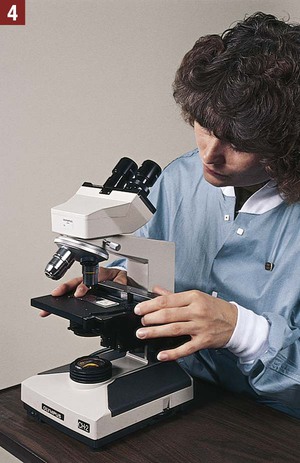
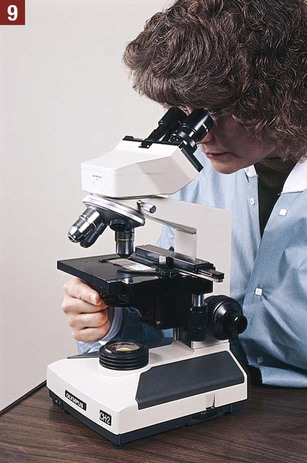
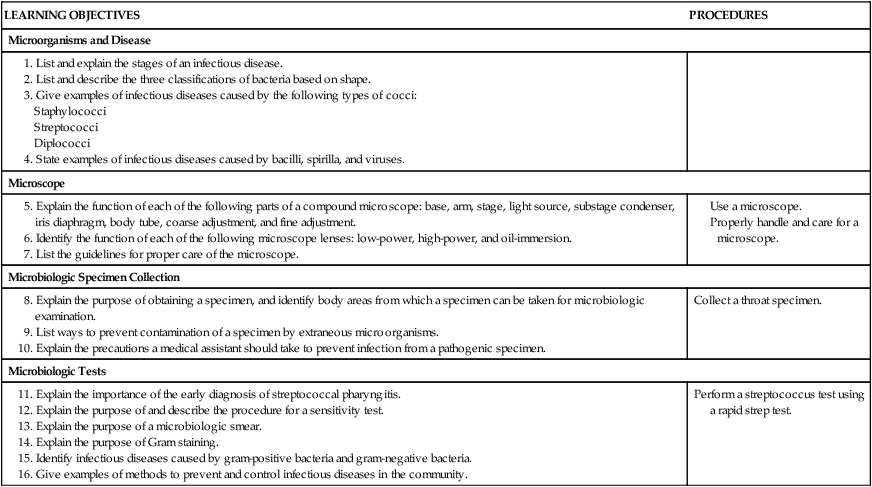
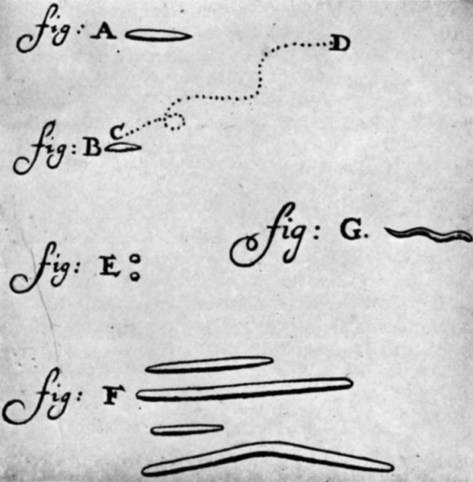
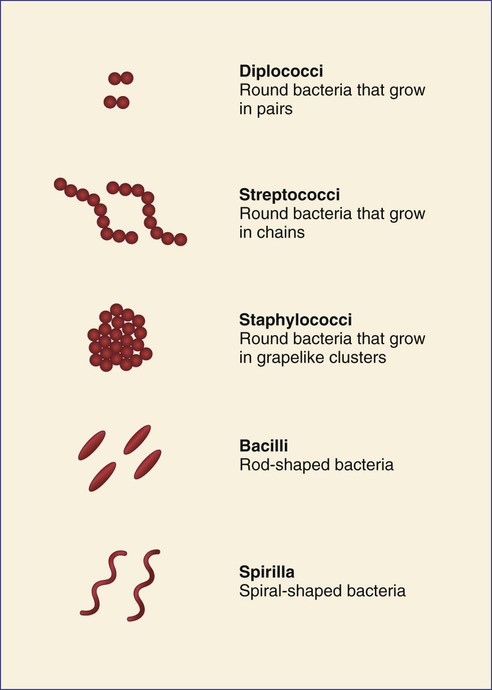
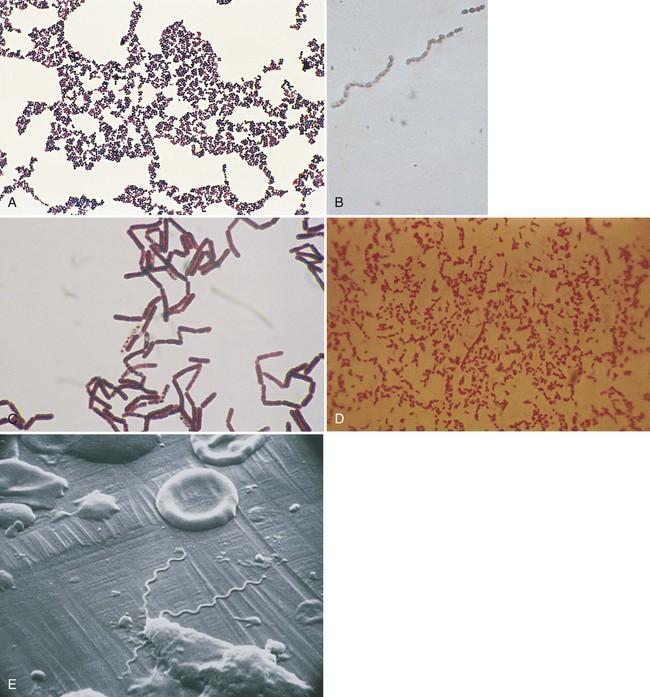
Microbiology is the scientific study of microorganisms and their activities. As described in Chapter 17, microorganisms are tiny living plants and animals that cannot be seen by the naked eye, but must be viewed under a microscope. Anton van Leeuwenhoek (1632-1723) designed a magnifying glass strong enough for viewing microorganisms. He was the first individual to observe and describe protozoa and bacteria (Figure 34-1). Leeuwenhoek’s magnifying glass was the precursor of modern microscopes used today to study microorganisms. A microscope allows the observer to see individual microbial cells and to differentiate and identify microorganisms. This chapter provides an introduction to microbiology, including a description of proper microbiologic collection and handling techniques that must be followed to ensure a high-quality specimen. Identification of a pathogen using microbial culturing, biochemical testing, and microscopy is also discussed in this chapter. DNA testing to detect pathogens (e.g., chlamydia and gonorrhea) was previously described in Chapter 23. Before undertaking this study, the medical assistant should review Chapter 17, which discusses introductory concepts that are basic to this chapter. Invasion of the body by pathogenic microorganisms is known as infection. Under conditions favorable to the pathogens, they grow and multiply, resulting in an infectious disease (also known as a communicable disease) that produces harmful effects on the host. Not all pathogens that enter a host are able to cause disease, however. When a pathogen enters the body, it attempts to invade the tissues so that it can grow and multiply. The body tries to stop the invasion with its second line of natural defense mechanisms,* which includes inflammation, phagocytosis by white blood cells, and the production of antibodies. These defense mechanisms work to destroy the pathogen and remove it from the body. If the body is successful, the pathogens are destroyed, and the individual experiences no adverse effects. If the pathogen is able to overcome the body’s natural defense mechanisms, an infectious disease results. Droplet infection refers to an infection that is indirectly transmitted by tiny contaminated droplets of moisture expelled from the upper respiratory tract of an infected individual. When an individual exhales (as during breathing, talking, coughing, or sneezing), a fine spray of moisture droplets is emitted by that individual from the upper respiratory tract. If the individual has a contagious disease that is transmitted by droplet infection, the pathogens are carried into the air by these tiny moisture droplets. Another individual may inhale these contaminated droplets and become infected with the disease. To help prevent the spread of droplet infections, contagious individuals should cover their mouths and noses while coughing or sneezing. See Figure 17-1 for examples of other means of pathogen transmission. 1. The infection is the invasion and multiplication of pathogenic microorganisms in the body. 2. The incubation period is the interval of time between the invasion by a pathogenic microorganism and the appearance of the first symptoms of the disease. Depending on the type of disease, the incubation period may range from a few days to several months. During this time, the pathogen is growing and multiplying. 3. The prodromal period is a short period in which the first symptoms that indicate an approaching disease occur. Headache and a feeling of illness are common prodromal symptoms. 4. The acute period is when the disease is at its peak and symptoms are fully developed. Fever is a common symptom of many infectious diseases. 5. The decline period is when symptoms of the disease begin to subside. 6. The convalescent period is the stage in which the patient regains strength and returns to a state of good health. Bacteria can be classified according to their shape into three basic groups (Figure 34-2). Round bacteria are known as cocci. Cocci can be categorized further as diplococci, streptococci, or staphylococci, depending on their pattern of growth. Rod-shaped bacteria are bacilli. Spiral and curve-shaped bacteria are spirilla, and they include spirochetes and vibrios. Staphylococci are round bacteria that grow in grapelike clusters (Figure 34-3, A). The species Staphylococcus epidermidis is widely distributed and is normally present on the surface of the skin and the mucous membranes of the mouth, nose, throat, and intestines. S. epidermidis is usually nonpathogenic; however, a cut, abrasion, or other break in the skin can allow invasion of the tissues by the organism, resulting in a mild infection. Streptococci are round bacteria that grow in chains (Figure 34-3, B). Before the advent of antibiotics, streptococcal infections were a major cause of human death. Diseases caused by streptococci include streptococcal sore throat (“strep throat”), scarlet fever, rheumatic fever, pneumonia, puerperal sepsis, erysipelas, and skin conditions such as carbuncles and impetigo. Bacilli are rod-shaped bacteria that are frequently found in the soil and air (Figure 34-3, C). Some bacilli are able to form spores, a characteristic that enables them to resist adverse conditions such as heat and disinfectants. Diseases caused by bacilli include botulism, tetanus, gas gangrene, gastroenteritis produced by Salmonella food poisoning, typhoid fever, pertussis (whooping cough), bacillary dysentery, diphtheria, tuberculosis, leprosy, and plague. Escherichia coli is a species of bacillus that is found among the normal flora of the large intestine in enormous numbers (Figure 34-3, D). It is normally a harmless bacterium; however, if it enters the urinary tract as a result of lowered resistance, poor hygiene practices, or both, it may cause a urinary tract infection. Spirilla are spiral or curve-shaped bacteria. Treponema pallidum, a spirochete, is the causative agent of syphilis (Figure 34-3, E). This microorganism cannot be grown in commonly available culture media; the diagnosis of syphilis is generally made using serologic tests. A serologic test is performed on the serum of the blood. Cholera is caused by another type of spirillum, Vibrio cholerae. Immunization and proper methods of sanitation and water purification have all but eliminated cholera in the United States. Many kinds of microscopes are available, but the type used most often for office laboratory work is the compound microscope. The compound microscope consists of a two-lens system, and the magnification of one system is increased by the other. A source of bright light is required for proper illumination of the object to be viewed. This combination of lenses and light permits visualization of structures that cannot be seen with the unaided eye, such as microorganisms and cellular forms. The compound microscope consists of two main components—the support system and the optical system. The medical assistant should be able to identify the parts of a microscope (Figure 34-4) and should be able to use and care for it properly. Procedure 34-1 outlines the correct use and care of a microscope.
Medical Microbiology
Introduction to Microbiology
Infection
Stages of an Infectious Disease
Microorganisms and Disease
Bacteria
Cocci
Bacilli
Spirilla
Microscope
Get Clinical Tree app for offline access

Medical Microbiology
Get Clinical Tree app for offline access