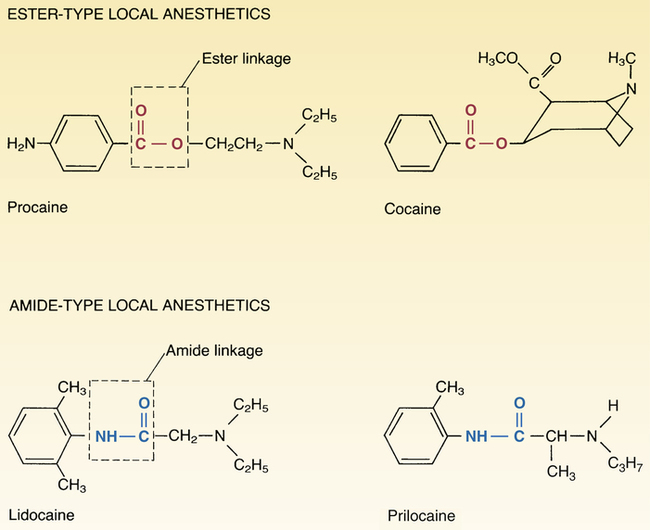
CHAPTER 26 There are two major groups of local anesthetics: esters and amides. As shown in Figure 26–1, the ester-type anesthetics, represented by procaine [Novocain], contain an ester linkage in their structure. In contrast, the amide-type agents, represented by lidocaine [Xylocaine], contain an amide linkage. The ester-type agents and amide-type agents differ in two important ways: (1) method of inactivation and (2) promotion of allergic responses. Contrasts between the esters and amides are summarized in Table 26–1. TABLE 26–1 Contrasts Between Ester and Amide Local Anesthetics Ideally, local anesthesia would begin promptly and would persist no longer (or shorter) than needed. Unfortunately, although onset of anesthesia is usually rapid (see Tables 26–2 and 26–3 below), duration of anesthesia is often less than ideal. In some cases, anesthesia persists longer than needed. In others, repeated administration is required to maintain anesthesia of sufficient duration. When absorbed in sufficient amounts, local anesthetics can affect the heart and blood vessels. In the heart, these drugs suppress excitability in the myocardium and conducting system, and thereby can cause bradycardia, heart block, reduced contractile force, and even cardiac arrest. In blood vessels, anesthetics relax vascular smooth muscle; the resultant vasodilation can cause hypotension. As discussed in Chapter 49 (Antidysrhythmic Drugs), the cardiosuppressant actions of one local anesthetic—lidocaine—are exploited to treat dysrhythmias. In addition to its use in local anesthesia, lidocaine is employed to treat dysrhythmias (see Chapter 49). Control of dysrhythmias results from suppression of cardiac excitability secondary to blockade of cardiac sodium channels.
Local anesthetics
Basic pharmacology of the local anesthetics
Classification

Property
Ester-type Anesthetics
Amide-type Anesthetics
Characteristic Chemistry
Ester bond
Amide bond
Representative Agent
Procaine
Lidocaine
Incidence of Allergic Reactions
Low
Very low
Method of Metabolism
Plasma esterases
Hepatic enzymes
Time course of local anesthesia
Adverse effects
Cardiovascular system.
Properties of individual local anesthetics
Procaine
Lidocaine

Local anesthetics
Get Clinical Tree app for offline access