of gravity of the body low with a wide base of support and maintaining correct body posture.
Individuals require balance for maintaining a static position (e.g., sitting) and moving (e.g., walking). Disease, injury, pain, physical development (e.g., age), and life changes (e.g., pregnancy) compromise the ability to remain balanced. Medications that cause dizziness and prolonged immobility also affect balance. Impaired balance is a major threat to physical safety and contributes to a fear of falling and self-imposed restrictions on activity.
Gravity and Friction
Weight is the force exerted on a body by gravity. The force of weight is always directed downward, which is why an unbalanced object falls. Unsteady patients fall if their center of gravity becomes unbalanced because of the gravitational pull on their weight.
To lift safely the lifter has to overcome the weight of the object and know its center of gravity. In symmetrical inanimate objects the center of gravity is at the exact center of the object. However, people are not geometrically perfect; their centers of gravity are usually at 55% to 57% of standing height and are in the midline, which is why only using principles of body mechanics in lifting patients often leads to injury of the nurse or health care professional.
Friction is a force that occurs in a direction to oppose movement. The greater the surface area of the object that is moved, the greater the friction. A larger object produces greater resistance to movement. In addition, the force exerted against the skin while the skin remains stationary and the bony structures move is called shear. Unfortunately a common example is when the head of the bed is elevated beyond 60 degrees and gravity pulls the bony skeleton toward the foot of the bed while the skin remains against the sheets. The blood vessels in the underlying tissue are stretched and damaged, resulting in impeded blood flow to the deep tissues. Ultimately pressure ulcers often develop within the undermined tissue; the surface tissue appears less affected. To decrease surface area and reduce friction when patients are unable to assist with moving up in bed, nurses use an ergonomic assistive device such as a full body sling. This sling mechanically lifts the patient off the surface of the bed, thereby preventing friction, tearing, or shearing his or her delicate skin, and protects the nurse and other staff from injury (Nelson et al., 2009).
Physiology and Regulation of Movement
Skeletal System
The skeleton provides attachments for muscles and ligaments and the leverage necessary for movement. Thus the skeleton is the supporting framework of the body and is made up of four types of bones: long, short, flat, and irregular. Long bones contribute to height (e.g., the femur, fibula, and tibia in the leg) and length (e.g., the phalanges of the fingers and toes). Short bones (e.g., the carpal bones in the foot and the patella in the knee) occur in clusters and, when combined with ligaments and cartilage, permit movement of the extremities. Flat bones (e.g., some bones in the skull and the ribs in the thorax) provide structural contour. Irregular bones make up the vertebral column and some bones of the skull such as the mandible.
Bones are further characterized by firmness, rigidity, and elasticity. Firmness results from inorganic salts such as calcium and phosphate that are in the bone matrix. It is related to the rigidity of the bone, which is necessary to keep long bones straight and enables bones to withstand weight bearing. In addition, bones have a degree of elasticity and skeletal flexibility that change with age. For example, the newborn has a large amount of cartilage and is highly flexible but is unable to support weight. The toddler’s bones are more pliable than those of an older person and are better able to withstand falls. Older adults, especially women, are more susceptible to bone loss (resorption) and osteoporosis, which increase the risk of fractures.
The skeletal system has several functions. It protects vital organs (e.g., the skull around the brain and the ribs around the heart and lungs) and aids in calcium regulation. Bones store calcium and release it into the circulation as needed. Patients with decreased calcium regulation and metabolism are at risk for developing osteoporosis and pathological fractures (fractures caused by weakened bone tissue). In addition, the internal structure of long bones contains bone marrow, participates in red blood cell (RBC) production, and acts as a reservoir for blood. Patients with altered bone marrow function or diminished RBC production fatigue easily because of reduced hemoglobin and oxygen-carrying ability. This fatigue decreases their mobility and increases the risk for falling.
Joints
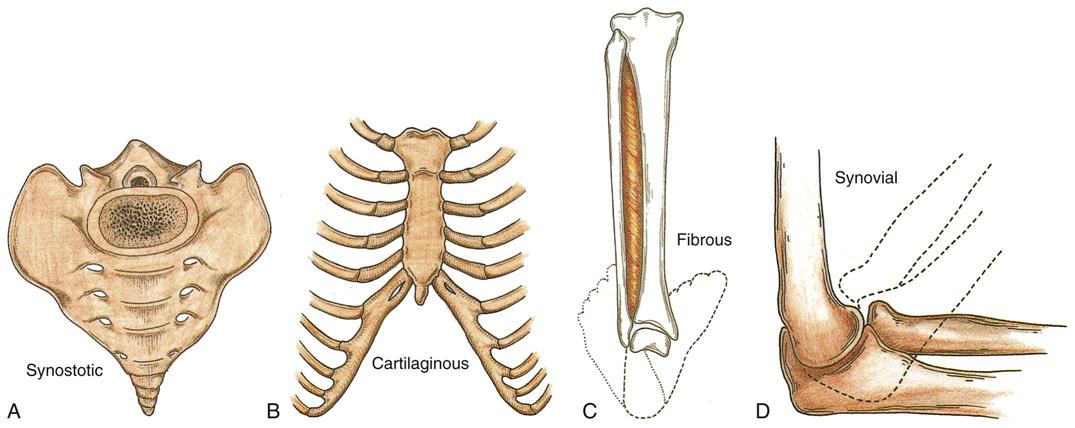
Joints are the connections between bones. Each joint is classified according to its structure and degree of mobility. There are four classifications of joints: synostotic, cartilaginous, fibrous, and synovial.
