Medication Administration
Objectives
• Discuss the nurse’s role and responsibilities in medication administration.
• Describe the physiological mechanisms of medication action.
• Differentiate among different types of medication actions.
• Discuss developmental factors that influence pharmacokinetics.
• Discuss factors that influence medication actions.
• Discuss methods used to educate patients about prescribed medications.
• Implement nursing actions to prevent medication errors.
• Describe factors to consider when choosing routes of medication administration.
• Calculate prescribed medication doses correctly.
• Discuss factors to include in assessing a patient’s needs for and response to medication therapy.
• Identify the six rights of medication administration and apply them in clinical settings.
Key Terms
Absorption, p. 567
Adverse effects, p. 569
Anaphylactic reactions, p. 569
Biological half-life, p. 570
Biotransformation, p. 568
Buccal, p. 572
Detoxify, p. 568
Idiosyncratic reaction, p. 569
Infusions, p. 570
Injection, p. 567
Instillation, p. 572
Intraarticular, p. 572
Intracardiac, p. 572
Intradermal (ID), p. 572
Intramuscular (IM), p. 572
Intraocular, p. 573
Intravenous (IV), p. 572
Irrigations, p. 573
Medication allergy, p. 569
Medication error, p. 582
Medication interaction, p. 569
Medication reconciliation, p. 583
Metric system, p. 573
Nurse Practice Acts (NPAs), p. 566
Ophthalmic, p. 596
Parenteral administration, p. 572
Peak, p. 570
Pharmacokinetics, p. 567
Polypharmacy, p. 591
Prescriptions, p. 581
Pressurized metered-dose inhalers (pMDIs), p. 599
Side effects, p. 569
Solution, p. 573
Subcutaneous, p. 572
Sublingual, p. 571
Synergistic effect, p. 569
Therapeutic effect, p. 569
Toxic effects, p. 569
Transdermal disk, p. 572
Trough, p. 570
Verbal order, p. 577
Z-track method, p. 607
![]()
Patients with acute or chronic health problems restore or maintain their health using a variety of strategies. One of these strategies is medication, a substance used in the diagnosis, treatment, cure, relief, or prevention of health problems. No matter where they receive their health care—hospitals, clinics, or home—nurses play an essential role in safe medication preparation, administration, and evaluation of medication effects. When patients cannot administer their own medications at home, family members, friends, or home care personnel are often responsible for medication administration. In all settings, nurses are responsible for evaluating the effects of medications on the patient’s ongoing health status, teaching them about their medications and side effects, ensuring adherence to the medication regimen, and evaluating the patient’s and family caregiver’s ability to self-administer medications.
Scientific Knowledge Base
Medications are frequently used to manage diseases. Because medication administration and evaluation are a critical part of nursing practice, nurses need to have knowledge about the actions and effects of the medications taken by their patients. Administering medications safely requires an understanding of legal aspects of health care, pharmacology, pharmacokinetics, the life sciences, pathophysiology, human anatomy, and mathematics.
Medication Legislation and Standards
Federal Regulations.
The U.S. government regulates the pharmaceutical industry to protect the health of the people by ensuring that medications are safe and effective. The first American law to regulate medications was the Pure Food and Drug Act. This law simply requires all medications to be free of impure products. Subsequent legislation has set standards related to safety, potency, and efficacy. Enforcement of medication laws currently rests with the Food and Drug Administration (FDA), which ensures that all medications on the market undergo vigorous testing before they are sold to the public. Federal medication law extends and refines controls on medication sales and distribution; testing, naming, and labeling; and the regulation of controlled substances. Official publications such as the United States Pharmacopeia (USP) and the National Formulary set standards for medication strength, quality, purity, packaging, safety, labeling, and dose form. In 1993 the FDA instituted the MedWatch program. This voluntary program encourages nurses and other health care professionals to report when a medication, product, or medical event causes serious harm to a patient by completing the MedWatch form. The form is available on the MedWatch website (USFDA, 2010).
State and Local Regulation of Medication.
State and local medication laws must conform to federal legislation. States often have additional controls, including control of substances not regulated by the federal government. Local governmental bodies regulate the use of alcohol and tobacco.
Health Care Institutions and Medication Laws.
Health care agencies establish individual policies to meet federal, state, and local regulations. The size of the agency, the types of services it provides, and the types of professional personnel it employs influence these policies. Agency policies are often more restrictive than governmental controls. For example, a common agency policy is the automatic discontinuation of narcotics after a set number of days. Although a prescriber can reorder the narcotic, this policy helps to control unnecessarily prolonged medication therapy and requires the prescriber to review the need for this class of medication on a regular basis.
Medication Regulations and Nursing Practice.
State Nurse Practice Acts (NPAs) have the most influence over nursing practice by defining the scope of nurses’ professional functions and responsibilities. Most NPAs are purposefully broad so nurses’ professional responsibilities are not limited. Health care agencies often interpret specific actions allowed under NPAs; but they are not able to modify, expand, or restrict the intent of the act. The primary intent of NPAs is to protect the public from unskilled, undereducated, and unlicensed personnel.
The nurse is responsible for following legal provisions when administering controlled substances such as opioids, which are carefully controlled through federal and state guidelines. Violations of the Controlled Substances Act are punishable by fines, imprisonment, and loss of nurse licensure. Hospitals and other health care agencies have policies for the proper storage and distribution of narcotics (Box 31-1).
