Managing Patient Care
Objectives
• Differentiate among the types of nursing care delivery models.
• Describe the elements of decentralized decision making.
• Discuss ways to apply clinical care coordination skills in nursing practice.
• Discuss principles to follow in the appropriate delegation of patient care activities.
Key Terms
Accountability, p. 277
Authority, p. 277
Autonomy, p. 277
Case management, p. 276
Decentralized management, p. 277
Delegation, p. 281
Empowered, p. 274
Primary nursing, p. 276
Responsibility, p. 277
Shared governance, p. 278
Team nursing, p. 276
Total patient care, p. 276
![]()
As a nursing student it is important for you to acquire the necessary knowledge and competencies that ultimately allow you to practice as an entry-level staff nurse. The National Council of State Boards of Nursing (NCSBN) identified competencies that registered nurses (RNs) and licensed practical/vocational nurses need on entry to practice (Kearney, 2009) (Box 21-1). Regardless of the type of setting in which you eventually choose to work as a staff nurse, you will be responsible for using organizational resources, participating in organizational routines while providing direct patient care, using time productively, collaborating with all members of the health care team, and using certain leadership characteristics to manage others on the nursing team. The delivery of nursing care within the health care system is a challenge because of the changes that influence health professionals, patients, and health care organizations (see Chapter 2). However, change offers opportunities. As you develop the knowledge and skills to become a staff nurse, you learn what it takes to effectively manage the patients for whom you care and to take the initiative in becoming a leader among your professional colleagues.
Building a Nursing Team
Nurses are self-directed and, with proper leadership and motivation, are able to solve most complex problems. A nurse’s education and commitment to practicing within established standards and guidelines ensures a rewarding professional career. As a nurse it is also important to work in an empowering environment as a member of a solid and strong nursing team. A strong nursing team works together to achieve the best outcomes for patients (Batcheller et al., 2004).
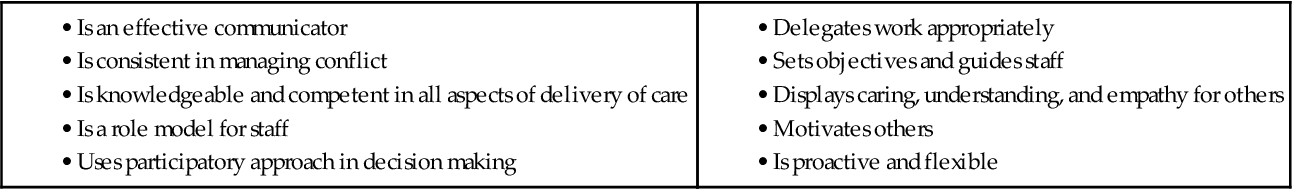
Building an empowered nursing team begins with the nurse executive, who is often vice president or director of nursing. The executive’s position within an organization is critical in uniting the strategic direction of an organization with the philosophical values and goals of nursing. The nurse executive is both a clinical and business leader who is concerned with maximizing quality of care and cost-effectiveness while maintaining relationships and professional satisfaction of the staff. The relationship between the nurse and nurse manager contributes to job satisfaction and retention (Ulrich et al., 2005). Perhaps the most important responsibility of the nurse executive is to establish a philosophy for nursing that enables managers and staff to provide quality nursing care. In this environment staff members have high levels of productivity and make contributions to the success of the organization (Feltner et al., 2008). Box 21-2 identifies the characteristics of an effective nurse leader.
It takes an excellent nurse manager and an excellent nursing staff to make an empowering work environment. Together a manager and the nursing staff have to share a philosophy of care for their work unit. A philosophy of care includes the professional nursing staff’s values and concerns for the way they view and care for patients. For example, a philosophy addresses the purpose of the nursing unit, how staff works with patients and families, and the standards of care for the work unit. Selection of a nursing care delivery model and a management structure that supports professional nursing practice are essential to the philosophy of care.
Magnet Recognition
One way of creating an empowering work environment is through the Magnet Recognition Program (see Chapter 2). A Magnet hospital has a transformed culture with a practice environment that is dynamic, autonomous, collaborative, and positive for nurses. The culture focuses on concern for patients. Typically a Magnet hospital has clinical promotion systems and research and evidence-based practice programs. The nurses have professional autonomy over their practice and control over the practice environment (Upenieks and Sitterding, 2008). A Magnet hospital empowers the nursing team to make changes and be innovative. Professional nurse councils at the organizational and unit level are one way to create an empowerment model. An effective empowerment model leads to a staff that feels valued and has increased autonomy and a work environment that promotes job satisfaction (Gokenbach, 2007).This culture and empowerment combine to produce a strong collaborative relationship among team members and improve patient quality outcomes (Box 21-3).
Nursing Care Delivery Models
Since the time of Florence Nightingale nurses have used a variety of nursing care delivery models to provide care for patients. Ideally the philosophy that nurses establish for the quality care of patients guides the selection of a care delivery model. However, too often a lack of nursing resources and business plans from the health care organization influences the final decision. A care delivery model needs to help nurses achieve desirable outcomes for their patients, either in the way work is organized or in the way a nurse’s responsibilities are defined. Important factors contributing to success of a care delivery model are decision-making authority for nurses who provide direct care, autonomy, collaborative practice, and effective methods of communicating with colleagues, physicians, and other health care providers (Tiedeman and Lookinland, 2004). In effective nursing models, the experienced RN provides faster diagnosis and intervention, which promotes a safe patient environment (Berkow et al., 2007).
Three common models are team nursing, total patient care, and primary nursing. Team nursing developed in response to the severe nursing shortage following World War II. By 2000 the interdisciplinary team was a more common model (Marriner Tomey, 2009). Total patient care delivery was the original care delivery model developed during Florence Nightingale’s time. The model disappeared in the 1930s and became popular again during the 1970s and 1980s, when the number of RNs increased (Tiedeman and Lookinland, 2004). The primary nursing model of care delivery was developed to place RNs at the bedside and improve the accountability of nursing for patient outcomes and the professional relationships among staff members (Marriner Tomey, 2009). The model became more popular in the 1970s and early 1980s as hospitals began to employ more RNs. Primary nursing supports a philosophy regarding nurse and patient relationships. Table 21-1 summarizes the three nursing models.
TABLE 21-1
| NURSING MODEL | CHARACTERISTICS | ADVANTAGES | DISADVANTAGES |
| Team nursing | |||
| Total patient care | |||
| Primary nursing |
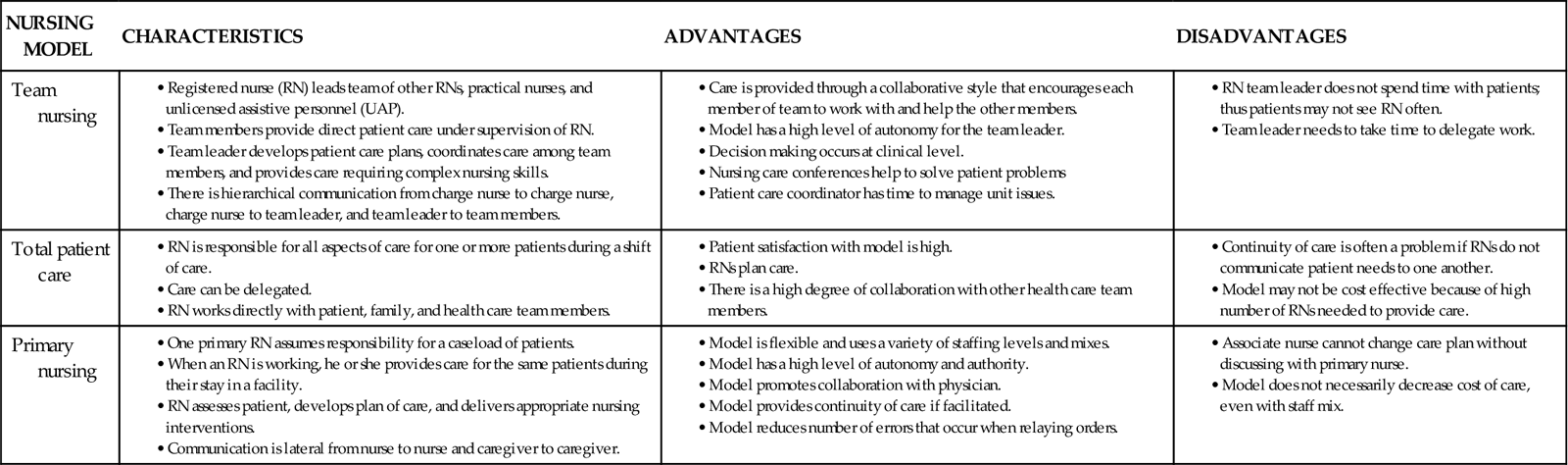
Modified from Marriner Tomey A: Guide to nursing management and leadership, ed 8, St Louis, 2009, Mosby; Tiedeman ME, Lookinland S: Traditional models of care delivery: what have we learned? J Nurs Adm 34(6):291, 2004.
Case management is a care management approach that coordinates and links health care services to patients and their families while streamlining costs and maintaining quality (Marriner Tomey, 2009) (see Chapter 2). The Case Management Society of America (2010) defines case management as “a collaborative process of assessment, planning, facilitation, and advocacy for options and services to meet an individual’s health needs through communication and available resources to promote quality cost-effective outcomes.” Case management is unique because clinicians, either as individuals or as part of a collaborative group, oversee the management of patients with specific, complex health problems or are held accountable for some standard of cost management and quality.
For example, a case manager coordinates a patient’s acute care in the hospital and follows up with the patient after discharge home. Case managers do not always provide direct care but instead work with and supervise the care delivered by other staff and health care team members and actively coordinate patient discharge planning. Ongoing communication with team members facilitates the patient’s transition to home (Carr, 2007). In this situation the case manager helps the patient identify health needs, determine the services and resources that are available, and make cost-efficient choices (Marriner Tomey, 2009). The case manager frequently oversees a caseload of patients with complex nursing and medical problems. Often he or she is an advanced practice nurse who, through specific interventions, helps to improve patient outcomes, optimize patient safety by facilitating care transitions, decrease length of stay, and lower health care costs (Carr, 2007; Thomas, 2008).
Many organizations use critical pathways or CareMaps in a case management delivery system (see Chapter 18). These are multidisciplinary treatment plans for specific cases. The case manager, along with members of the health care team, uses the critical pathways or CareMaps to implement timely interventions in a coordinated plan of care. The plans eliminate the guesswork in patient care because all members of the health care team work from the same plan.
Decision Making
With a philosophy for nursing established, it is the manager who directs and supports staff in the realization of that philosophy. The nurse executive supports managers by establishing a structure that helps to achieve organizational goals and provide appropriate support to care delivery staff. It takes a committed nurse executive, an excellent manager, and an empowered nursing staff to create an enriching work environment in which nursing practice thrives.
Decentralized management, in which decision making is moved down to the level of staff, is very common within health care organizations. This type of management structure has the advantage of creating an environment in which managers and staff become more actively involved in shaping the identity and determining the success of a health care organization. Working in a decentralized structure has the potential for greater collaborative effort, increased competency of staff, increased staff motivation, and ultimately a greater sense of professional accomplishment and satisfaction.
Progressive organizations achieve more when employees at all levels are actively involved. As a result, the role of a nurse manager is critical in the management of effective nursing units or groups. Box 21-4 highlights the diverse responsibilities of nursing managers. To make decentralized decision making work, managers need to know how to move it down to the lowest level possible. On a nursing unit it is important for all nursing staff members (RNs, licensed practical nurses [LPNs], and licensed vocational nurses [LVNs]), nurse assistants, and unit secretaries to become involved. They need to be kept well informed. They also need to be given the opportunity by managers to participate in problem-solving activities, including opportunities in direct patient care and unit activities such as committee participation. Important elements of the decision-making process are responsibility, autonomy, authority, and accountability (Anders and Hawkins, 2006).
Responsibility refers to the duties and activities that an individual is employed to perform. A position description outlines a professional nurse’s responsibilities. Nurses meet these responsibilities through participation as members of the nursing unit.
Responsibility reflects ownership. The individual who manages the employee has to distribute responsibility, and the employee has to accept it. Managers have to be sure that staff clearly understand their responsibilities, particularly in the face of change. For example, when hospitals participate in work redesign, patient care delivery models change significantly. A manager is responsible for clearly defining the RN’s role within the new care delivery model. If decentralized decision making is in place, professional staff have a voice in identifying the new RN role. Each RN on the work team is responsible for knowing his or her role and how to perform that role on the busy nursing unit. For example, primary nurses are responsible for completing a nursing assessment of all assigned patients and developing a plan of care that addresses each of the patient’s nursing diagnoses (see Chapters 15 to 20). As the staff delivers the plan of care, the primary nurse evaluates whether the plan is successful. This responsibility becomes a work ethic for the nurse in delivering excellent patient care.
Autonomy is freedom of choice and responsibility for the choices (Marriner Tomey, 2009). Autonomy consistent with the scope of professional nursing practice maximizes your effectiveness as a nurse (Weston, 2008). With clinical autonomy a professional nurse makes independent decisions about patient care, planning nursing care for the patient within the scope of professional nursing practice. The nurse implements independent nursing interventions (Weston, 2008) (see Chapter 18). Another type of autonomy for nurses is work autonomy. In work autonomy the nurse makes independent decisions about the work of the unit such as scheduling or unit governance (Weston, 2008). Autonomy is not an absolute; it occurs in degrees. For example, a nurse has the autonomy to develop and implement a discharge teaching plan based on specific patient needs for any hospitalized patient. He or she also provides nursing care that complements the prescribed medical therapy.