The synostotic joint refers to bones jointed by bones. No movement is associated with this type of joint, and the bony tissue that forms between the bones provides strength and stability. The classic example of this type of joint is the skull, where fusion of the joint occurs later in life (Fig. 47-1, A).
In the cartilaginous joint, or synchondrosis joint, cartilage unites bony components. This type of joint allows for bone growth while providing stability. When bone growth is complete, the joints ossify. The first sternocostal joint is an example of a synchondrosis joint (Fig. 47-1, B).
The fibrous joint, or syndesmosis joint, is a joint in which a ligament or membrane unites two bony surfaces. The fibers of ligaments are flexible and stretch, permitting a limited amount of movement. The paired bones of the lower leg (tibia and fibula) are syndesmotic joints (Huether and McCance, 2008) (Fig. 47-1, C).
The synovial joint, or true joint, is a freely movable joint in which contiguous bony surfaces are covered by articular cartilage and connected by ligaments lined with a synovial membrane. Joining of the humeral radius and ulna by cartilage and ligaments forms a pivotal joint (Fig. 47-1, D). Other types of synovial joints are the ball-and-socket joints such as the hip joint and the hinge joints such as the interphalangeal joints of the fingers.
Ligaments
Ligaments are white, shiny, flexible bands of fibrous tissue binding joints together and connecting bones and cartilages. Ligaments are elastic and aid joint flexibility and support (Fig. 47-2). In addition, some ligaments have a protective function. For example, ligaments between the vertebral bodies and the ligamentum flavum prevent damage to the spinal cord during movement of the back.
Tendons
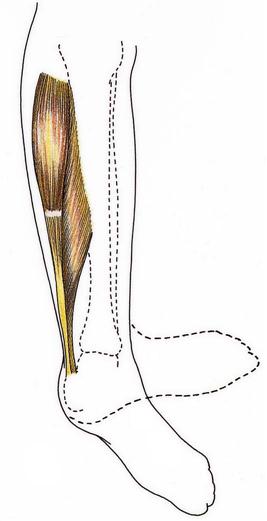
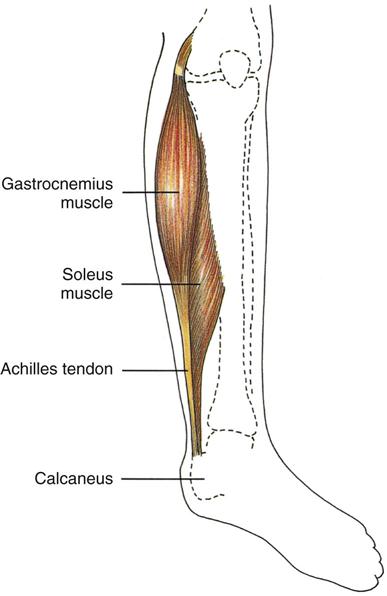
Tendons are white, glistening, fibrous bands of tissue that connect muscle to bone. They are strong, flexible, and inelastic; and they occur in various lengths and thicknesses. The Achilles tendon (tendo calcaneus) is the thickest and strongest tendon in the body. It begins near the midposterior of the leg and attaches the gastrocnemius and soleus muscles in the calf to the calcaneal bone in the back of the foot (Fig. 47-3).
Cartilage
Cartilage is nonvascular (without blood vessels) supporting connective tissue located chiefly in the joints and thorax, trachea, larynx, nose, and ear. The fetus has a large amount of temporary cartilage, which is replaced by bone developed during infancy. Permanent cartilage is unossified (not hardened), except in advanced age and diseases such as osteoarthritis.
Joints, ligaments, tendons, and cartilage facilitate strength and flexibility of the skeleton. Strength enables the skeletal system to support the body. A person’s flexibility is demonstrated through range of motion (ROM). However, strength and flexibility do not result entirely from these four structures. Adequate skeletal muscle is also necessary.
Skeletal Muscle
Movement of bones and joints involves active processes that are carefully integrated to achieve coordination. Skeletal muscles, because of their ability to contract and relax, are the working elements of movement. Anatomical structure and attachment to the skeleton enhance contractile elements of the skeletal muscle.
Muscles are made of fibers that contract when stimulated by an electrochemical impulse that travels from the nerve to the muscle across the neuromuscular junction. The electrochemical impulse causes the filaments (predominantly protein molecules of myosin and actin) within the fiber to slide past one another, with the filaments changing length.
Muscle contractions are categorized by functional purpose: moving, resisting, or stabilizing body parts. In concentric tension increased muscle contraction causes muscle shortening, resulting in movement such as when a patient uses an overhead trapeze to pull up in bed. Eccentric tension helps control the speed and direction of movement. For example, when using an overhead trapeze, the patient slowly lowers himself to the bed. The lowering is controlled when the antagonistic muscles lengthen. Concentric and eccentric muscle actions are necessary for active movement and therefore are referred to as dynamic or isotonic contraction. Isometric contraction (static contraction) causes an increase in muscle tension or muscle work but no shortening or active movement of the muscle (e.g., instructing the patient to tighten and relax a muscle group, as in quadriceps set exercises or pelvic floor exercises). Voluntary movement is a combination of isotonic and isometric contractions.
Although isometric contractions do not result in muscle shortening, energy expenditure increases. This type of muscle work is comparable to having a car in neutral with the driver continually depressing the accelerator and racing the engine. The driver is not going anywhere but expends a large amount of energy. It is important to understand the energy expenditure (increased respiratory rate and increased work on the heart) associated with isometric exercises because the exercises are sometimes contraindicated in certain patients’ illnesses (e.g., myocardial infarction or chronic obstructive pulmonary disease).
Muscle Movement and Posture
Muscles that attach to bones of leverage provide necessary strength to move an object. Leverage is an inducing or compelling force and occurs when specific bones such as the humerus, ulna, and radius and the associated joint such as the elbow act together as a lever. Force is applied to one end of the bone to lift a weight as another point rotates the bone in the opposite direction.
Muscles associated primarily with maintaining posture are short and featherlike in appearance because they converge obliquely at a common tendon. Muscles of the lower extremities, trunk, neck, and back are concerned primarily with posture (the position of the body in relation to the surrounding space). These muscle groups work together to stabilize and support body weight, and they allow an individual to maintain a sitting or standing posture.
Muscle Regulation of Posture and Movement
Posture and movement depend on the skeleton and the shape and development of skeletal muscles. They also contribute to musculoskeletal function and often reflect personality, discomfort, and mood. For example, a person with a dramatic personality gestures with the hands, a person who is fatigued or depressed may slouch, and a person with abdominal pain may curl into a fetal-like position.
Coordination and regulation of different muscle groups depend on muscle tone and activity of antagonistic, synergistic, and antigravity muscles (see Chapter 38). Muscle tone, or tonus, is the normal state of balanced muscle tension. The body achieves tension by alternating contraction and relaxation without active movement of neighboring fibers of a specific muscle group. Muscle tone helps maintain functional positions such as sitting or standing without excess muscle fatigue and is maintained through continual use of muscles. ADLs require muscle action and help maintain muscle tone. When a patient is immobile or on prolonged bed rest, activity level, activity tolerance, and muscle tone decrease.
Nervous System
The nervous system regulates movement and posture. The precentral gyrus, or motor strip, is the major voluntary motor area and is in the cerebral cortex. A majority of motor fibers descend from the motor strip and cross at the level of the medulla. Thus the motor fibers from the right motor strip initiate voluntary movement for the left side of the body, and motor fibers from the left motor strip initiate voluntary movement for the right side of the body.
During voluntary movement impulses descend from the motor strip to the spinal cord. An impulse exits the spinal cord through efferent motor nerves and travels through the nerves. Through a complex process neurotransmitters, or chemicals such as acetylcholine, transfer electric impulses from the nerve across the neuromuscular junction to the muscle. The neurotransmitter reaches a muscle and stimulates it, causing movement. Movement is impaired by disorders that alter neurotransmitter production, transfer of impulses from the nerve to the muscle, or activation of muscle activity. Parkinsonism is an example of such a disorder (see Chapter 38).
Pathological Influences on Mobility
Many pathological conditions affect mobility. Although a complete description of each is beyond the scope of this chapter, an overview of four pathological influences are presented.
Postural Abnormalities
Congenital or acquired postural abnormalities affect the efficiency of the musculoskeletal system and body alignment, balance, and appearance. During assessment observe body alignment and ROM (see Chapter 38). Postural abnormalities can cause pain, impair alignment or mobility, or both. Knowledge about the characteristics, causes, and treatment of common postural abnormalities is necessary for lifting, transfer, and positioning (Table 47-1). Some postural abnormalities limit ROM. Nurses intervene to maintain maximum ROM in unaffected joints and then design interventions to strengthen affected muscles and joints, improve the patient’s posture, and adequately use affected and unaffected muscle groups. Referral to and/or collaboration with a physical therapist enhances the nurse’s interventions for a patient with a postural abnormality.
TABLE 47-1
| ABNORMALITY | DESCRIPTION | CAUSE | POSSIBLE TREATMENTS* |
| Torticollis | Inclining of head to affected side, in which sternocleidomastoid muscle is contracted | Congenital or acquired condition | Surgery, heat, support, or immobilization, depending on cause and severity, gentle ROM |
| Lordosis | Exaggeration of anterior convex curve of lumbar spine | Congenital condition Temporary condition (e.g., pregnancy) | Spine-stretching exercises (based on cause) |
| Kyphosis | Increased convexity in curvature of thoracic spine | Congenital condition Rickets, osteoporosis Tuberculosis of spine | Spine-stretching exercises, sleeping without pillows, using bed board, bracing, spinal fusion (based on cause and severity) |
| Scoliosis | Lateral “S”- or “C”-shaped spinal column with vertebral rotation, unequal heights of hips and shoulders | Sometimes a consequence of numerous congenital, connective tissue and neuromuscular disorders | Approximately half of children with scoliosis require surgery Nonsurgical treatment is with braces and exercises |
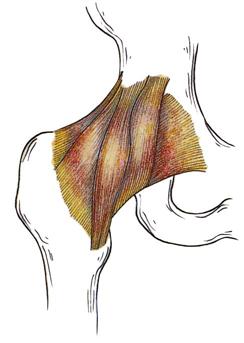
| Congenital hip dysplasia | Hip instability with limited abduction of hips and occasionally adduction contractures (head of femur does not articulate with acetabulum because of abnormal shallowness of acetabulum) | Congenital condition (more common with breech deliveries) | Maintenance of continuous abduction of thigh so head of femur presses into center of acetabulum Abduction splints, casting, surgery |
| Knock-knee (genu valgum) | Legs curved inward so knees come together as person walks | Congenital condition Rickets | Knee braces, surgery if not corrected by growth |
| Bowlegs (genu varum) | One or both legs bent outward at knee, which is normal until 2 to 3 years of age | Congenital condition Rickets | Slowing rate of curving if not corrected by growth With rickets, increase of vitamin D, calcium, and phosphorus intake to normal ranges |
| Clubfoot | 95%: Medial deviation and plantar flexion of foot (equinovarus) 5%: Lateral deviation and dorsiflexion (calcaneovalgus) | Congenital condition | Casts, splints such as Denis Browne splint, and surgery (based on degree and rigidity of deformity) |
| Footdrop | Inability to dorsiflex and invert foot because of peroneal nerve damage | Congenital condition Trauma Improper position of immobilized patient | None (cannot be corrected) Prevention through physical therapy Bracing with ankle-foot orthotic (AFO) |
| Pigeon toes | Internal rotation of forefoot or entire foot, common in infants | Congenital condition Habit | Growth, wearing reversed shoes |
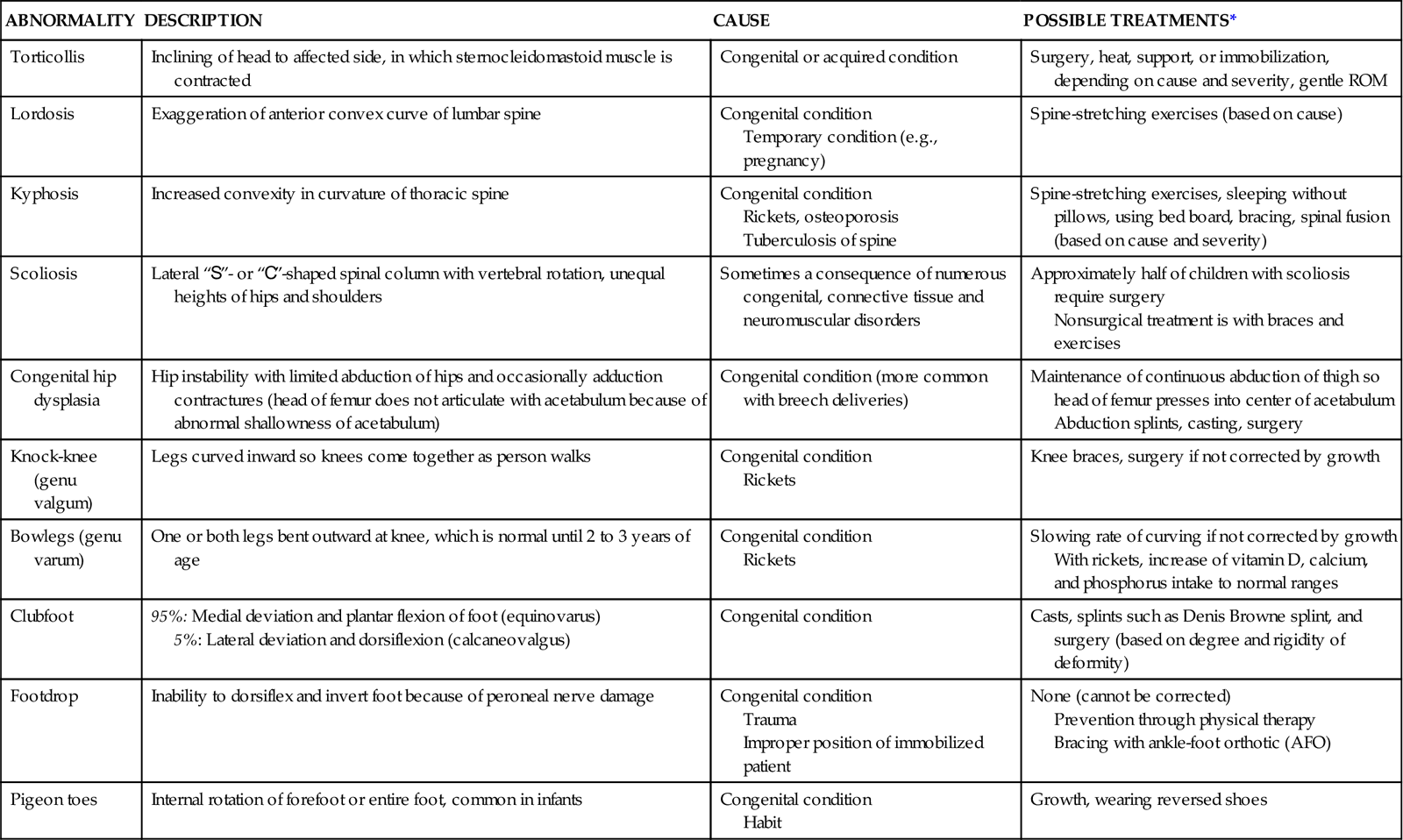
*Severity of condition and cause dictate treatment, which is individualized to the patient’s needs.
Data from McCance K, Huether SE: Pathophysiology: the biologic basis for disease in adults and children, ed 6, St Louis, 2009, Mosby.