Pharmacological Concepts
Medication Names.
Some medications have as many as three different names. The chemical name of a medication provides an exact description of its composition and molecular structure. Nurses rarely use chemical names in clinical practice. An example of a chemical name is N-acetyl-para-aminophenol, which is commonly known as Tylenol. The manufacturer who first develops the medication gives the generic or nonproprietary name, with United States Adopted Names (USAN) Council approval (AMA, 2010). Acetaminophen is an example of a generic name. It is the generic name for Tylenol. The generic name becomes the official name listed in official publications such as the USP. The trade name, brand name, or proprietary name is the name under which a manufacturer markets a medication. The trade name has the symbol (™) at the upper right of the name, indicating that the manufacturer has trademarked the name of the medication (e.g., Panadol,™ Tempra,™ and St. Joseph Aspirin-Free Fever Reducer for Children™).
Manufacturers choose trade names that are easy to pronounce, spell, and remember. Many companies produce the same medication, and similarities in trade names are often confusing. Therefore be careful to obtain the exact name and spelling for each medication you administer to your patients. Because similarities in drug names are a common cause of medical errors, The Institute for Safe Medication Practices (ISMP) (2010a) (http://www.ismp.org/Tools/confuseddrugnames.pdf) and The Joint Commission (TJC) (2011a) (http://www.jointcommission.org/standards_information/npsgs.aspx) publish a list of medications that are frequently confused with one another. TJC’s list includes recommendations to prevent mixing these medications.
Classification.
Medication classification indicates the effect of the medication on a body system, the symptoms the medication relieves, or its desired effect. Usually each class contains more than one medication that is used for the same type of health problem. For example, patients who have asthma often take a variety of medications to control their illness such as beta2-adrenergic agonists. The beta2-adrenergic classification contains at least eight different medications (Lehne, 2010). Some are part of more than one class. For example, aspirin is an analgesic, an antipyretic, and an antiinflammatory medication.
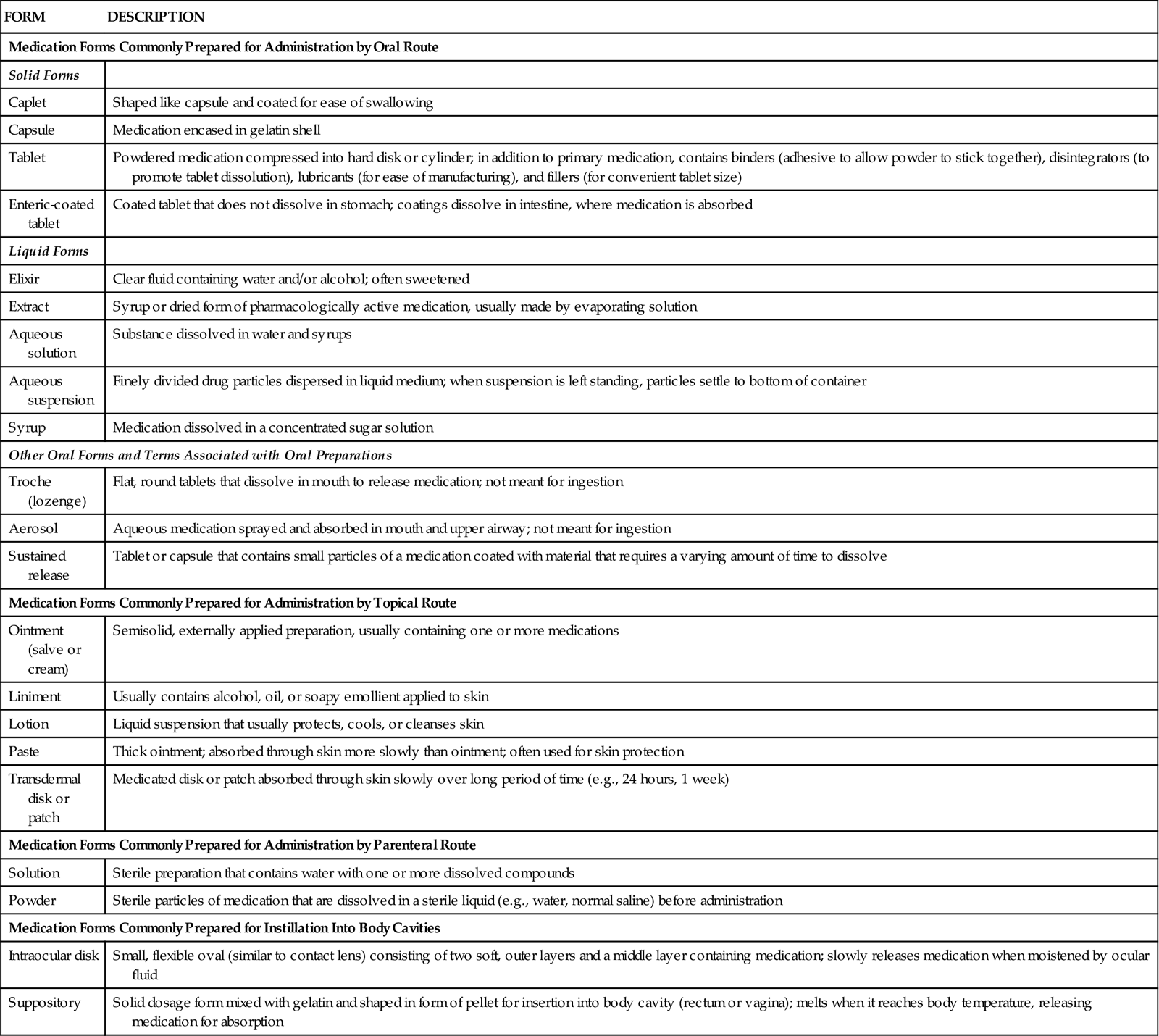
Medication Forms.