Authority refers to legitimate power to give commands and make final decisions specific to a given position (Anders and Hawkins, 2006; Marriner Tomey, 2009). For example, a primary nurse managing a caseload of patients discovers that members of the nursing team did not follow through on a discharge teaching plan for an assigned patient. The primary nurse has the authority to consult other nurses to learn why the team did not follow recommendations on the plan of care and to choose appropriate teaching strategies for the patient that all members of the team will follow. The primary nurse has the final authority in selecting the best course of action for the patient’s care.
Accountability refers to individuals being answerable for their actions. It means that as a nurse you accept the commitment to provide excellent patient care and the responsibility for the outcomes of the actions in providing that care (Anders and Hawkins, 2006). A primary nurse is accountable for his or her patients’ outcomes and for ensuring that each patient learns the information necessary to improve self-care. The nurse demonstrates accountability by checking on the patient and family after discharge and reviewing with the nursing team whether continuity in teaching occurred.
A successful decentralized nursing unit supports the four elements of decision making: responsibility, autonomy, authority, and accountability. An effective manager sets the same expectations for the staff in how decisions are made. Staff routinely meet to discuss and negotiate how to maintain an equality and balance in the elements. Staff members need to feel comfortable in expressing differences of opinion and challenging ways in which the team functions while recognizing their own responsibility, autonomy, authority, and accountability. Ultimately decentralized decision making helps create the philosophy of professional nursing care for the unit.
Staff Involvement
When decentralized decision making exists on a nursing unit, all staff members actively participate in unit activities (Fig. 21-1). The influence and control that nurses have over their practice contribute to job satisfaction (Schmalenberg and Kramer, 2008). Because the work environment promotes participation, all staff members benefit from the knowledge and skills of the entire work group. If the staff learns to value knowledge and the contributions of co-workers, better patient care is an outcome. Experienced RNs provide leadership and mentoring on a nursing unit while promoting collaborative practice (Berkow et al., 2007). The nursing manager supports staff involvement through a variety of approaches:
1 Establishing nursing practice or problem-solving committees or professional shared governance councils. Chaired by senior clinical staff, these groups establish and maintain care standards for nursing practice on their work unit. Shared governance councils promote empowerment in staff nurses and enable them to control their nursing practice (Kramer et al., 2008, 2010). The committees review and establish standards of care, develop policy and procedures, resolve patient satisfaction issues, or develop new documentation tools. It is important for the committees to focus on patient outcomes rather than only work issues to ensure quality care on the unit. Quality of care is further improved when nurses control their own practice (Anders and Hawkins, 2006). The committee establishes methods to ensure that all staff have input or participation on practice issues. Managers do not always sit on a committee, but they receive regular reports of committee progress. The nature of work on the nursing unit determines committee membership. At times members of other disciplines (e.g., pharmacy, respiratory therapy, or clinical nutrition) participate in practice committees or shared governance councils.
2 Nurse/physician collaborative practice. Collaboration is a process between individuals. There is a sharing of different perspectives that are then synthesized to better understand complex problems. An outcome of collaboration is a shared solution that could not have been accomplished by a single person or organization. Nurse-physician collaboration improves patient safety and outcomes and reduces errors (Manojlovich et al., 2008; Seago, 2008). The care delivery model of the nursing unit, an environment that supports teamwork, and organizational values influence how nurses and physicians collaborate. An open communication system that fosters respect, trust, shared decision making, and teamwork among all team members is critical to achieving quality patient care (Cronenwett et al., 2007). Physicians sometimes attend practice committees when clinical problems arise and present timely in-service programs.
3 Interdisciplinary collaboration. The emphasis on efficiency in health care delivery brings all members of the health care team together. Teamwork decreases mistakes because team members commit to shared knowledge, skills, and attitudes (Baker et al., 2006). Interdisciplinary collaboration leads to decreased patient mortality, decreased health care costs, and increased nurse job satisfaction (Manojlovich et al., 2008). Mutual respect is a critical part of any collaborative relationship (Ulrich et al., 2005). Essential characteristics for effective teams include having a common purpose, communicating frequently, anticipating one another, trust, managing conflict well, and providing feedback to one another (Baker et al., 2006). Use your judgment to decide which problems are complex and require a collaborative process. At the patient care level, staff recognize the importance of prompt referrals and timely communication with other health professionals. Participating in interdisciplinary patient care rounds, use of protocols and critical pathways, and holding interdisciplinary training for collaboration development are strategies that promote interdisciplinary collaboration (Kramer et al., 2010). Other strategies include having representatives of the various disciplines together in practice projects, in-service programs, conferences, and staff meetings.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree