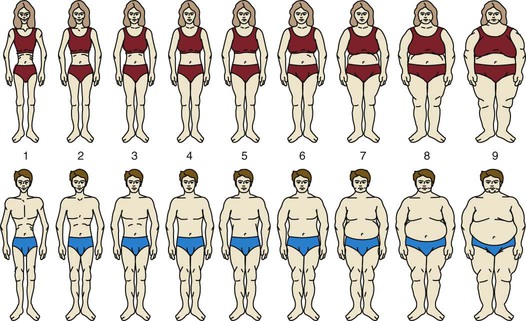
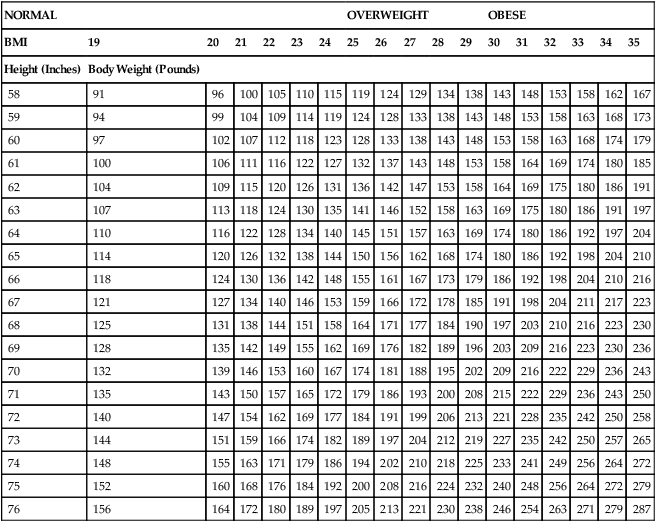
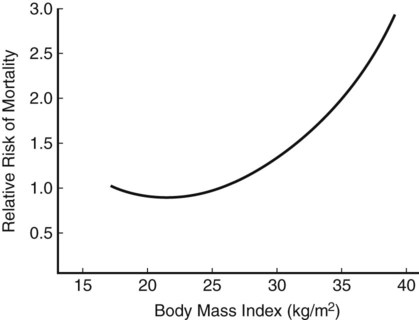
As America entered the twentieth century, things changed. There developed a preference for slenderness that has not abated. Why this change in perception of attractiveness occurred and endured is not completely clear. Probably it was the coming together of several factors. These include concerns about the effects of an increasingly sedentary lifestyle, a heightened interest in fashion, the development of the medical profession, and increased knowledge of nutrition, as well as the self-interests of various promoters who saw profit to be gained by creating an anxiety about fatness.1 Most of us weigh ourselves regularly and have a good idea of our current weight. The figure on the scale, however, does not always agree with how fat we feel. Figure 10-1 shows an example of the type of instrument that investigators use to assess differences between actual, perceived, and preferred body size. The investigator instructs the subjects to mark the figure that is most like the way they feel at that time, as well as the figure that they consider ideal for themselves. When these figures are compared with an objective assessment, regardless of their actual size, the subjects usually have greatly overestimated their size. Investigators also use figure rating scales to determine how men and women differ in size preferences; they ask you which figure is most like how you would like to be, which is most like how you currently are, and which you think is most attractive to the opposite sex. Ideally, the answers to these three questions would be closely clustered, indicating that you are fairly satisfied with your size. For men, that is usually the case. Women, however, on average consider themselves much fatter than they think is ideal. Originally it was assumed that the women’s dissatisfaction represented a desire to appear more slender and, therefore, more attractive to men. Usually, however, women’s personal ideal is thinner than the figure they think men would choose, challenging the assumption that women want to be thin to attract men. An alternative interpretation is that both men and women interpret a slender body as evidence of being in control of one’s life.2 Why is body image important? A negative body image may affect how we feel about ourselves generally: body image tends to become self-image. Furthermore, a negative body image may influence our health behaviors. We may feel defeated that because our bodies are so bad, it is not worth working hard to improve our health. At other times we may feel drawn to various kinds of risky behaviors in a frantic attempt to make our bodies more acceptable. We may strive mightily to meet the societal standards of attractiveness and thinness, but, given our individual genetic makeup, we cannot all succeed. Although humans have an awesome potential for growth and development, there are limits to the changes we can make and sustain in our body size and shape.2 If we have a healthy and positive body image, we evaluate various aspects of our bodies fairly realistically, finding some characteristics positive and others less so. Those we consider weak or unattractive, we accept in a dispassionate way, much the same way that we accept that we don’t all have beautiful singing voices or the ability to throw a great curveball. We understand that our bodies have multiple aspects, that there is more to our bodies than their size and shape. Our healthy body image is influenced by our awareness of how our bodies function and how they look. This image affects and is affected by socio-demographic factors. Body image satisfaction may be related to the degree of overweight and to psychologic distress represented by depression and low self-esteem.3 Understanding and accepting what we can and cannot expect to achieve in pursuit of the ideal body is a key to wellness. Only with this understanding can we establish goals to guide our behaviors toward health (see the Social Issues box, Dealing With Our Own Prejudices). Most of our evidence of the association between fatness and physical health comes from epidemiologic studies. Epidemiologic research investigates the distribution of disease in a population and seeks to explain associations between causative factors and the disease. This type of research usually involves thousands of subjects and may be longitudinal (i.e., involving observations over a number of years). Because it is not practical to measure fatness in these large studies, weight is usually measured instead. Weight is most meaningful when considered in relationship to height. A convenient way to determine fatness is to calculate body mass index (BMI), a value derived by dividing one’s weight in kilograms by the square of one’s height in meters (Table 10-1). This formula for BMI results in a value that correlates well with body fatness. TABLE 10-1 Data from Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. From National Institutes of Health: Aim for a healthy weight, NIH Pub. No. 05-5213, Bethesda, Md, 2005 (August), U.S. Department of Health and Human Services. If we were to plot the findings of epidemiologic studies of the association of BMI and the risk of certain diseases or mortality from all causes, we would usually produce a U-shaped curve such as that shown in Figure 10-2.4 This curve means that individuals at both extremes of fatness—those very thin and those very fat—are at increased risk. Those at a more moderate fatness level have the lowest risk for the four leading causes of death in the United States: heart disease, some types of cancer, stroke, and diabetes. It is a surprise to many people that the low end of the fatness range, or underweight, shows an increased risk, which provides strong evidence that one can be too thin. It is possible that the lowest BMI in these types of curves reflects low levels not of fat but of the lean body components.4 The higher risks at the low BMI levels probably reflect some degree of body wasting, including lean body mass, possibly caused by smoking or the effects of disease. To understand the effect of fat on mortality, we need to measure body composition (fat and lean) and not rely on weight alone. Although the factors contributing to this increased risk of extremely low weight are not completely clear, they are thought to differ from the factors associated with increased risk of heavy individuals. As research has extended beyond merely relating BMI to mortality risk, we have become aware that, between extreme emaciation and great obesity, just knowing how fat a person is doesn’t tell us much about their health. If we consider how the body fat is distributed, we can improve our understanding. Without knowing the individual’s total fatness or BMI, we can still make fat-mediated predictions about health risk. Higher levels of body fat around the waist seem to be more dangerous than fat in the buttocks and thighs. Fat located in the abdominal area is called visceral fat and seems to be especially related to risk. People with high levels of visceral fat are prone to a cluster of metabolic risk factors, including high blood pressure (hypertension of ≥130/85 mm Hg); low level high-density lipoproteins (men <40 mg/dL; women <50 mg/dL); elevated triglycerides (≥150 mg/dL); and impaired fasting glucose.5 When three or more of these criteria are present, the condition is referred to as the metabolic syndrome.5 TABLE 10-2 POTENTIAL HEALTH CONCERNS ASSOCIATED WITH OR AT GREATER RISK FOR OBESE INDIVIDUALS Adapted from Table 1.3, p. 35, Power ML, Schulkin J: The evolution of obesity, Baltimore, MD, 2009, The Johns Hopkins University Press. Does losing weight make health risks go away? And what about weight gain? We don’t have strong evidence that weight loss reduces health risk. The literature is mixed about the long-term health effects of weight loss; some epidemiologic studies show increased risks following weight loss, whereas others show no effect or a diminished risk.6 Important factors seem to be whether the weight was lost in response to a voluntary effort, the health condition of the person initially, and the pattern of weight changes (many gains and losses, one sustained loss, or other patterns). One issue of contemporary concern is the effect of repeated or chronic dieting on risk. Given our cultural concern about fatness and the extremely limited success of most weight-loss attempts, there is a high likelihood that an overweight or obese adult will have tried to lose weight many times. Is it possible that some of the observed negative effects of obesity are really the outcomes of a lifetime of unsuccessful dieting? Although animal studies and some limited observations of humans support this hypothesis, reviews of the evidence conclude the risks were not strong enough to justify discouraging people from making repeated attempts to lose weight6 (see the Personal Perspectives box, A Work in Progress). For many years investigators have searched for a psychopathology that would fit most obese people and would help explain their fatness. Their efforts failed, for although a minority of overweight people suffer from a variety of mental health problems, no set of psychologic problems typical of obesity has been identified.8 Our culture’s extreme stigma against fatness extracts a tremendous toll on people who are obese. Social, economic, and other types of discrimination against obese people are widely practiced. This may lead to impaired self-image and feelings of inferiority, which in turn may contribute to social isolation and depression. Some people feel so guilty about their fatness that they hide away and put their lives on hold until they can achieve slenderness.