Medications are available in a variety of forms, or preparations. The form of the medication determines its route of administration. The composition of a medication enhances its absorption and metabolism. Many medications come in several forms such as tablets, capsules, elixirs, and suppositories. When administering a medication, be certain to use the proper form (Table 31-1).
TABLE 31-1
| FORM | DESCRIPTION |
| Medication Forms Commonly Prepared for Administration by Oral Route | |
| Solid Forms | |
| Caplet | Shaped like capsule and coated for ease of swallowing |
| Capsule | Medication encased in gelatin shell |
| Tablet | Powdered medication compressed into hard disk or cylinder; in addition to primary medication, contains binders (adhesive to allow powder to stick together), disintegrators (to promote tablet dissolution), lubricants (for ease of manufacturing), and fillers (for convenient tablet size) |
| Enteric-coated tablet | Coated tablet that does not dissolve in stomach; coatings dissolve in intestine, where medication is absorbed |
| Liquid Forms | |
| Elixir | Clear fluid containing water and/or alcohol; often sweetened |
| Extract | Syrup or dried form of pharmacologically active medication, usually made by evaporating solution |
| Aqueous solution | Substance dissolved in water and syrups |
| Aqueous suspension | Finely divided drug particles dispersed in liquid medium; when suspension is left standing, particles settle to bottom of container |
| Syrup | Medication dissolved in a concentrated sugar solution |
| Other Oral Forms and Terms Associated with Oral Preparations | |
| Troche (lozenge) | Flat, round tablets that dissolve in mouth to release medication; not meant for ingestion |
| Aerosol | Aqueous medication sprayed and absorbed in mouth and upper airway; not meant for ingestion |
| Sustained release | Tablet or capsule that contains small particles of a medication coated with material that requires a varying amount of time to dissolve |
| Medication Forms Commonly Prepared for Administration by Topical Route | |
| Ointment (salve or cream) | Semisolid, externally applied preparation, usually containing one or more medications |
| Liniment | Usually contains alcohol, oil, or soapy emollient applied to skin |
| Lotion | Liquid suspension that usually protects, cools, or cleanses skin |
| Paste | Thick ointment; absorbed through skin more slowly than ointment; often used for skin protection |
| Transdermal disk or patch | Medicated disk or patch absorbed through skin slowly over long period of time (e.g., 24 hours, 1 week) |
| Medication Forms Commonly Prepared for Administration by Parenteral Route | |
| Solution | Sterile preparation that contains water with one or more dissolved compounds |
| Powder | Sterile particles of medication that are dissolved in a sterile liquid (e.g., water, normal saline) before administration |
| Medication Forms Commonly Prepared for Instillation Into Body Cavities | |
| Intraocular disk | Small, flexible oval (similar to contact lens) consisting of two soft, outer layers and a middle layer containing medication; slowly releases medication when moistened by ocular fluid |
| Suppository | Solid dosage form mixed with gelatin and shaped in form of pellet for insertion into body cavity (rectum or vagina); melts when it reaches body temperature, releasing medication for absorption |
Pharmacokinetics As the Basis of Medication Actions
For medications to be therapeutic they must be taken into a patient’s body; be absorbed and distributed to cells, tissues, or a specific organ; and alter physiological functions. Pharmacokinetics is the study of how medications enter the body, reach their site of action, metabolize, and exit the body. Use knowledge of pharmacokinetics when timing medication administration, selecting the route of administration, considering the patient’s risk for alterations in medication action, and evaluating the patient’s response.
Absorption.
Absorption is the passage of medication molecules into the blood from the site of medication administration. Factors that influence absorption are the route of administration, ability of the medication to dissolve, blood flow to the site of administration, body surface area (BSA), and lipid solubility of medication.
Route of Administration.
Each route of medication administration has a different rate of absorption. When applying medications on the skin, absorption is slow because of the physical makeup of the skin. Medications placed on the mucous membranes and respiratory airways are absorbed quickly because these tissues contain many blood vessels. Because orally administered medications pass through the gastrointestinal (GI) tract, the overall rate of absorption is usually slow. Intravenous (IV) injection produces the most rapid absorption because medications are immediately available when they enter the systemic circulation.
Ability of the Medication to Dissolve.
The ability of an oral medication to dissolve depends largely on its form or preparation. The body absorbs solutions and suspensions already in a liquid state more readily than tablets or capsules. Acidic medications pass through the gastric mucosa rapidly. Medications that are basic are not absorbed before reaching the small intestine.
Blood Flow to the Site of Administration.
Medications are absorbed as blood comes in contact with the site of administration. The richer the blood supply to the site of administration, the faster the medication is absorbed.
Body Surface Area.
When a medication comes in contact with a large surface area, it is absorbed at a faster rate. This helps explain why the majority of medications are absorbed in the small intestine rather than the stomach.
Lipid Solubility.
Because the cell membrane has a lipid layer, highly lipid-soluble medications cross cell membranes easily and are absorbed quickly. Another factor that often affects medication absorption is whether or not food is in the stomach. Some oral medications are absorbed more easily when administered between meals because food changes the structure of a medication and sometimes impairs its absorption. When some medications are administered together, they interfere with one another, which impairs the absorption of both medications.
Safe medication administration requires knowledge of factors that alter or impair absorption of prescribed medications. You need an understanding of medication pharmacokinetics, the patient’s health history, the physical examination, and knowledge gained through daily interactions with patients. Use this knowledge to ensure that you administer medications at the correct time for best absorption. When medications interact with food, know which medications must be administered before or between meals or on an empty stomach. When medications interact with one another, ensure that they are not given at the same time. Consult and collaborate with the patient’s prescribers to ensure that the patient achieves the therapeutic effect of all medications. Before administering any medication, check pharmacology books, drug references, or package inserts or consult with pharmacists to identify medication-medication or medication-food interactions.
Distribution.
After a medication is absorbed, it is distributed within the body to tissues and organs and ultimately to its specific site of action. The rate and extent of distribution depend on the physical and chemical properties of the medication and the physiology of the person taking it.
Circulation.
Once a medication enters the bloodstream, it is carried throughout the tissues and organs. How fast it reaches the site depends on the vascularity of the various tissues and organs. Conditions that limit blood flow or blood perfusion inhibit the distribution of a medication. For example, patients with heart failure have impaired circulation, which slows medication delivery to the intended site of action. Therefore the efficacy of medications in these patients is often delayed or altered.
Membrane Permeability.
Membrane permeability refers to the ability of the medication to pass through tissues and membranes to enter target cells. To be distributed to an organ, a medication has to pass through all of the tissues and biological membranes of the organ. Some membranes serve as barriers to the passage of medications. For example, the blood-brain barrier allows only fat-soluble medications to pass into the brain and cerebral spinal fluid. Therefore central nervous system infections often require treatment with antibiotics injected directly into the subarachnoid space in the spinal cord. Some older patients experience adverse effects (e.g., confusion) as a result of the change in the permeability of the blood-brain barrier, with easier passage of fat-soluble medications. The placental membrane also has a nonselective barrier to medications. Fat-soluble and nonfat-soluble agents often cross the placenta and produce fetal deformities. After birth neonates often experience respiratory depression and withdrawal symptoms when their mothers use or abuse narcotics.
Protein Binding.
The degree to which medications bind to serum proteins such as albumin affects their distribution. Most medications partially bind to albumin. Medications bound to albumin cannot exert pharmacological activity. The unbound or “free” medication is its active form. Older adults have a decrease in albumin, probably caused by a change in liver function. The same is true for patients with liver disease or malnutrition. In both examples patients are at risk for an increase in medication activity, toxicity, or both.
Metabolism.
After a medication reaches its site of action, it becomes metabolized into a less active or inactive form that is easier to excrete. Biotransformation occurs under the influence of enzymes that detoxify, break down, and remove biologically active chemicals. Most biotransformation occurs within the liver, although the lungs, kidneys, blood, and intestines also metabolize medications. The liver is especially important because its specialized structure oxidizes and transforms many toxic substances. The liver degrades many harmful chemicals before they become distributed to the tissues. If a decrease in liver function occurs such as with aging or liver disease, a medication is usually eliminated more slowly, resulting in its accumulation. Patients are at risk for medication toxicity if organs that metabolize medications are not functioning correctly. For example, a small sedative dose of a barbiturate sometimes causes a patient with liver disease to lapse into a coma.
Excretion.
After medications are metabolized, they exit the body through the kidneys, liver, bowel, lungs, and exocrine glands. The chemical makeup of a medication determines the organ of excretion. Gaseous and volatile compounds such as nitrous oxide and alcohol exit through the lungs. Deep breathing and coughing (see Chapter 40) help patients eliminate anesthetic gases more rapidly after surgery. The exocrine glands excrete lipid-soluble medications. When medications exit through sweat glands, the skin often becomes irritated, requiring you to instruct patients in good hygiene practices (see Chapter 39). If a medication is excreted through the mammary glands, there is a risk that a nursing infant will ingest the chemicals. Check the safety of any medication used in breastfeeding women.
The GI tract is another route for medication excretion. Medications that enter the hepatic circulation are broken down by the liver and excreted into the bile. After chemicals enter the intestines through the biliary tract, the intestines resorb them. Factors that increase peristalsis (e.g., laxatives and enemas) accelerate medication excretion through the feces, whereas factors that slow peristalsis (e.g., inactivity and improper diet) often prolong the effects of a medication.
The kidneys are the main organs for medication excretion. Some medications escape extensive metabolism and exit unchanged in the urine. Others undergo biotransformation in the liver before the kidneys excrete them. If renal function declines, a patient is at risk for medication toxicity. When the kidney cannot adequately excrete a medication, it is necessary to reduce the dose. Maintenance of an adequate fluid intake (8 to 9 cups, or about 2 L of water/day) promotes proper elimination of medications for the average adult.
Types of Medication Action
Medications vary considerably in the way they act and their types of action. Patients do not always respond in the same way to each successive dose of a medication. Sometimes the same medication causes very different responses in different patients. Therefore it is essential to understand all the effects that medications have on patients.
Therapeutic Effects.
