Under this layer the mesoderm differentiates into connective tissue and models into extensive blood vessel networks.
Clusters of cells which will form tooth buds appear in the jaws.
Eyelids form and fuse.
The connective tissue differentiates into dermis; a loose, continuous layer over a dense continuous layer; further differentiation will result in the subcutaneous layer. Adipose cells accumulate.
The neural crest cells, melanocytes, which will eventually pigment the skin, migrate into the epithelium (the infant is not fully pigmented at birth).
The ectoderm supports the development of nails, hair follicles (early hair growth is called lanugo) and sebaceous glands.
Nails begin to form as small thickenings of ectodermal epidermis near the tips of the digits; finger nails precede toe nails.
The eyes can open from weeks 24–25, although layered; the skin is so thin it appears transparent. Fingerprints are forming.
Skin is much more than a surface. Its colour, texture and condition are accurate indicators of a child’s health and wellbeing. The way young people manage and modify their skin can depict their level of self-esteem for skin is central to body image. Many of the conditions children come into ITU with result in scarring which will have lifelong ramifications for them.
Anatomy and Physiology of the Skin
The skin is a highly complex structure and only a brief overview is given here.
The skin is the largest organ in the body, covering the entire surface. By adulthood it weighs 2.5–3 kg. It serves as a protective barrier against heat, light, injury and infection, and skin also:
- thermoregulates;
- has a role in the fluid balance of the body;
- acts as a repository for fat and vitamin D, which has an important role in calcium homeostasis;
- has a role in sensory perception.
The skin is innervated with approximately 1 million afferent nerve fibres. The majority supply the face; relatively few populate the back. The cutaneous nerves contain axons with cell bodies in the dorsal root ganglia. The main nerve trunks entering the subdermal tissue and divide into smaller branches to form a network which usually follows the blood vessel pattern and forms a mesh of nerves in the dermis where they terminate as most do not extend into the epidermis. The skin is not uniform over the surface of the body, for example the head contains the most hair follicles, the palms of the hand and the soles of the feet contain none; areas which are modelled to endure high friction, such as the palms and soles, have thick layers.
The epidermis is the outermost layer and is a multi-layered structure. Stratified epithelium is renewed continuously by cellular division from the basal layer. The cells produced by mitosis in the basal layer ascend towards the surface and undergo keratinisation and denucleation. By the time they reach the surface they are waterproof and dead.
The dermis varies in thickness and contains the lymphatic vessels, hair follicles, sweat glands, blood vessels, nerves, etc. The dermis also hosts mast cells which release histamine and play a central role in hypersensitivity reactions, and phagocytic macrophages which have a key role in the immune response.
The subcutaneous layer consists of adipose tissue lobules separated by dense fibrous walls and blood vessels.
The rate of skin cell production must be balanced by the rate of cell loss at the surface. The control mechanism of epidermopoiesis consists of a balance of stimulatory and inhibitory signals. Wound healing is one example. A wound results in a wave of epidermal mitotic activity as a result of trigger factors, which include cytokines and growth hormones.
Managing a Child’s Skin in ITU
Early assessment of the child’s skin will avoid confusion regarding when and how the damage occurred. This is particularly important if the damage to the child’s skin becomes the subject of a complaint or clinical incident. There is some evidence to suggest that the prevention and treatment of pressure ulcers and maintenance of skin integrity in the critically ill child are not viewed as a high priority (Butler 2007). Benchmarking for one’s unit can be difficult as the prevalence of pressure ulcers in PICUs in some studies is as high as 27% (Curley et al. 2003), but has been considered to be low in other literature (McLane et al. 2004). However, the incidence of other forms of skin breakdown, such as nappy rash and IV extravasation, was higher (McLane et al. 2004). Preventing any breaches in skin integrity is preferable to managing them when they occur.
Children in the ITU are uniquely vulnerable; their dermal capillary pressure may be compromised by impaired cardiac function and peripheral shutdown. A chronically ill child may have significantly reduced dermal capillary pressure compared to a usually healthy child who is suddenly ill or admitted because of trauma. Children in ITU are at particular risk of skin damage as they are usually sedated and cannot move freely. They may have multiple and invasive lines which influence the position in which they can be nursed. They may have fitted appliances such as traction, external fixators, plasters, splits, braces, etc., and secured probes, catheters, ventilator, tubing, etc. The fit of these appliances and the means of securing lines must be frequently revised (Willock et al. 1999).
Children who destabilise when being handled may not have probes changed frequently enough for their needs. They may have impaired circulation, reducing the level of oxygen and nutrients available for the maintenance of tissues. They may be in a hypercatabolic state and not have the nutrients available to support tissue regeneration. Decubitus ulcers or pressure sores are areas of localised skin damage, which once established can extend to underlying structures such as muscle and bone (Allman et al. 1995). This may be as a result of a combination of factors, including prolonged exposure to pressure, the shearing force of friction and maceration of the skin from moisture. Pressure ulcers can develop in any area of the body (Rycroft-Malone and McInnes 2000) but generally occur over bony prominences (Jones et al. 2001; Murdoch 2002; Willock et al. 1999).
In young children nursed supine the back of the head and the ears are particularly at risk due to the size and shape of the head. Hair braids may need to be taken down to prevent hidden damage from occurring (Dixon and Ratliff 2011). The child’s sacrum and heels are also at risk. Prone infants and children may have knees, elbows, shoulders and the side of the face on the mattress more at risk, so when children are nursed prone the position of the dependent ear should be checked.
Assessment of Risk
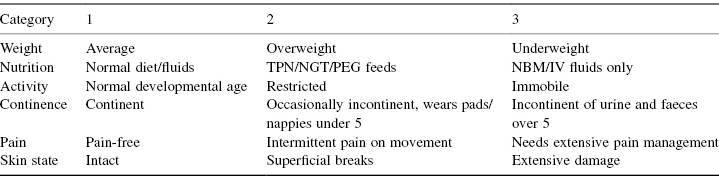
Most units use skin assessment tools and a range is available. Many children’s units use the Braden Q, although there is some evidence to suggest that the Glamorgan scale is more sensitive (Willock et al. 2009). Table 14.2 and Table 14.3 are examples of neonatal and children’s skin assessment (McGurk et al. 2004) currently in use in an area where there are minimal critical incident reports generated.
Table 14.2 Northampton neonatal skin tool
Source: reproduced by kind permission of the lead author and the Journal of Nursing Children and Young People.
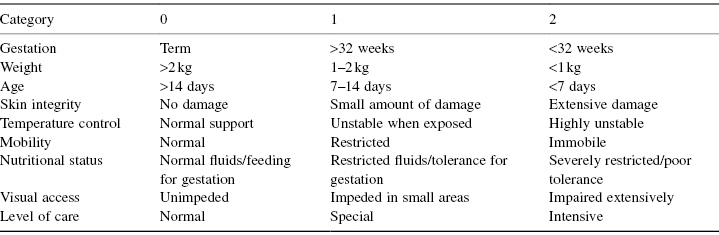
Table 14.3 Northampton Children’s Skin Tool
Source: reproduced by kind permission of the lead author and the Journal of Nursing Children and Young People.
Scores are totalled and 2 added for each of the following: intravenous cannula in situ; arterial line in situ; site of extravasation; wound; apparent birth trauma; nappy rash; electrolyte imbalance; cord clamp in situ.
Final score:
- 0–8 Low risk: Recommend daily assessment.
- 8–15 Moderate risk: Recommend 6–8 hourly assessment and repositioning.
- 16–24 High risk: Recommend 4–6 hourly assessment and repositioning.
- >24 Extreme risk: Recommend 2–4 hourly assessment and repositioning.
Add 2 for each of the following: radiotherapy, chemotherapy, steroid therapy, diabetes, >2 hours on the operating table, splints/plaster cast, anaemia (Hb <8), sensation deficit.
Final score:
- 0–4 Low risk: Daily assessment.
- 5–8 Medium risk: Twice daily assessment.
- 9+ High risk: 4–6 hourly assessment or as condition dictates.
However, a tool is only as good as the nurses who use it. A child’s skin should not be assessed in isolation but in conjunction with their clinical condition and their clinical needs and requirements taken into account. Whenever possible the child’s parent/carer should be involved in the assessment process and the comfort, privacy and dignity of the child should be a high priority. The baseline assessment of the condition of the child’s skin should be done soon after admission with the caveat that children transferred from a referring unit or having had long surgical procedures may already have suffered some pressure damage so may need immediate intervention. Children in ITU need to be assessed with every change of shift. If a child is at particular risk their skin should be assessed every time they have a change of position. Each assessment must be documented, signed and dated by the assessor.
Early signs of pressure ulcer development include erythema, particularly non-blanching erythema. There may be a discoloured area on the skin, localised heat, oedema or induration. The assessment should pay particular attention to the skin over bony prominences.
More advanced tissue damage may include an area which feels a different temperature or texture from the surrounding skin.
Planning Skin Management
Children at significant risk of pressure ulcer development should be identified and assessed at each shift change. The child’s at-risk status must be clearly documented if the child is transferred out or moved to another ward for step-down care.
The assessment should involve the child’s parents as they are often the first to notice any skin changes given their level of interaction with their child and their familiarity with the skin through dressing, changing nappies and bathing, etc. The assessment should involve the use of a tool (e.g. the Braden Q, where a score of 10 or below constitutes the child being at risk). If the child is identified as being at risk of developing a pressure ulcer a plan of care must be provided. For a child scoring 10 or lower this should include:
- An at least daily inspection of skin and bony prominences. The prophylactic use of a barrier film (e.g. Cavilon®) for children in nappies or pads, or the child could be nursed on top of the nappy/pad and discreetly covered with a light sheet.
- A plan for repositioning every 2–3 hours, using enough staff to perform the position change safely and eliminate the risk of friction and shear without overhandling the child. Devices to assist manual handling (e.g. sliding sheets, hoists) should be used where possible to reduce the potential of skin damage to the child and injury to carers. Where this is not possible because the child cannot physiologically tolerate position changes a senior member of the team should explain the reason for this to the family and document this is the child’s medical record.
- All episodes of repositioning should be recorded on the child’s chart.
- The use of a pressure-relieving mattress and support where possible. The latter includes surfaces such as mattresses or cushions and pillows to support or separate limbs. There are two main forms of pressure-relieving support surface: the continuous low-pressure surface and the alternating-pressure surface. The continuously low-pressure surface contours to the shape of the child and spreads the pressure over a larger surface area; this reduces pressure over their bony prominences. Different types are available using a variety of substances (e.g. air, gel, foam, fluid, or a combination of these). The alternating-pressure devices consist of air cells which are time-cycled. They inflate and deflate. The inflated cells support the child’s weight while the deflated cells provide pressure relief. These devices can cause some movement so are not suitable for some children; lines, catheters, etc. need to be secured. Pressure-relieving mattresses should be covered by appropriate bedding, which should be checked for creases and wrinkles when the child is moved. Pillows, foam wedges and rolls of Gamgee can be used to support and maintain position.
- Work with the multidisciplinary team to ensure that the child is adequately hydrated and their nutritional needs considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


