Military Carriers
Chapter objectives
After completion of this chapter, the student should be able to:
1. Discuss the role of the Military Health Program.
2. Outline the TRICARE program, including eligibility and enrollment options.
3. Describe TRICARE’s supplemental programs.
4. Explain the process of verifying TRICARE eligibility.
5. Distinguish between TRICARE PARs and nonPARs.
6. Recap TRICARE’s cost-sharing requirements.
7. Describe the TRICARE claims process.
8. Explain the CHAMPVA program, including eligibility.
9. Discuss what the Department of Defense has done to implement HIPAA’s privacy rules.
Chapter terms
accepting assignment
balance bill
catastrophic cap (cat cap)
certificate of credible coverage
CHAMPUS Maximum Allowable Charge
CHAMPVA for Life (CFL)
Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA)
Civilian Health and Medical Program of the Uniformed Services (CHAMPUS)
claims processor
custodial care
covered charges
Defense Enrollment Eligibility Reporting System (DEERS)
eZ TRICARE
Military Health System
military treatment facility (MTF)
nonavailability statement (NAS)
other health insurance (OHI)
regional contractor
sponsor
TRICARE
TRICARE for Life (TFL)
TRICARE Management Activity
TRICARE Supplemental Insurance
TRICARE allowable charge
XPressClaim
Military health programs
The federal government has provided healthcare for the military from the earliest years of U.S. history. In 1884 Congress requested that Army medical officers and surgeons attend to the families of the officers and soldiers free of charge whenever possible. During World War II, Congress authorized the creation of the Emergency Maternal and Infant Care Program, which provided maternity care and care of infants up to 1 year of age for wives and children of service members. During the Korean War, in 1956, the Dependents Medical Care Act became law. The 1966 amendments to this law initiated what later became the Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), a military healthcare program that existed for more than 30 years, until it was replaced with TRICARE in 1998.
TRICARE
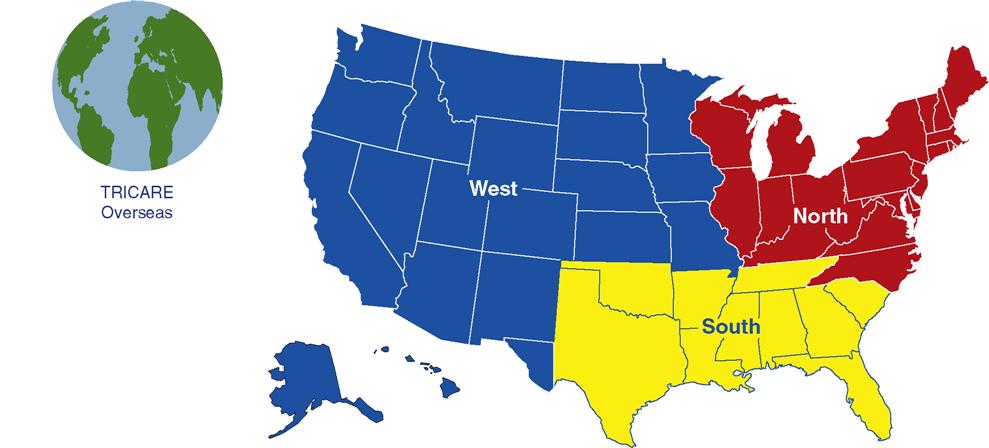
TRICARE (TRI because it offers three different plans) is a worldwide healthcare system for the military. This wide-ranging program combines resources of the uniformed services and supplements them with networks of civilian healthcare professionals, institutions, pharmacies, and suppliers to give enrollees access to cost-efficient, high-quality healthcare. TRICARE serves nearly 10 million beneficiaries worldwide, including National Guard and Reserve members, retirees, their families, survivors, and certain former spouses. The TRICARE program is managed by TRICARE Management Activity (TMA) under the authority of the U.S. Assistant Secretary of Defense (Health Affairs). TRICARE is organized into six geographic parts: West, North, and South regions, and three overseas “areas”: Eurasia-Africa, Latin America and Canada, and the Pacific Areas (Fig. 10-1). Each region/area has its own regional office and regional contractor. Each region/area:
• provides oversight of operations and health plan administration at the regional level;
• manages the contracts with regional contractors;
• supports Military Treatment Facility (MTF) Commanders;
• develops business plans for non-MTF areas (e.g., remote areas); and
• funds regional initiatives to enhance and improve delivery of healthcare.