The therapeutic effect is the expected or predicted physiological response that a medication causes. Each medication has a desired therapeutic effect. For example, nitroglycerin reduces cardiac workload and increases myocardial oxygen supply. Some medications have more than one therapeutic effect. For example, prednisone, a steroid, decreases swelling, inhibits inflammation, reduces allergic responses, and prevents rejection of transplanted organs. Knowing the desired therapeutic effect for each medication allows you to provide patient education and accurately evaluate its desired effect.
Side Effects/Adverse Effects.
Every medication has a potential to harm a patient. Side effects are predictable and often unavoidable secondary effects produced at a usual therapeutic dose. They are either harmless or cause injury. For example, some antihypertensive medications cause impotence in men. If the side effects are serious enough to negate the beneficial effects of the therapeutic action of the medication, the prescriber discontinues the medication. Patients often stop taking medications because of side effects. Adverse effects are unintended, undesirable, and often unpredictable severe responses to medication. Some adverse effects are immediate, whereas others take weeks or months to develop. Early recognition is important. When adverse responses to medications occur, the prescriber discontinues the medication immediately. Health care providers report adverse effects to the FDA using the MedWatch program (USFDA, 2010).
Toxic Effects.
Toxic effects develop after prolonged intake of a medication or when a medication accumulates in the blood because of impaired metabolism or excretion. Excess amounts of a medication within the body sometimes have lethal effects, depending on its action. For example, toxic levels of morphine, an opioid, cause severe respiratory depression and death. Antidotes are available to treat specific types of medication toxicity. For example, naloxone (Narcan), an opioid antagonist, reverses the effects of opioid toxicity.
Idiosyncratic Reactions.
Medications sometimes cause unpredictable effects such as an idiosyncratic reaction, in which a patient overreacts or underreacts to a medication or has a reaction different from normal. For example, a child who receives diphenhydramine (Benadryl), an antihistamine, becomes extremely agitated or excited instead of drowsy. It is not always possible to predict if a patient will have an idiosyncratic response to a medication.
Allergic Reactions.
Allergic reactions also are unpredictable responses to a medication. Some patients become immunologically sensitized to the initial dose of a medication. With repeated administration the patient develops an allergic response to it, its chemical preservatives, or a metabolite. The medication or chemical acts as an antigen, triggering the release of the antibodies in the body. A patient’s medication allergy symptoms vary, depending on the individual and the medication (Table 31-2). Among the different classes of medications, antibiotics cause a high incidence of allergic reactions. Severe or anaphylactic reactions, which are life threatening, are characterized by sudden constriction of bronchiolar muscles, edema of the pharynx and larynx, and severe wheezing and shortness of breath. Immediate medical attention is required to treat anaphylactic reactions. A patient with a known history of an allergy to a medication needs to avoid exposure to that medication in the future and wear an identification bracelet or medal (Fig. 31-1), which alerts nurses and physicians to the allergy if the patient is unconscious when receiving medical care.
TABLE 31-2
| SYMPTOM | DESCRIPTION |
| Urticaria | Raised, irregularly shaped skin eruptions with varying sizes and shapes; eruptions have reddened margins and pale centers |
| Rash | Small, raised vesicles that are usually reddened; often distributed over entire body |
| Pruritus | Itching of skin; accompanies most rashes |
| Rhinitis | Inflammation of mucous membranes lining nose; causes swelling and clear, watery discharge |
Medication Interactions
When one medication modifies the action of another, a medication interaction occurs. Medication interactions are common in individuals taking several medications. Some medications increase or diminish the action of others and may alter the way another medication is absorbed, metabolized, or eliminated from the body. When two medications have a synergistic effect, their combined effect is greater than the effect of the medications when given separately. For example, alcohol is a central nervous system depressant that has a synergistic effect on antihistamines, antidepressants, barbiturates, and narcotic analgesics. Sometimes a medication interaction is desired. Prescribers often combine medications to create an interaction that has a beneficial effect. For example, a patient with high blood pressure takes several medications such as diuretics and vasodilators that act together to control the blood pressure when one medication is not effective on its own.
Timing of Medication Dose Responses
Medications administered intravenously enter the bloodstream and act immediately, whereas medications given in other routes take time to enter the bloodstream and have an effect. The quantity and distribution of a medication in different body compartments change constantly. Medications are ordered at various times, depending on when their response begins, becomes most intense, and ceases.
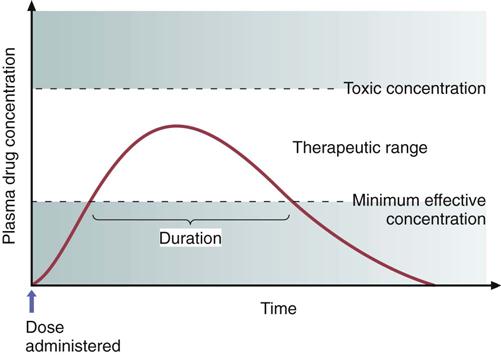
The minimum effective concentration (MEC) is the plasma level of a medication below which the effect of the medication does not occur. The toxic concentration is the level at which toxic effects occur. When a medication is prescribed, the goal is to achieve a constant blood level within a safe therapeutic range, which falls between the MEC and the toxic concentration (Fig. 31-2). When a medication is administered repeatedly, its serum level fluctuates between doses. The highest level is called the peak concentration, and the lowest level is called the trough concentration. After reaching its peak, the serum concentration of the medication falls progressively. With IV infusions the peak concentration occurs quickly, but the serum level also begins to fall immediately. Some medication doses (e.g., vancomycin) are based on peak and trough serum levels. The trough level is generally drawn 30 minutes before administering the drug, and the peak level is drawn whenever the drug is expected to reach its peak concentration. The time it takes for a drug to reach its peak concentration varies, depending on the pharmacokinetics of the medication.
All medications have a biological half-life, which is the time it takes for excretion processes to lower the amount of unchanged medication by half. A medication with a short half-life needs to be given more frequently than a medication with a longer half-life. The half-life does not change, no matter how much medication is given. For example, if the nurse gives 1 g of a medication that has a half-life of 8 hours, the patient excretes 500 mg of the medication in 8 hours. In the next 8 hours the patient excretes 250 mg. This process continues until the medication is totally eliminated from the body.
To maintain a therapeutic plateau the patient must receive regular fixed doses. For example, current evidence shows that pain medications are most effective when they are given around the clock (ATC) rather than when the patient intermittently complains of pain because ATC allows the body to maintain an almost constant level of pain medication. After an initial medication dose, the patient receives each successive dose when the previous dose reaches its half-life.
Safe drug administration involves adherence to prescribed doses and dosage schedules (Table 31-3). Some agencies set schedules for medication administration. However, nurses are able to alter this schedule based on knowledge about a medication. For example, at some agencies medications that are to be taken once a day are given at 9:00 AM. However, if a medication works best when given before bedtime, the nurse administers it before the patient goes to sleep. In addition, acute care agencies use guidelines from the Institute for Safe Medication Practices (CMS, 2011; ISMP, 2011) to determine safe, effective, and timely administration of scheduled medications. According to the ISMP guidelines, hospitals need to determine which medications are time-critical and which are non–time-critical. Time-critical medications are medications in which early or delayed administration of maintenance doses (more than 30 minutes before or after the scheduled dose) will most likely cause harm or result in subtherapeutic responses in a patient. Non–time-critical medications include medications in which the timing of administration will most likely not affect the desired effect of the medication if given 1 to 2 hours before or after its scheduled time. You need to administer time-critical medications at a precise time or within 30 minutes before or after the scheduled time. You administer medications identified as non–time-critical within 1 to 2 hours of their scheduled time. Follow your agency’s medication administration policies about the timing of medications to ensure you administer medications at the right time (CMS, 2011; ISMP, 2011).
TABLE 31-3
Common Dosage Administration Schedules
| DOSAGE SCHEDULE | ABBREVIATION |
| Before meals | AC, ac |
| As desired | ad lib |
| At bedtime | “nightly” or “at bedtime” |
| After meals | PC, pc |
| Whenever there is a need | prn |
| Every morning, every AM | qAM |
| Every day | Daily |
| Give immediately | STAT, stat |
When teaching patients about dosage schedules, use language that is familiar to the patient. For example, when teaching a patient about medication dosing twice a day, instruct him or her to take it in the morning and again in the evening. Use knowledge about the time intervals and terms used to describe medication actions to anticipate the effect of a medication and educate the patient about when to expect a response (Table 31-4).
TABLE 31-4
Terms Associated with Medication Actions
| TERM | MEANING |
| Onset | Time it takes after a medication is administered for it to produce a response |
| Peak | Time it takes for a medication to reach its highest effective concentration |
| Trough | Minimum blood serum concentration of medication reached just before the next scheduled dose |
| Duration | Time during which the medication is present in concentration great enough to produce a response |
| Plateau | Blood serum concentration of a medication reached and maintained after repeated fixed doses |
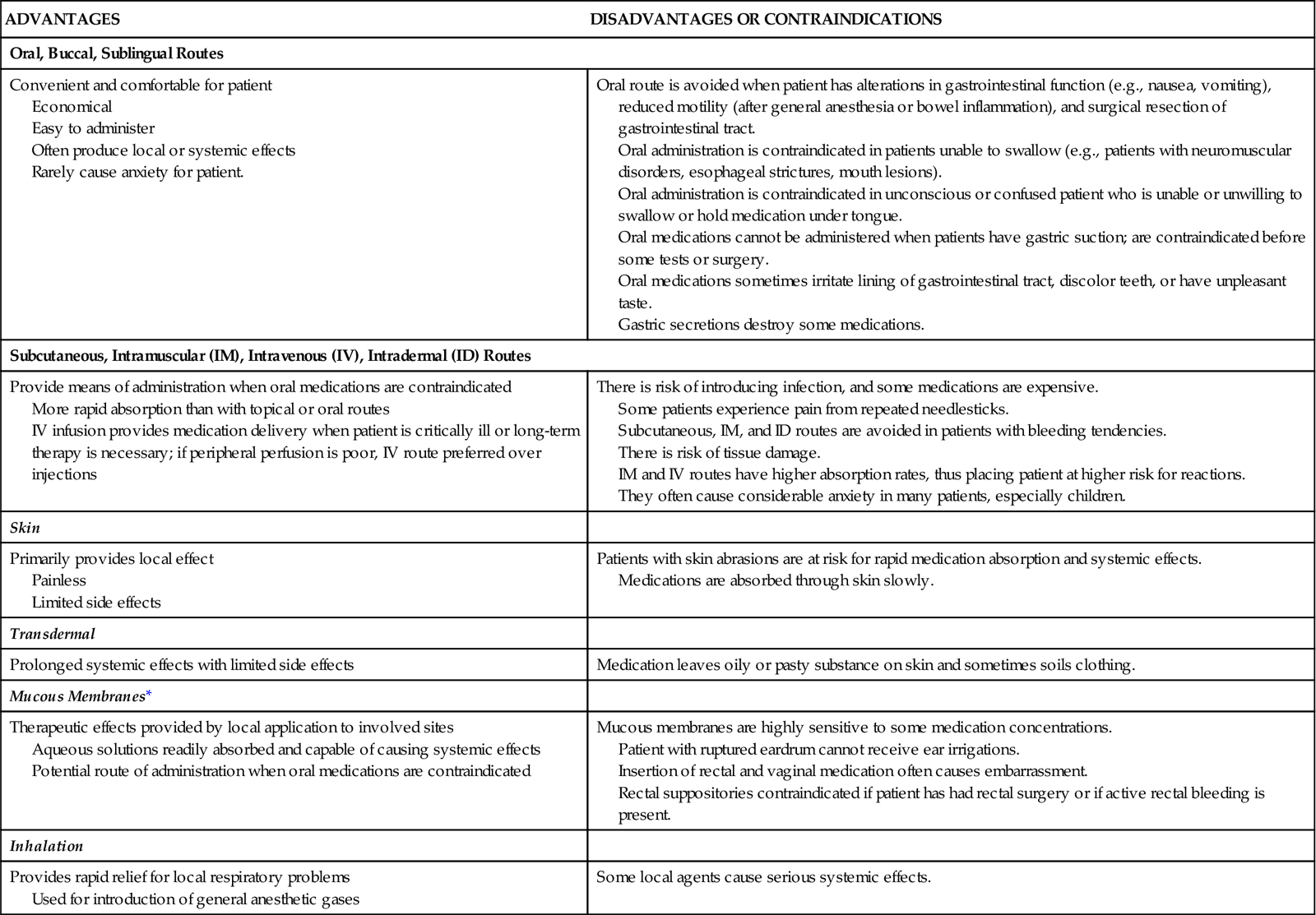
Routes of Administration
The route prescribed for administering a medication depends on the properties and desired effect of the medication and the patient’s physical and mental condition (Table 31-5). Work with the prescriber in determining the best route for a patient’s medication.
TABLE 31-5
Factors Influencing Choice of Administration Routes
| ADVANTAGES | DISADVANTAGES OR CONTRAINDICATIONS |
| Oral, Buccal, Sublingual Routes | |
| Convenient and comfortable for patient Economical Easy to administer Often produce local or systemic effects Rarely cause anxiety for patient. | Oral route is avoided when patient has alterations in gastrointestinal function (e.g., nausea, vomiting), reduced motility (after general anesthesia or bowel inflammation), and surgical resection of gastrointestinal tract. Oral administration is contraindicated in patients unable to swallow (e.g., patients with neuromuscular disorders, esophageal strictures, mouth lesions). Oral administration is contraindicated in unconscious or confused patient who is unable or unwilling to swallow or hold medication under tongue. Oral medications cannot be administered when patients have gastric suction; are contraindicated before some tests or surgery. Oral medications sometimes irritate lining of gastrointestinal tract, discolor teeth, or have unpleasant taste. Gastric secretions destroy some medications. |
| Subcutaneous, Intramuscular (IM), Intravenous (IV), Intradermal (ID) Routes | |
| Provide means of administration when oral medications are contraindicated More rapid absorption than with topical or oral routes IV infusion provides medication delivery when patient is critically ill or long-term therapy is necessary; if peripheral perfusion is poor, IV route preferred over injections | There is risk of introducing infection, and some medications are expensive. Some patients experience pain from repeated needlesticks. Subcutaneous, IM, and ID routes are avoided in patients with bleeding tendencies. There is risk of tissue damage. IM and IV routes have higher absorption rates, thus placing patient at higher risk for reactions. They often cause considerable anxiety in many patients, especially children. |
| Skin | |
| Primarily provides local effect Painless Limited side effects | Patients with skin abrasions are at risk for rapid medication absorption and systemic effects. Medications are absorbed through skin slowly. |
| Transdermal | |
| Prolonged systemic effects with limited side effects | Medication leaves oily or pasty substance on skin and sometimes soils clothing. |
| Mucous Membranes* | |
| Therapeutic effects provided by local application to involved sites Aqueous solutions readily absorbed and capable of causing systemic effects Potential route of administration when oral medications are contraindicated | Mucous membranes are highly sensitive to some medication concentrations. Patient with ruptured eardrum cannot receive ear irrigations. Insertion of rectal and vaginal medication often causes embarrassment. Rectal suppositories contraindicated if patient has had rectal surgery or if active rectal bleeding is present. |
| Inhalation | |
| Provides rapid relief for local respiratory problems Used for introduction of general anesthetic gases | Some local agents cause serious systemic effects. |
Oral Routes.
The oral route is the easiest and the most commonly used route. Medications are given by mouth and swallowed with fluid. Oral medications have a slower onset of action and a more prolonged effect than parenteral medications. Patients generally prefer the oral route.
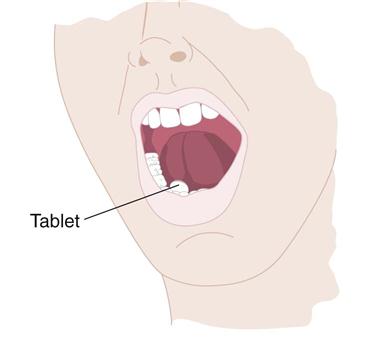
Sublingual Administration.
Some medications are readily absorbed after being placed under the tongue to dissolve (Fig. 31-3). A medication given by the sublingual route should not be swallowed because the medication does not have the desired effect. Nurses often give nitroglycerin by the sublingual route. Tell the patient not to drink anything until the medication is completely dissolved.
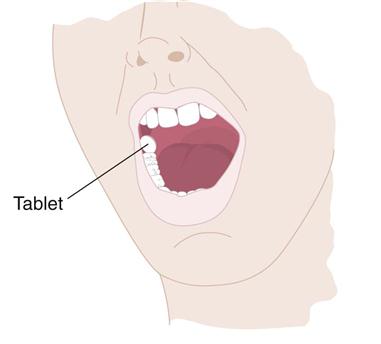
Buccal Administration.
Administration of a medication by the buccal route involves placing the solid medication in the mouth against the mucous membranes of the cheek until it dissolves (Fig. 31-4). Teach patients to alternate cheeks with each subsequent dose to avoid mucosal irritation. Warn patients not to chew or swallow the medication or to take any liquids with it. A buccal medication acts locally on the mucosa or systemically as it is swallowed in a person’s saliva.
Parenteral Routes.
Parenteral administration involves injecting a medication into body tissues. The following are the four major sites of injection:
1. Intradermal (ID): Injection into the dermis just under the epidermis
2. Subcutaneous: Injection into tissues just below the dermis of the skin
3. Intramuscular (IM): Injection into a muscle
Some medications are administered into body cavities other than the four types listed here. These additional routes include epidural, intrathecal, intraosseous, intraperitoneal, intrapleural, and intraarterial. Nurses usually are not responsible for the administration of medications through these advanced techniques. Whether or not you actually administer the medication, you remain responsible for monitoring the integrity of the medication delivery system, understanding the therapeutic value of the medication, and evaluating the patient’s response to the therapy.
Epidural.
Epidural medications are administered in the epidural space via a catheter, which is placed by a nurse anesthetist or an anesthesiologist. This route is used for the administration of regional analgesia for surgical procedures (see Chapter 43). Nurses who have advanced education in the epidural route can administer medications by continuous infusion or by a bolus dose.
Intrathecal.
Physicians and specially educated nurses administer intrathecal medications through a catheter placed in the subarachnoid space or one of the ventricles of the brain. Intrathecal administration is often associated with long-term medication administration through surgically implanted catheters.
Intraosseous.
This method of medication administration involves the infusion of medication directly into the bone marrow. It is most commonly used in infants and toddlers who have poor access to their intravascular space and when an emergency arises and IV access is impossible.
Intraperitoneal.
Medications administered into the peritoneal cavity are absorbed into the circulation. Chemotherapeutic agents, insulin, and antibiotics are administered in this fashion.
Intrapleural.
A syringe and needle or a chest tube is used to administer intrapleural medications directly into the pleural space. Chemotherapeutic agents are the most common medications administered via this method. Physicians also instill medications that help resolve persistent pleural effusion. This is called pleurodesis, which promotes adhesion between the visceral and parietal pleura.
Intraarterial.
Intraarterial medications are administered directly into the arteries. Intraarterial infusions are common in patients who have arterial clots. The nurse manages a continuous infusion of clot-dissolving agents and carefully monitors the integrity of the infusion to prevent inadvertent disconnection of the system and subsequent bleeding.
Other methods of medication administration that are usually limited to physician administration are intracardiac, an injection of a medication directly into cardiac tissue, and intraarticular, an injection of a medication into a joint.
Topical Administration.
Medications applied to the skin and mucous membranes generally have local effects. You apply topical medications to the skin by painting or spreading the medication over an area, applying moist dressings, soaking body parts in a solution, or giving medicated baths. Systemic effects often occur if a patient’s skin is thin or broken down, the medication concentration is high, or contact with the skin is prolonged. A transdermal disk or patch (e.g., nitroglycerin, scopolamine, and estrogens) has systemic effects. The disk secures the medicated ointment to the skin. These topical applications are left in place for as little as 12 hours or as long as 7 days.
Nurses administer medications to mucous membranes in a variety of ways, including the following, by:
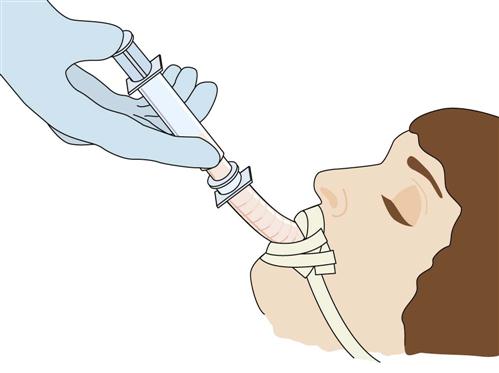
Inhalation Route.
The deeper passages of the respiratory tract provide a large surface area for medication absorption. Nurses administer inhaled medications through the nasal and oral passages or endotracheal or tracheostomy tubes. Endotracheal tubes enter the patient’s mouth and end in the trachea (Fig. 31-5), whereas tracheostomy tubes enter the trachea directly through an incision made in the neck. Inhaled medications are readily absorbed and work rapidly because of the rich vascular alveolar capillary network present in the pulmonary tissue. Many inhaled medications have local or systemic effects.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree