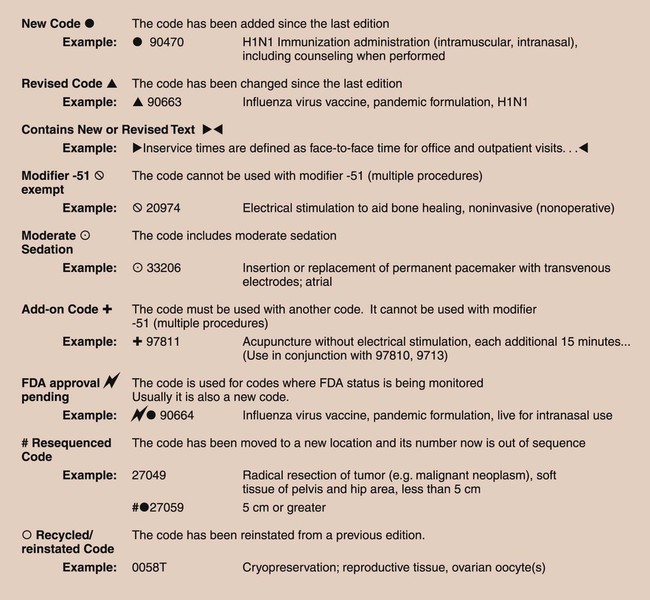
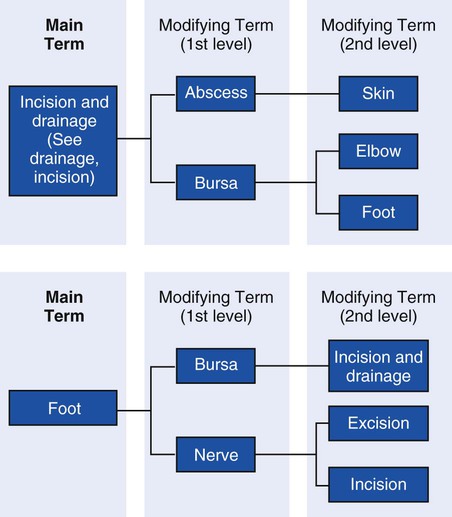
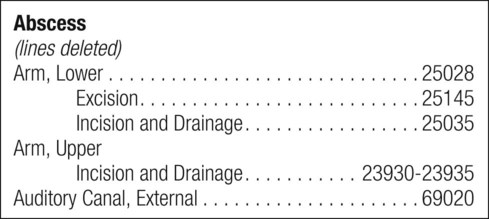
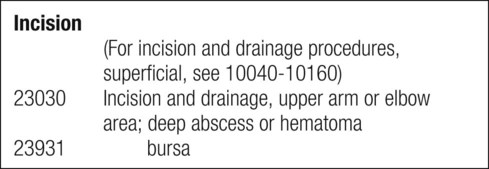
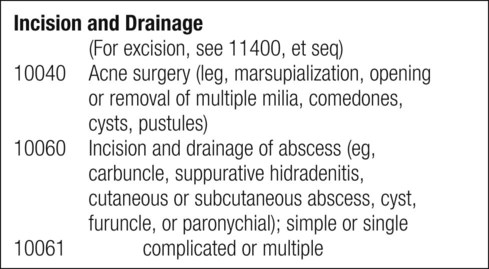
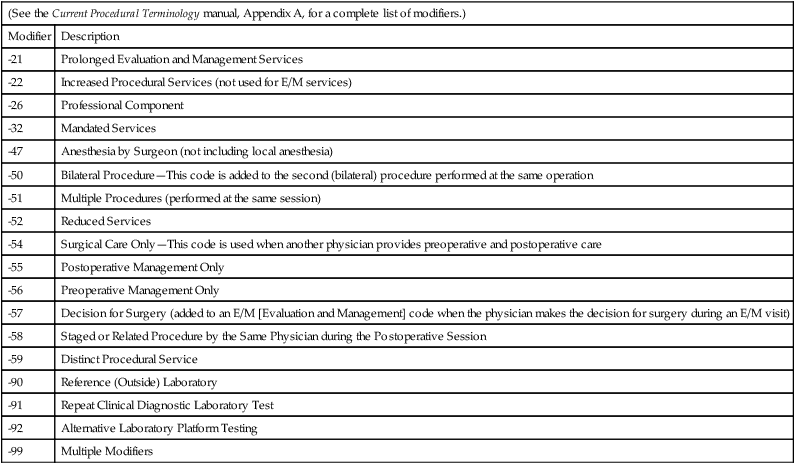
1. To justify medical services to insurance companies by correlating procedures to diagnosis 2. To collect statistics about the outcome and effectiveness of treatments 3. To help physicians and hospitals set fees based on the amount of time and skill required to provide a specific service The fourth edition of the CPT, first published in 1977, became the standard for insurance billing in the early 1980s, when it was used as the basis for a Medicare procedure coding system, the Healthcare Common Procedure Coding System (HCPCS), pronounced “hick-picks.” Medicare, the government insurance program for the elderly and disabled, is administered by the Centers for Medicare and Medicaid Services (CMS). It will be discussed in detail in Chapter 46. In each annual update of the CPT, new codes may be added for new procedures, old codes may be dropped for procedures no longer in use, and modifications may be made to current procedures. A darkened circle in front of a code indicates that the code is new. A darkened triangle in front of the code indicates that the description for the code has been changed or modified (Figure 45-1). The medical assistant must familiarize himself or herself with the important revisions each year when the new codes are published. In addition, codes must be updated in the office computer system and on office forms such as charge slips to be sure that insurance is billed correctly. The main body of the CPT manual is organized by section, then subsection, subheading, and finally category, each providing a finer level of detail. The back of the manual contains an alphabetic index of procedures. The most common procedures performed in a given office are usually found on the charge slip and in the computer billing program. In the office itself, the provider usually checks off the codes for common procedures done during a patient visit and writes in the name of procedures not found on the charge slip. However, the patient may be billed from the medical office for services provided in another setting—for example, when a physician visits a patient in the hospital during morning rounds, when he or she examines a patient in the emergency room or a nursing home, and when he or she performs surgery in the hospital or an outpatient surgery setting. In most locations the office bills only for office services. If the office bills for labwork done by an outside reference lab, this must be indicated on the insurance form (see Chapter 46). Several appendices follow the Category III codes as indicated in the following list: Appendix B—Additions, Deletions, Revisions Appendix C—Clinical Examples for E/M Codes Appendix E—Modifier -51 Exempt codes Appendix F—Modifier -63 Exempt codes Appendix G—Moderate Sedation codes Appendix H—Alphabetical Clinical Topics Listing (removed and now only on the AMA website) Appendix I—Genetic Testing Modifiers Appendix J—Electrodiagnostic Medicine Listing of Sensory, Motor and Mixed Nerves Appendix K—Product Pending FDA Approval A modifier is an addition to a procedure code that indicates unusual circumstances related to the procedure, such as a more extensive procedure or two procedures performed in the same session. All modifiers are listed in Appendix A. The two-digit modifier can be added to the main code after a hyphen. The modifier can also be written as a separate five-digit code for electronic billing. The five-digit modifier always begins with 099 and ends with the two digits of the modifier (Table 45-1). Table 45-1 Selected CPT Modifiers Used in the Medical Office It may be necessary to look up the procedure in several ways to locate the correct code. In the index, procedures may be