Muscle Abnormalities
Injury and disease lead to numerous alterations in musculoskeletal function. For example, the muscular dystrophies are a group of familial disorders that cause degeneration of skeletal muscle fibers. They are the most prevalent of the muscle diseases in childhood. Patients with muscular dystrophy experience progressive, symmetrical weakness and wasting of skeletal muscle groups, with increasing disability and deformity (McCance and Huether, 2009).
Damage to the Central Nervous System
Damage to any component of the central nervous system that regulates voluntary movement results in impaired body alignment, balance, and mobility. Trauma from a head injury, ischemia from a stroke or brain attack (cerebrovascular accident [CVA]), or bacterial infection such as meningitis can damage the cerebellum or the motor strip in the cerebral cortex. Damage to the cerebellum causes problems with balance, and motor impairment is directly related to the amount of destruction of the motor strip. For example, a person with a right-sided cerebral hemorrhage with necrosis has destruction of the right motor strip that results in left-sided hemiplegia. Trauma to the spinal cord also impairs mobility. For example, a complete transection of the spinal cord results in a bilateral loss of voluntary motor control below the level of the trauma because motor fibers are cut.
Direct Trauma to the Musculoskeletal System
Direct trauma to the musculoskeletal system results in bruises, contusions, sprains, and fractures. A fracture is a disruption of bone tissue continuity. Fractures most commonly result from direct external trauma, but they also occur as a consequence of some deformity of the bone (e.g., pathological fractures of osteoporosis, Paget’s disease, or osteogenesis imperfecta). Young children are usually able to form new bone more easily than adults and, as a result, have few complications after a fracture. Treatment often includes positioning the fractured bone in proper alignment and immobilizing it to promote healing and restore function. Even this temporary immobilization results in some muscle atrophy, loss of muscle tone, and joint stiffness.
Nursing Knowledge Base
Fully understanding movement and mobility requires more than an overview of movement and the physiology and regulation of movement by the musculoskeletal and nervous systems. You need to know how to apply these scientific principles in the clinical setting to determine the safest way to move patients and to understand the effect of immobility on the physiological, psychosocial, and developmental aspects of patient care.
Safe Patient Handling
Nurses are exposed to the hazards related to lifting and transferring patients in many settings such as inpatient nursing units, long-term care facilities, and the operating room (de Castro et al., 2006). Manually lifting and transferring patients contributes to the high incidence of work-related musculoskeletal problems and back injuries in nurses and other health care staff (Nelson and Baptiste, 2006). Current evidence shows that many nurses frequently transfer to different positions and leave the profession because of work-related injuries (de Castro et al., 2006). Implementing evidence-based interventions and programs (e.g., lift teams) reduces the number of work-related injuries, which improves the health of the nurse and reduces indirect costs to the health care agency (e.g., workers’ compensation and replacing injured workers).
Today many states have laws that mandate safe patient handling in health care agencies. Health care agencies are implementing comprehensive safe patient–handling programs in all parts of the United States. Comprehensive safe patient–handling programs include the following elements: an ergonomics assessment protocol for health care environments, patient assessment criteria, algorithms for patient handling and movement, special equipment kept in convenient locations to help transfer patients, back injury resource nurses, an “after-action review” that allows the health care team to apply knowledge about moving patients safely in different settings, and a no-lift policy (Nelson, 2006).
Factors Influencing Mobility-Immobility
To determine how to move patients safely, assess their ability to move. Mobility refers to a person’s ability to move about freely, and immobility refers to the inability to do so. Some patients can be mobile or immobile, whereas others experience varying degrees of partial immobility. Think of mobility as a continuum, with mobility on one end, immobility on the other, and varying degrees of partial immobility between the end points. Some patients move back and forth between mobility and immobility, but for others immobility is absolute and continues indefinitely. The terms bed rest and impaired physical mobility are used frequently when discussing patients on the mobility-immobility continuum.
Bed rest is an intervention that restricts patients to bed for therapeutic reasons. Nurses and health care providers most often prescribe this intervention. Bed rest has many different interpretations among health care professionals. Patients with a wide variety of conditions are placed on bed rest. The duration of bed rest depends on the illness or injury and the patient’s prior state of health.
The effects of muscular deconditioning associated with lack of physical activity are often apparent in a matter of days. This cluster of symptoms is often referred to as the “hazards of immobility.” The individual of average weight and height without a chronic illness on bed rest loses muscle strength from baseline levels at a rate of 3% a day. Immobility also is associated with cardiovascular, skeletal, and other organ changes. The term disuse atrophy describes the tendency of cells and tissue to reduce in size and function in response to prolonged inactivity resulting from bed rest, trauma, casting, or local nerve damage (McCance and Huether, 2009).
Periods of immobility or prolonged bed rest cause major physiological, psychological, and social effects. These effects are gradual or immediate and vary from patient to patient. The greater the extent and the longer the duration of immobility, the more pronounced the consequences. The patient with complete mobility restrictions is continually at risk for the hazards of immobility.
Systemic Effects
All body systems work more efficiently with some form of movement. Exercise has positive outcomes for all major systems of the body. When there is an alteration in mobility, each body system is at risk for impairment. The severity of the impairment depends on the patient’s overall health, degree and length of immobility, and age. For example, older adults with chronic illnesses develop pronounced effects of immobility more quickly than do younger patients with the same immobility problem.
Metabolic Changes
Changes in mobility alter endocrine metabolism, calcium resorption, and functioning of the gastrointestinal system. The endocrine system, made up of hormone-secreting glands, maintains and regulates vital functions such as (1) response to stress and injury; (2) growth and development; (3) reproduction; (4) maintenance of the internal environment; and (5) energy production, use, and storage.
When injury or stress occurs, the endocrine system triggers a series of responses aimed at maintaining blood pressure and preserving life. It is important in maintaining homeostasis. Tissues and cells live in an internal environment that the endocrine system helps regulate through maintenance of sodium, potassium, water, and acid-base balance. It also regulates energy metabolism. Thyroid hormone increases the basal metabolic rate (BMR), and energy becomes available to cells through the integrated action of gastrointestinal and pancreatic hormones (McCance and Huether, 2009).
Immobility disrupts normal metabolic functioning: decreasing the metabolic rate; altering the metabolism of carbohydrates, fats, and proteins; causing fluid, electrolyte, and calcium imbalances; and causing gastrointestinal disturbances such as decreased appetite and slowing of peristalsis. However, in the presence of an infectious process, immobilized patients often have an increased BMR as a result of fever or wound healing because these increase cellular oxygen requirements (Huether and McCance, 2008).
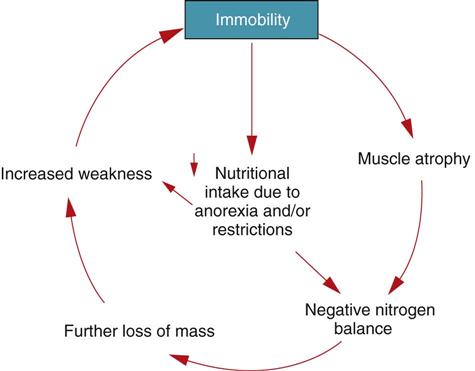
A deficiency in calories and protein is characteristic of patients with a decreased appetite secondary to immobility. The body is constantly synthesizing proteins and breaking them down into amino acids to form other proteins (see Chapter 41). When the patient is immobile, his or her body often excretes more nitrogen (the end product of amino acid breakdown) than it ingests in proteins, resulting in negative nitrogen balance (Fig. 47-4). Weight loss, decreased muscle mass, and weakness result from tissue catabolism (tissue breakdown) (McCance and Huether, 2009).
Another metabolic change associated with immobility is calcium resorption (loss) from bones. Immobility causes the release of calcium into the circulation. Normally the kidneys excrete the excess calcium. However, if the kidneys are unable to respond appropriately, hypercalcemia results. Pathological fractures occur if calcium resorption continues as the patient remains on bed rest or continues to be immobile (Huether and McCance, 2008).
Impairments of gastrointestinal functioning caused by decreased mobility vary. Difficulty in passing stools (constipation) is a common symptom, although pseudodiarrhea often results from a fecal impaction (accumulation of hardened feces). Be aware that this finding is not normal diarrhea, but rather liquid stool passing around the area of impaction (see Chapter 46). Left untreated, fecal impaction results in a mechanical bowel obstruction that partially or completely occludes the intestinal lumen, blocking normal propulsion of liquid and gas. The resulting fluid in the intestine produces distention and increases intraluminal pressure. Over time intestinal function becomes depressed, dehydration occurs, absorption ceases, and fluid and electrolyte disturbances worsen.
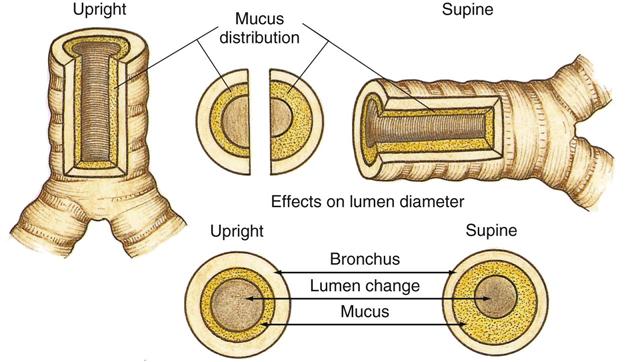
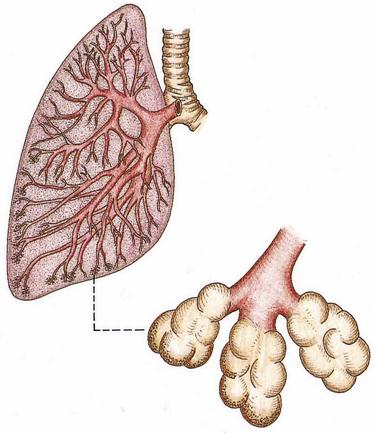
Respiratory Changes
Regular aerobic exercise enhances respiratory functioning. Lack of movement and exercise places patients at higher risk for respiratory complications. Patients who are immobile are at high risk for developing pulmonary complications. The most common respiratory complications are atelectasis (collapse of alveoli) and hypostatic pneumonia (inflammation of the lung from stasis or pooling of secretions). Both decreased oxygenation and prolonged recovery add to the patient’s discomfort (Lewis et al., 2011). In atelectasis secretions block a bronchiole or a bronchus; and the distal lung tissue (alveoli) collapses as the existing air is absorbed, producing hypoventilation. The site of the blockage affects the severity of atelectasis. Sometimes an entire lung lobe or a whole lung collapses. At some point in the development of these complications, there is a proportional decline in the patient’s ability to cough productively. Ultimately the distribution of mucus in the bronchi increases, particularly when the patient is in the supine, prone, or lateral position (Fig. 47-5). Mucus accumulates in the dependent regions of the airways (Fig. 47-6). Hypostatic pneumonia frequently results because mucus is an excellent place for bacteria to grow.
Cardiovascular Changes
Immobilization also affects the cardiovascular system. The three major changes are orthostatic hypotension, increased cardiac workload, and thrombus formation.
Orthostatic hypotension is an increase in heart rate of more than 15% and a drop of 15 mm Hg or more in systolic blood pressure or a drop of 10 mm Hg or more in diastolic blood pressure when the patient changes from the supine to standing position (Huether and McCance, 2008). In the immobilized patient decreased circulating fluid volume, pooling of blood in the lower extremities, and decreased autonomic response occur. These are especially evident in the older adult.
As the workload of the heart increases, so does its oxygen consumption. Therefore the heart works harder and less efficiently during periods of prolonged rest. As immobilization increases, cardiac output falls, further decreasing cardiac efficiency and increasing workload.
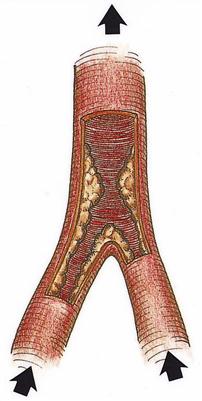
Patients who are immobile are also at risk for thrombus formation. A thrombus is an accumulation of platelets, fibrin, clotting factors, and the cellular elements of the blood attached to the interior wall of a vein or artery, which sometimes occludes the lumen of the vessel (Fig. 47-7). Three factors contribute to venous thrombus formation: (1) damage to the vessel wall (e.g., injury during surgical procedures), (2) alterations of blood flow (e.g., slow blood flow in calf veins associated with bed rest), and (3) alterations in blood constituents (e.g., a change in clotting factors or increased platelet activity). These three factors are often referred to as Virchow’s triad (Huether and McCance, 2008).
Musculoskeletal Changes
The effects of immobility on the musculoskeletal system include permanent or temporary impairment or permanent disability. Restricted mobility sometimes results in loss of endurance, strength, and muscle mass and decreased stability and balance. Other effects of restricted mobility affecting the skeletal system are impaired calcium metabolism and joint mobility.
Muscle Effects
Because of protein breakdown, the patient loses lean body mass. The reduced muscle mass is unable to sustain activity without increased fatigue. If immobility continues and the patient does not exercise, there is further loss of muscle mass. Muscle weakness always occurs with immobility, and prolonged immobility often leads to disuse atrophy. Muscle atrophy is a widely observed response to illness, decreased ADLs, and immobilization. Loss of endurance, decreased muscle mass and strength, and joint instability (see Skeletal Effects) put patients at risk for falls (see Chapter 38).
Skeletal Effects
Immobilization causes two skeletal changes: impaired calcium metabolism and joint abnormalities. Because immobilization results in bone resorption, the bone tissue is less dense or atrophied, and disuse osteoporosis results. When disuse osteoporosis occurs, the patient is at risk for pathological fractures.
Osteoporosis is a major health concern in this country. The first Surgeon General’s report on the topic of bone health stated that one in two Americans over 50 years of age will be at risk for fractures related to osteoporosis by the year 2020. Furthermore, the National Osteoporosis Foundation (2010) reports that 44 million Americans (55% of those over the age of 50) either have osteoporosis or are at risk for developing it. Approximately 80% of people who have osteoporosis are female. Although primary osteoporosis is different in origin from the osteoporosis that results from immobility, it is imperative for nurses to recognize that immobilized patients are at high risk for accelerated bone loss if they have primary osteoporosis.
Immobility can lead to joint contractures. A joint contracture is an abnormal and possibly permanent condition characterized by fixation of the joint. It is important to note that flexor muscles for joints are stronger than extensor muscles and therefore contribute to the formation of contractures. Disuse, atrophy, and shortening of the muscle fibers cause joint contractures. When a contracture occurs, the joint cannot achieve full ROM. Contractures sometimes leave a joint or joints in a nonfunctional position, as seen in patients who are permanently curled in a fetal position. Early prevention of contractures is essential; they can begin to form after only 8 hours of immobility in the older adult (Fletcher, 2005).
One common and debilitating contracture is footdrop (Fig. 47-8). When footdrop occurs, the foot is permanently fixed in plantar flexion. Ambulation is difficult with the foot in this position because the patient cannot dorsiflex the foot. The patient with footdrop is unable to lift the toes off the ground. Patients who have suffered CVAs or brain attacks with resulting right- or left-sided paralysis (hemiplegia) are at risk for footdrop.
Urinary Elimination Changes
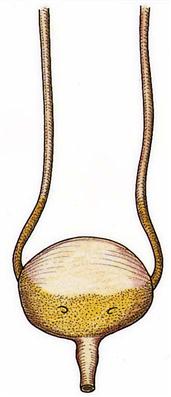
Immobility alters the patient’s urinary elimination. In the upright position urine flows out of the renal pelvis and into the ureters and bladder because of gravitational forces. When the patient is recumbent or flat, the kidneys and ureters move toward a more level plane. Urine formed by the kidney needs to enter the bladder unaided by gravity. Because the peristaltic contractions of the ureters are insufficient to overcome gravity, the renal pelvis fills before urine enters the ureters (Fig. 47-9). This condition is called urinary stasis and increases the risk of urinary tract infection and renal calculi (see Chapter 45). Renal calculi are calcium stones that lodge in the renal pelvis or pass through the ureters. Immobilized patients are at risk for calculi because they frequently have hypercalcemia.
