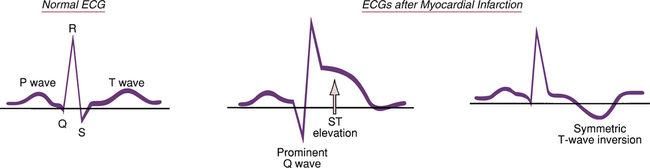
CHAPTER 53 Acute STEMI produces changes in the ECG. Why? Because conduction of electrical impulses through the heart becomes altered in the region of injury. Elevation of the ST segment, which defines STEMI, occurs almost immediately in response to acute ischemia (Fig. 53–1). Following a period of ST-segment elevation, a prominent Q wave (more than 40 milliseconds in duration) develops in the majority of patients. (Q waves are small or absent in the normal ECG.) Over time, the ST segment returns to baseline, after which a symmetric inverted T wave appears. This T-wave inversion may resolve within weeks to months. Q waves may resolve over a period of years. • ACC/AHA Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction) • 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines • 2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines • 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction (Updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (Updating the 2005 Guideline and 2007 Focused Update): A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines These guidelines are available online at circ.ahajournals.org. The discussion below reflects recommendations in these documents. Beta blockers should be used routinely in the absence of specific contraindications (eg, asthma, bradycardia, significant LV dysfunction). The initial dose may be oral or IV; oral dosing is used thereafter. Treatment with an oral beta blocker should begin within 24 hours and should continue for at least 2 to 3 years, and perhaps longer. Beta blockers are especially good for patients with reflex tachycardia, systolic hypertension, atrial fibrillation, and atrioventricular conduction abnormalities. Contraindications include overt severe heart failure, pronounced bradycardia, persistent hypotension, advanced heart block, and cardiogenic shock. The basic pharmacology of the beta blockers is presented in Chapter 18.
Management of ST-elevation myocardial infarction
Diagnosis of STEMI
ECG changes.
Management of STEMI
Routine drug therapy
Beta blockers
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Management of ST-elevation myocardial infarction
Only gold members can continue reading. Log In or Register to continue
Get Clinical Tree app for offline access