located by looking under the name of the procedure, the anatomic location, and sometimes the diagnosis. The terms are arranged alphabetically with the main term in boldface type and modifying terms arranged below the main term. Each level of modifying term is indented further than the level above it. For example, the main term may be an anatomic location, such as the foot. The first modifying term would identify either a condition, an anatomic location, or a procedure (such as Lesion, Nerve, or Repair). When a procedure is listed in the index (as the main term or any level of modifying term), it is followed by a code or range of codes (e.g., Foot, Nerve, Excision …… 28055). Both main terms and modifying terms may point to a cross-reference using the word See. (See Figure 45-2.) Several pieces of information may be significant when choosing the correct code for a procedure: There are two types of CPT codes: stand-alone codes and indented codes. The stand-alone code contains a semicolon (e.g., 93000 Electrocardiogram, routine ECG with at least 12 leads; with interpretation and report). The indented code, which follows a stand-alone code or another indented code, provides only text to replace the words after the semicolon in the stand-alone code (e.g., 93005 [indent] tracing only, without interpretation and report). In the example given, the code 93000 would be used if the ECG tracing is made and the physician interprets the tracing in the same medical office. The code 93005 would be used if the ECG tracing is made in one office, but insurance should not be billed for the interpretation because it will be done by another physician and billed from another office (Procedure 45-1). 1. For coding purposes, the patient is either an established patient (one who has been seen in the previous 3 years) or a new patient (one who has not had services performed by any provider in the medical office in the previous 3 years). There are separate groups of codes for each type of patient. New patients are expected to take longer to examine and are reimbursed at a higher rate. The patient is also either an outpatient (one who has not been admitted to a health care facility) or an inpatient (a patient who has been formally admitted to a health care facility). Although most services for patients who are inpatients are billed by the health care facility itself, physicians who are not employees of that facility bill for visits to the patient during a hospital admission, for inpatient consultations, for providing reports for some diagnostic tests performed at the hospital (such as cardiac stress tests), for critical care and intensive care services, as well as care for visits to patients in nursing homes. 2. There are separate groups of codes, depending on where the service is provided and whether the physician is the patient’s primary care provider or a consultant. A medical service could have been provided in the office, in a nursing home, in a hospital to a patient who has been admitted, or in a hospital emergency department. The E/M section of the CPT manual is divided into several subsections, and it is important to select a code from the correct subsection, depending on the service that the physician provided and the location where the service was provided. 3. The level of service depends primarily on three key factors: • A problem-focused history is one that addresses the chief complaint, with a brief history of the illness or problem. • An expanded problem-focused history addresses the chief complaint, a brief history of the present illness or problem, and a review of systems that have to do with the chief complaint. • A detailed history addresses the chief complaint, an extended history of the present illness, and a review of body systems, including other systems beyond those related to the chief complaint. Family history is also reviewed as it relates to the present problem. • A