As the period of immobility continues, fluid intake often diminishes. When combined with other problems such as fever, the risk for dehydration increases. As a result, urinary output declines on or about the fifth or sixth day after immobilization, and the urine becomes concentrated. This concentrated urine increases the risk for calculi formation and infection. Inappropriate perineal care after bowel movements, particularly in women, increases the risk of urinary tract contamination by Escherichia coli bacteria. Another cause of urinary tract infections in immobilized patients is the use of an indwelling urinary catheter.
Integumentary Changes
The changes in metabolism that accompany immobility add to the harmful effect of pressure on the skin in the immobilized patient. This makes immobility a major risk factor for pressure ulcers. Any break in the integrity of the skin is difficult to heal. Preventing a pressure ulcer is much less expensive than treating one; therefore preventive nursing interventions are imperative (WOCN, 2009).
A pressure ulcer is an impairment of the skin as a result of prolonged ischemia (decreased blood supply) in tissues (see Chapter 48). The ulcer is characterized initially by inflammation and usually forms over a bony prominence. Ischemia develops when the pressure on the skin is greater than the pressure inside the small peripheral blood vessels supplying blood to the skin.
Tissue metabolism depends on the supply of oxygen and nutrients to and the elimination of metabolic wastes from the blood. Pressure affects cellular metabolism by decreasing or totally eliminating tissue circulation. When a patient lies in bed or sits in a chair, the weight of the body is on bony prominences. The longer the pressure is applied, the longer the period of ischemia and therefore the greater the risk of skin breakdown. The older adult is especially at risk. For example, an older adult who is immobilized on a backboard following a trauma can develop skin breakdown within 3 hours (Fletcher, 2005).
Psychosocial Effects
Immobilization often leads to emotional and behavioral responses, sensory alterations, and changes in coping. When normal, healthy young men who were part of a National Aeronautics and Space Administration (NASA) study were on bed rest for several weeks, they exhibited signs of sensory deprivation: altered sleep patterns and significant increases in anxiety, hostility, and depression (Fletcher, 2005). Every patient responds to immobility differently.
Patients with restricted mobility may have some depression. Depression is an affective disorder characterized by exaggerated feelings of sadness, melancholy, dejection, worthlessness, emptiness, and hopelessness out of proportion to reality. It results from worrying about present and future levels of health, finances, and family needs. Because immobilization removes the patient from a daily routine, he or she has more time to worry about disability. Worrying quickly increases the patient’s depression, causing withdrawal. Withdrawn patients often do not want to participate in their own care.
Developmental Changes
Developmental changes tend to be associated with immobility in the very young and older adults. The immobilized young or middle-age adult who has been healthy experiences few, if any, developmental changes. However, there are exceptions. For example, a mother with complications following birth has to go onto bed rest and as a result cannot interact with her newborn as expected.
Infants, Toddlers, and Preschoolers
The newborn infant’s spine is flexed and lacks the anteroposterior curves of the adult (see Chapter 12). As the baby grows, musculoskeletal development permits support of weight for standing and walking. Posture is awkward because the head and upper trunk are carried forward. Because body weight is not distributed evenly along a line of gravity, posture is off balance, and falls occur often. The infant, toddler, or preschooler is usually immobilized because of trauma or the need to correct a congenital skeletal abnormality. Prolonged immobilization delays the child’s gross motor skills, intellectual development, or musculoskeletal development.
Adolescents
The adolescent stage usually begins with a tremendous increase in growth (see Chapter 12). Growth is frequently uneven. Prolonged immobilization alters adolescent growth patterns. In addition, adolescents who experience immobility often are behind peers in gaining independence and accomplishing certain skills such as obtaining a driver’s license. Social isolation is a concern for this age-group when immobilization occurs.
Adults
An adult who has correct posture and body alignment feels good, looks good, and generally appears self-confident. The healthy adult also has the necessary musculoskeletal development and coordination to carry out ADLs (see Chapter 13). When periods of prolonged immobility occur, all physiological systems are at risk. In addition, the role of the adult often changes with regard to the family or social structure. Some adults lose their jobs, which affects their self-concept (see Chapter 33).
Older Adults
A progressive loss of total bone mass occurs with the older adult. Some of the possible causes of this loss include decreased physical activity, hormonal changes, and bone resorption. The effect of bone loss is weaker bones. Older adults often walk more slowly, take smaller steps, and appear less coordinated. Prescribed medications alter their sense of balance or affect their blood pressure when they change position too quickly, increasing their risk for falls and injuries (see Chapter 14). The outcomes of a fall include not only possible injury but also hospitalization, loss of independence, psychological effects, and quite possibly death (yeom et al., 2009).
Older adults often experience functional status changes secondary to hospitalization and altered mobility status (Box 47-1). Immobilization of older adults increases their physical dependence on others and accelerates functional losses. Immobilization of some older adults results from a degenerative disease, neurological trauma, or chronic illness. In others it occurs gradually and progressively, and in others—especially those who have had a stroke—immobilization is sudden. When providing nursing care for an older adult, encourage the patient to perform as many self-care activities as possible, thereby maintaining the highest level of mobility. Sometimes nurses inadvertently contribute to a patient’s immobility by providing unnecessary help with activities such as bathing and transferring.