Military Health System
Military Health System (MHS) is the name for the total healthcare infrastructure of the U.S. uniformed services under which TRICARE operates. Its mission is “to enhance the Department of Defense (DOD) and our Nation’s security by providing health support for the full range of military operations and sustaining the health of all those entrusted to our care.” The MHS includes military treatment facilities (MTFs) and various programs, such as TRICARE, within the civilian population. MTFs are clinics or hospitals operated by the DoD, located on military bases that provide care to military personnel, retirees, and dependents. The MHS provides cost-effective, quality medical care through a network of providers, MTFs, medical clinics, and dental clinics worldwide.
Source: http://www.fhpr.osd.mil/pdfs/MHS%20QDR%20Medical%20Transformation%20Roadmap.pdf
TRICARE Management Activity (TMA)
Since February 1998, TMA has administered the TRICARE healthcare program through the MHS. The mission of TMA is to manage TRICARE—the medical and dental programs under which members of the uniformed services, their dependents, and other beneficiaries are entitled to DoD healthcare. TMA also supports the military departments in implementing its medical mission to provide, and to maintain readiness to provide, medical and dental services to members of the Armed Forces during military operations.
Like the activities of all government agencies, TMA is updated frequently, and the health insurance professional should be aware of these updates. To keep abreast of changes, visit the Evolve site.
TRICARE Regional Contractors
As mentioned, TRICARE is administered on a regional basis. Each region is headed by a regional contractor whose responsibility it is to provide beneficiaries with healthcare services and support in addition to what services are available at MTFs. These responsibilities include:
Who is Eligible for TRICARE?
Like recipients of Medicaid and Medicare, TRICARE-eligible individuals are referred to as “beneficiaries.” The service member, whether in active duty, retired, or deceased, is called the sponsor. The sponsor’s relationship to the beneficiary (spouse, child, parent) creates eligibility under TRICARE. In addition, to be eligible for TRICARE, an individual must be registered in the Defense Enrollment Eligibility Reporting System (DEERS). DEERS is a global computerized database of uniformed services members, their family members, and others who are eligible for military benefits. Enrollment in DEERS is the key to using TRICARE benefits. All sponsors are automatically registered in DEERS when they enter the military; however, it is the sponsor’s responsibility to register eligible family members. Family members can update personal information such as addresses and phone numbers once they are registered.
TRICARE-eligible individuals can be classified into the following main categories:
• Active duty service members (ADSMs), who are automatically enrolled in TRICARE Prime;
• Spouses and unmarried children of ADSMs (active duty family members [ADFMs])
• Uniformed service retirees, their spouses, and unmarried children
For more details regarding TRICARE-eligible individuals, visit the Evolve site.
Who Is Not Eligible for TRICARE?
Categories of individuals not eligible for TRICARE include the following:
Losing TRICARE Eligibility
Eligibility for TRICARE may end for the following reasons:
• Sponsor separates from active duty; that is, he or she “gets out” of the military before retiring.
• Beneficiary becomes entitled to Medicare Part A but does not purchase Medicare Part B.
• Surviving spouse, widow, or former spouse remarries.
Note: The preceding list is not intended to be all-inclusive.
Upon loss of TRICARE eligibility, each member automatically receives a certificate of credible coverage, which serves as evidence of prior healthcare coverage under TRICARE, so that the individual cannot be excluded from a new health plan because of preexisting conditions.