comprehensive history includes a chief complaint; an extended history of the present illness; a review of all body systems, especially those directly related to the present problem; and a complete family history. • A problem-focused examination is limited to the affected body system or organ. • An expanded problem-focused examination is related to the affected body system, as well as other organs or systems that might be symptomatic. For example, the patient may be followed for angina (recurrent chest pain) and have a new complaint of calf pain when walking. • A detailed examination includes the affected body systems or organs and other related systems or organs. • A comprehensive examination is a multisystem examination, or a complete examination of one system. Medical decision making can be straightforward or have a low, moderate, or high level of complexity. If a patient has one problem, medical decision making is usually straightforward. When a patient has multiple problems, especially if they are causing severe or life-threatening symptoms, the decision-making process is more complex. For example, if a new patient has poorly controlled diabetes mellitus type 1, fever, and an increased white blood count, the decision-making process for the physician would be highly complex (Figure 45-3).
Medical Coding
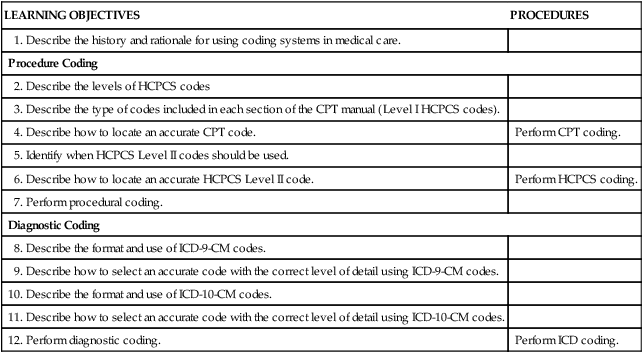
LEARNING OBJECTIVES
PROCEDURES
1. Describe the history and rationale for using coding systems in medical care.
Procedure Coding
2. Describe the levels of HCPCS codes
3. Describe the type of codes included in each section of the CPT manual (Level I HCPCS codes).
4. Describe how to locate an accurate CPT code.
Perform CPT coding.
5. Identify when HCPCS Level II codes should be used.
6. Describe how to locate an accurate HCPCS Level II code.
Perform HCPCS coding.
7. Perform procedural coding.
Diagnostic Coding
8. Describe the format and use of ICD-9-CM codes.
9. Describe how to select an accurate code with the correct level of detail using ICD-9-CM codes.
10. Describe the format and use of ICD-10-CM codes.
11. Describe how to select an accurate code with the correct level of detail using ICD-10-CM codes.
12. Perform diagnostic coding.
Perform ICD coding.
Introduction to Coding
Procedure Coding
Levels of Procedure Codes
CPT Manual
Sections of the CPT Manual
Evaluation and Management
99201 to 99499
Anesthesia
00100 to 01999, 99100 to 09140
Surgery
10021 to 69990
Radiology
70010 to 79999
Pathology and Laboratory
80047 to 89356
Medicine
90281 to 99199, 99500 to 99607
Appendices
(See the Current Procedural Terminology manual, Appendix A, for a complete list of modifiers.)
Modifier
Description
-21
Prolonged Evaluation and Management Services
-22
Increased Procedural Services (not used for E/M services)
-26
Professional Component
-32
Mandated Services
-47
Anesthesia by Surgeon (not including local anesthesia)
-50
Bilateral Procedure—This code is added to the second (bilateral) procedure performed at the same operation
-51
Multiple Procedures (performed at the same session)
-52
Reduced Services
-54
Surgical Care Only—This code is used when another physician provides preoperative and postoperative care
-55
Postoperative Management Only
-56
Preoperative Management Only
-57
Decision for Surgery (added to an E/M [Evaluation and Management] code when the physician makes the decision for surgery during an E/M visit)
-58
Staged or Related Procedure by the Same Physician during the Postoperative Session
-59
Distinct Procedural Service
-90
Reference (Outside) Laboratory
-91
Repeat Clinical Diagnostic Laboratory Test
-92
Alternative Laboratory Platform Testing
-99
Multiple Modifiers
Looking up CPT Codes in the Index
Selecting a Specific CPT Code
Evaluation and Management
Medical History
Physical Examination
Medical Decision Making
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Medical Coding
Get Clinical Tree app for offline access