Management of Body Composition
Body Composition, Body Image, and Culture
Body Image
Body Perception
Body Image: Illusions versus Reality
Body Preferences: Gender Concerns
Body Acceptance: A Key to Wellness
Management of Body Fat Composition
Association of Body Fatness with Health
Physical Health
NORMAL
OVERWEIGHT
OBESE
BMI
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
Height (Inches)
Body Weight (Pounds)
58
91
96
100
105
110
115
119
124
129
134
138
143
148
153
158
162
167
59
94
99
104
109
114
119
124
128
133
138
143
148
153
158
163
168
173
60
97
102
107
112
118
123
128
133
138
143
148
153
158
163
168
174
179
61
100
106
111
116
122
127
132
137
143
148
153
158
164
169
174
180
185
62
104
109
115
120
126
131
136
142
147
153
158
164
169
175
180
186
191
63
107
113
118
124
130
135
141
146
152
158
163
169
175
180
186
191
197
64
110
116
122
128
134
140
145
151
157
163
169
174
180
186
192
197
204
65
114
120
126
132
138
144
150
156
162
168
174
180
186
192
198
204
210
66
118
124
130
136
142
148
155
161
167
173
179
186
192
198
204
210
216
67
121
127
134
140
146
153
159
166
172
178
185
191
198
204
211
217
223
68
125
131
138
144
151
158
164
171
177
184
190
197
203
210
216
223
230
69
128
135
142
149
155
162
169
176
182
189
196
203
209
216
223
230
236
70
132
139
146
153
160
167
174
181
188
195
202
209
216
222
229
236
243
71
135
143
150
157
165
172
179
186
193
200
208
215
222
229
236
243
250
72
140
147
154
162
169
177
184
191
199
206
213
221
228
235
242
250
258
73
144
151
159
166
174
182
189
197
204
212
219
227
235
242
250
257
265
74
148
155
163
171
179
186
194
202
210
218
225
233
241
249
256
264
272
75
152
160
168
176
184
192
200
208
216
224
232
240
248
256
264
272
279
76
156
164
172
180
189
197
205
213
221
230
238
246
254
263
271
279
287
Obesity and Physical Health
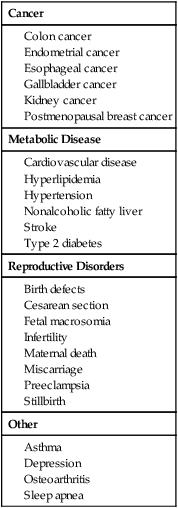
![]() Obesity also increases the risk of health conditions that affect well-being but aren’t usually life threatening. Examples include menstrual irregularities, infertility, gallbladder disease, and some types of arthritis. Table 10-2 lists health issues for which obesity increases risk.
Obesity also increases the risk of health conditions that affect well-being but aren’t usually life threatening. Examples include menstrual irregularities, infertility, gallbladder disease, and some types of arthritis. Table 10-2 lists health issues for which obesity increases risk.
Cancer
Metabolic Disease
Reproductive Disorders
Other
![]() Unanswered questions.
Unanswered questions.
![]() Most epidemiologic studies include only initial weight, final weight, and mortality. This level of evidence is inadequate to illustrate the effect of sustained weight changes. One of the studies attempting to provide the needed information is the Nurses’ Health Study, which has monitored for 20 years the health of more than 100,000 female nurses. This study shows that nurses who gained 22 pounds or more after the age of 18 had increased mortality risk in middle age.7
Most epidemiologic studies include only initial weight, final weight, and mortality. This level of evidence is inadequate to illustrate the effect of sustained weight changes. One of the studies attempting to provide the needed information is the Nurses’ Health Study, which has monitored for 20 years the health of more than 100,000 female nurses. This study shows that nurses who gained 22 pounds or more after the age of 18 had increased mortality risk in middle age.7
Chronic dieting and risk.
Obesity and Emotional/Social Health
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Management of Body Composition
Get Clinical Tree app for offline access