TRICARE Program Options
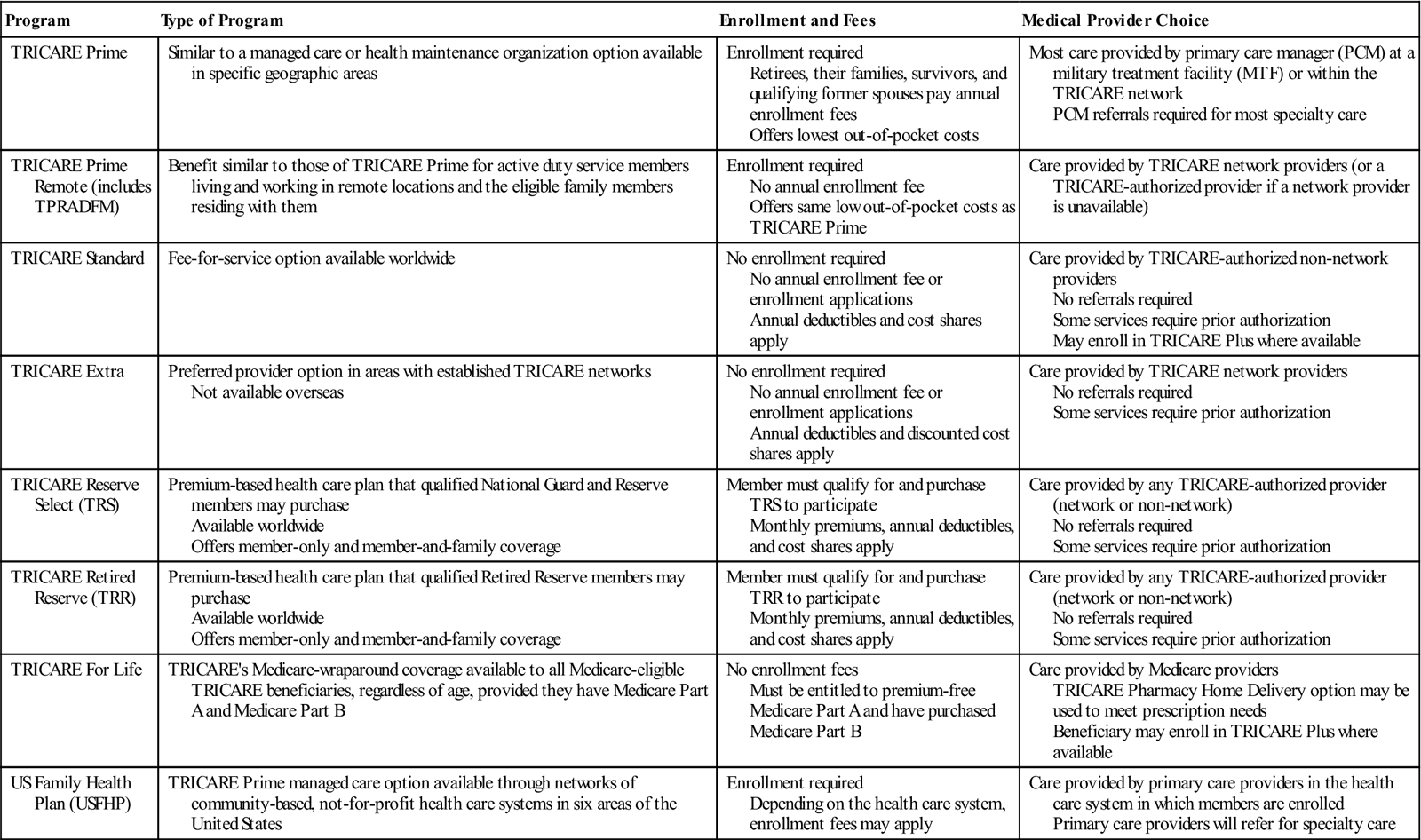
Depending on the category and location of the beneficiary, he or she may be eligible for different program options. These options may change when the enrollee travels or moves, or when he or she becomes entitled to Medicare Part A, discussed later in this chapter. See Table 10-1 for details on TRICARE program options. Table 10-2 provides program information on the TRICARE programs—the type of program, enrollment and fees, and provider choice.
Table 10-1
| Beneficiary Type | Program Options |
| Active duty service members (ADSMs) (Includes National Guard and Reserve members activated for more than 30 consecutive days) | TRICARE Prime TRICARE Prime Remote TRICARE Active Duty Dental Program |
| Active duty family members (ADFMs) (Includes family members of National Guard and Reserve members activated for more than 30 consecutive days and certain survivors) | TRICARE Prime TRICARE Prime Remote for Active Duty Family Members (TPRADFM) TRICARE Standard TRICARE Extra TRICARE For Life (TFL) (ADFMs must have Medicare Part B to participate in TFL) US Family Health Plan TRICARE Dental Program |
| Retired service members and eligible family members, survivors, Medal of Honor recipients, qualified former spouses, and others | TRICARE Prime TRICARE Standard TRICARE Extra TFL (if entitled to premium-free Medicare Part A on basis of age, disability, or end-stage renal disease, the beneficiary must have Medicare Part B to keep TRICARE eligibility) US Family Health Plan TRICARE Retiree Dental Program |
| National Guard and Reserve members and their family members (Qualified non–active duty members of the Selected Reserve, Retired Reserve, and certain members of the Individual Ready Reserve) | TRICARE Reserve Select (members of the Selected Reserve) TRICARE Retired Reserve (members of the Retired Reserve younger than 60 years) TRICARE Dental Program TRICARE Retiree Dental Program |
“TRICARE” is a registered trademark of the TRICARE Management Activity. All rights reserved.
Table 10-2
| Program | Type of Program | Enrollment and Fees | Medical Provider Choice |
| TRICARE Prime | Similar to a managed care or health maintenance organization option available in specific geographic areas | Enrollment required Retirees, their families, survivors, and qualifying former spouses pay annual enrollment fees Offers lowest out-of-pocket costs | Most care provided by primary care manager (PCM) at a military treatment facility (MTF) or within the TRICARE network PCM referrals required for most specialty care |
| TRICARE Prime Remote (includes TPRADFM) | Benefit similar to those of TRICARE Prime for active duty service members living and working in remote locations and the eligible family members residing with them | Enrollment required No annual enrollment fee Offers same low out-of-pocket costs as TRICARE Prime | Care provided by TRICARE network providers (or a TRICARE-authorized provider if a network provider is unavailable) |
| TRICARE Standard | Fee-for-service option available worldwide | No enrollment required No annual enrollment fee or enrollment applications Annual deductibles and cost shares apply | Care provided by TRICARE-authorized non-network providers No referrals required Some services require prior authorization May enroll in TRICARE Plus where available |
| TRICARE Extra | Preferred provider option in areas with established TRICARE networks Not available overseas | No enrollment required No annual enrollment fee or enrollment applications Annual deductibles and discounted cost shares apply | Care provided by TRICARE network providers No referrals required Some services require prior authorization |
| TRICARE Reserve Select (TRS) | Premium-based health care plan that qualified National Guard and Reserve members may purchase Available worldwide Offers member-only and member-and-family coverage | Member must qualify for and purchase TRS to participate Monthly premiums, annual deductibles, and cost shares apply | Care provided by any TRICARE-authorized provider (network or non-network) No referrals required Some services require prior authorization |
| TRICARE Retired Reserve (TRR) | Premium-based health care plan that qualified Retired Reserve members may purchase Available worldwide Offers member-only and member-and-family coverage | Member must qualify for and purchase TRR to participate Monthly premiums, annual deductibles, and cost shares apply | Care provided by any TRICARE-authorized provider (network or non-network) No referrals required Some services require prior authorization |
| TRICARE For Life | TRICARE’s Medicare-wraparound coverage available to all Medicare-eligible TRICARE beneficiaries, regardless of age, provided they have Medicare Part A and Medicare Part B | No enrollment fees Must be entitled to premium-free Medicare Part A and have purchased Medicare Part B | Care provided by Medicare providers TRICARE Pharmacy Home Delivery option may be used to meet prescription needs Beneficiary may enroll in TRICARE Plus where available |
| US Family Health Plan (USFHP) | TRICARE Prime managed care option available through networks of community-based, not-for-profit health care systems in six areas of the United States | Enrollment required Depending on the health care system, enrollment fees may apply | Care provided by primary care providers in the health care system in which members are enrolled Primary care providers will refer for specialty care |
“TRICARE” is a registered trademark of the TRICARE Management Activity. All rights reserved.
TRICARE Overseas Program (TOP)
TRICARE Overseas Program (TOP) has one overseas region consisting of three areas: TRICARE Eurasia-Africa, TRICARE Pacific, and TRICARE Latin America/Canada (TLAC) including the Caribbean basin. TOP provides health benefits to beneficiaries living and traveling overseas while they are eligible for TRICARE. TOP allows for significant cultural differences unique to foreign countries and their healthcare practices. The TRICARE Area Office (TAO) Director is responsible for the overall management of TOP. For more detailed information on this program, along with coverage options, visit the Evolve site.
TRICARE Young Adult (TYA) Program
Beginning May of 2011, adult children of military members and retirees younger than 26 years who are unmarried and are not eligible for their own employer-sponsored health care coverage may become eligible to purchase TRICARE Young Adult (TYA) Program coverage as long as their sponsor is still eligible for TRICARE. Initially, TRICARE Standard was the only TYA option; however, TRICARE Prime became another option for TYA enrollees effective October 1, 2011—the beginning of the federal government’s new fiscal year. To use Prime, however, qualifying young adults must live in areas where a TRICARE managed-care network is available. Monthly premiums for both Standard and Prime are considerably higher than what a military family typically pays to enroll in TRICARE. Cost shares, deductibles, and catastrophic cap protection are based on the sponsor’s status and the type of coverage selected.
What TRICARE Pays
Like most insurers, TRICARE pays for only allowed services, supplies, and procedures, which are referred to as covered charges. TRICARE’s covered charges include medical and psychological services and supplies that are considered appropriate care and are generally accepted by qualified professionals to be reasonable and adequate for the diagnosis and treatment of illness, injury, pregnancy, or mental disorders or for well-child care.
TRICARE’s allowable charge, also known as the CHAMPUS Maximum Allowable Charge (CMAC), is the amount on which TRICARE figures a beneficiary’s cost share (coinsurance) for covered charges. TRICARE calculates this allowable charge by looking at all professional (noninstitutional) providers’ fees for the same or similar services nationwide over the past year, with adjustments for specific localities. If the health insurance professional does not know what the allowable charge is for a particular service or supply, he or she can telephone the regional claims processor for this information or consult the TRICARE provider handbook. It is advisable to keep a current copy of the handbook on file for information regarding TRICARE billing and claims submission guidelines.
TRICARE’s additional programs
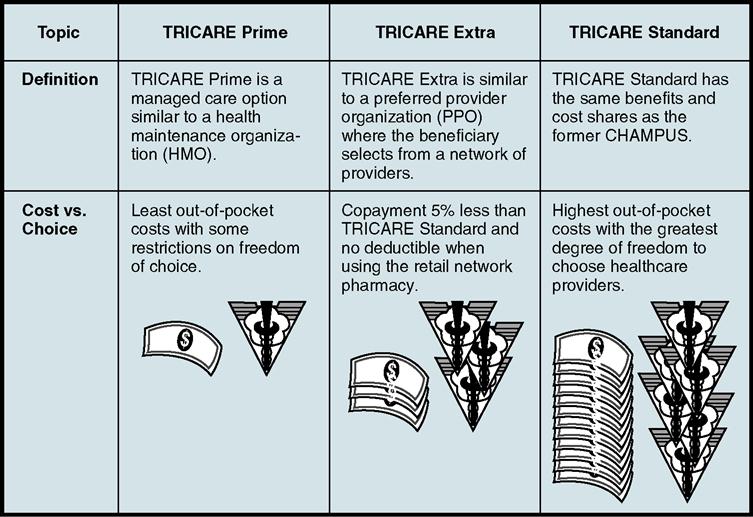
The three basic program options under TRICARE are TRICARE Standard, TRICARE Extra, and TRICARE Prime (Fig. 10-2). To use TRICARE Extra or TRICARE Prime, the individual receiving care must live in an area where these options are available and a civilian provider network has been established to support these plans. It is important to keep in mind that active duty, guard, and reserve members are automatically enrolled in TRICARE Prime. Military retirees and their dependents must choose the option that best suits their needs.
TRICARE Dental Programs
TRICARE also offers dental programs for both active duty and retirees. The TRICARE Active Duty Dental Program (ADDP) is available to eligible active duty service members who are either referred for care by a dental treatment facility (DTF) to a civilian dentist or have a duty location and live more than 50 miles from a DTF. ADSMs enrolled in Prime Remote are automatically eligible to use the Remote ADDP. National Guard and Reserve members are eligible only if they have active duty orders issued for a period of more than 30 consecutive days.
The TRICARE Retiree Dental Program (TRDP) is available to retired service members and their eligible family members, including retired National Guard and Reserve members. Enrollees must satisfy an initial 12-month enrollment period in order to become eligible for the full scope of benefits. New retirees who elect to enroll within 4 months after retirement are eligible for a waiver of this 12-month waiting period.
For detailed information on TRICARE health plan options, visit the Evolve site.
TRICARE Standard Nonavailability Statement
As discussed previously, military personnel and their TRICARE-eligible dependents typically receive healthcare at an MTF. If the needed treatment is unavailable at an MTF and it becomes necessary for the individual to seek treatment in a civilian hospital, he or she sometimes must obtain a nonavailability statement (NAS). An NAS is certification from a military hospital stating that it cannot provide the care that a TRICARE beneficiary needs. If the beneficiary does not get an NAS before receiving inpatient care from a civilian source, TRICARE may not share the costs. The NAS system is now automated. This means that instead of sending a paper copy of the NAS in with the TRICARE claim, the MTF enters the NAS electronically into the DEERS computer files.
Even though an outpatient NAS is no longer required for outpatient procedures (except in specific situations, e.g., maternity), the beneficiary must obtain advance authorization to undergo any procedures. Healthcare providers—whether or not they participate in TRICARE Standard—are required to obtain these advance authorizations. To learn more about this topic, visit the Evolve site.
Supplemental TRICARE Programs
TRICARE offers supplemental programs tailored specifically to beneficiary health concerns or conditions. Many of these programs have specific eligibility requirements based on beneficiary category, plan, or status. They include health promotion programs such as alcohol education, smoking cessation, and weight loss. Some are for specific populations, such as the Foreign Force Member Health Care Option and the Pre-activation Benefit for National Guard and Reserve. Other programs are for certain health conditions, such as the Cancer Clinical Trials. Many programs are limited to a certain number of participants or a particular geographic location. The following sections discuss two of these special programs. For detailed information on all of these special TRICARE programs, visit the Evolve site.
Exceptional Family Member Program
The Exceptional Family Member Program (EFMP) is a mandatory enrollment program based on specifically defined rules. EFMP works with other military and civilian agencies to provide comprehensive and coordinated medical, educational, housing, community support, and personnel services to families with special needs. An exceptional family member is a dependent, regardless of age, who requires medical services for a chronic condition; receives ongoing services from a specialist; has mental health concerns/social problems/psychological needs; receives education services provided by means of an Individual Education Program (IEP); or a family member receiving services provided through an Individual Family Services Plan (IFSP). To learn more about EFMP, visit the Evolve site.
TRICARE Plus
TRICARE Plus is a military treatment facility primary care enrollment program that is offered at selected local MTFs. This program allows beneficiaries who normally are only able to get care at MTFs on a space-available basis, and who are not enrolled in a TRICARE Prime option, to enroll and receive primary care appointments at the MTF within the same primary care access standards as beneficiaries enrolled in a TRICARE Prime option. Non-enrollment in TRICARE Plus does not affect TRICARE For Life benefits or other existing programs. (TRICARE For Life is discussed later in this chapter.)
TRICARE and Other Health Insurance (OHI)
If a TRICARE-eligible beneficiary has other healthcare coverage besides TRICARE Standard, Extra, or Prime through an employer, an association, or a private insurer, or if a student in the family has a healthcare plan through his or her school, TRICARE considers this coverage to be other health insurance (OHI). It also may be called double coverage or coordination of benefits. Any OHI a TRICARE enrollee has in addition to TRICARE coverage is considered primary health insurance. If a TRICARE beneficiary has OHI, he or she should tell the healthcare provider and regional contractor. Keeping the regional contractor informed about OHI will allow TRICARE to better coordinate benefits and will help ensure that there is no delay in payment of claims.
TRICARE Fact: OHI does not include TRICARE supplemental insurance or Medicaid. These programs are not primary to TRICARE.
TRICARE Standard Supplemental Insurance
TRICARE Supplemental Insurance policies, similar to Medicare supplemental insurance policies, are health benefit plans designed specifically to supplement TRICARE benefits. These plans are frequently available from military associations or other private organizations. Although TRICARE supplement plans have their own rules, they generally pay most or all of whatever is left after TRICARE has paid its share of the cost of covered services and supplies. Such policies are not specifically for retirees and may be advantageous for other TRICARE-eligible families as well.
TRICARE For Life
TRICARE For Life (TFL) is TRICARE’s Medicare-wraparound coverage available to all Medicare-eligible TRICARE beneficiaries regardless of age or place of residence provided that they have both Medicare Part A and Part B. Medicare is the primary insurer, but TRICARE acts as secondary payer, minimizing out-of-pocket expenses. TFL benefits include covering Medicare’s coinsurance and deductible. Whether the beneficiary uses either a provider who does participate in Medicare (PAR) or one who does not (nonPAR), the provider files claims with Medicare. Medicare pays its portion first and electronically forwards the claim to the TFL claims processor. TFL pays the provider directly for TRICARE-covered services. TFL has no enrollment fees and no monthly premium cost, and is a permanent healthcare benefit for all uniformed service branches.
TRICARE For Life Eligibility
TFL is available for all dual TRICARE-Medicare–eligible uniformed services retirees, including:
• retired members of the Reserve Component who are in receipt of retirement pay,
• Medicare-eligible family members, and
Dependent parents and parents-in-law are not eligible for TRICARE Prime, Standard, or Extra or TRICARE For Life. They are eligible, however, to receive care under the sponsor’s TRICARE benefits at an MTF on a space-available basis. Care received outside the MTF must be covered by another form of insurance. They may also be eligible for TRICARE Senior Pharmacy benefits if they are entitled to Medicare Part A, if they turned 65 on or after April 1, 2001, and if they are enrolled in Medicare Part B.
TRICARE Fact: ADFMs are not required to have Medicare Part B to remain eligible for TRICARE. Once the sponsor reaches age 65, Medicare Part B must be in effect no later than the sponsor’s retirement date to avoid a break in TRICARE coverage.
For a more comprehensive look at TFL, visit the Evolve site.