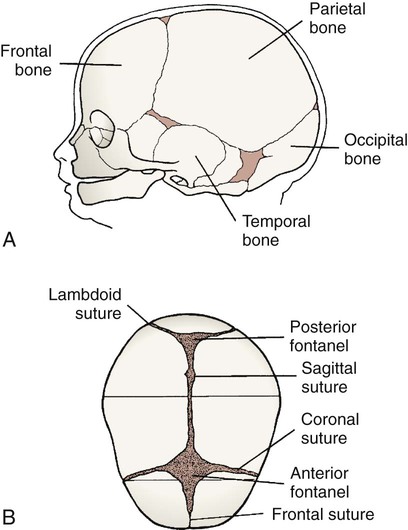
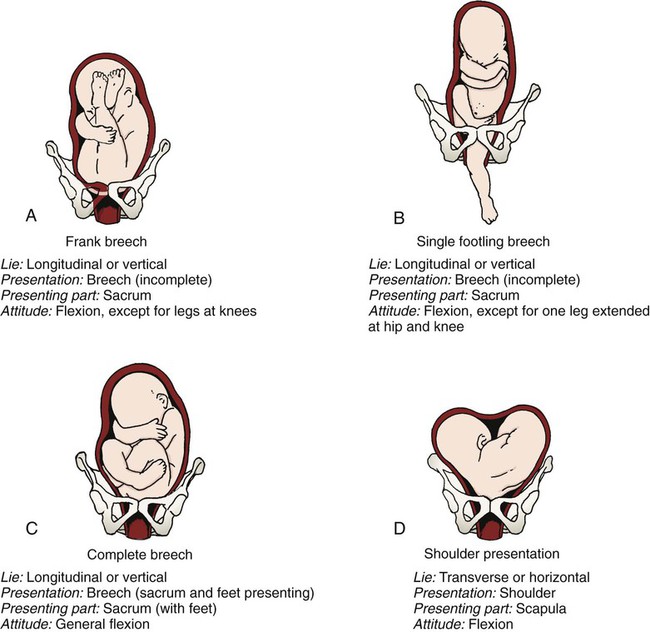
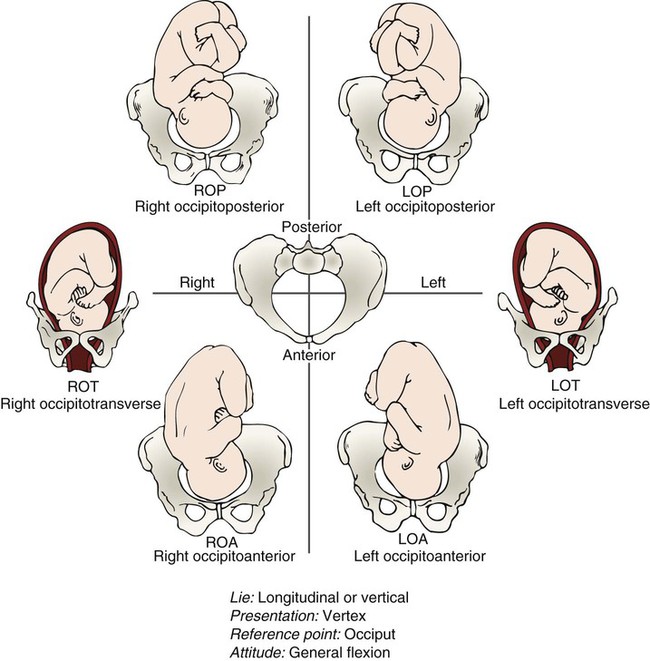
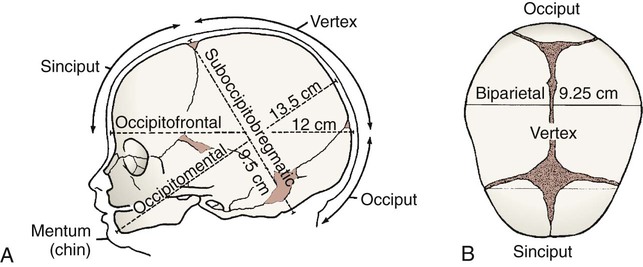
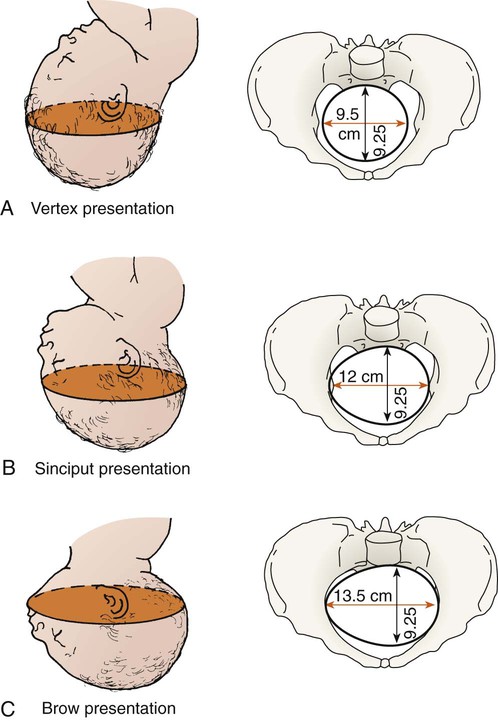
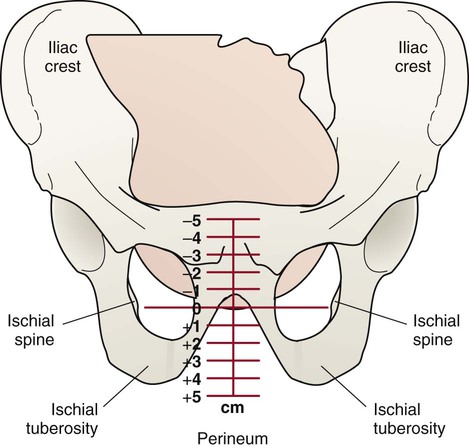
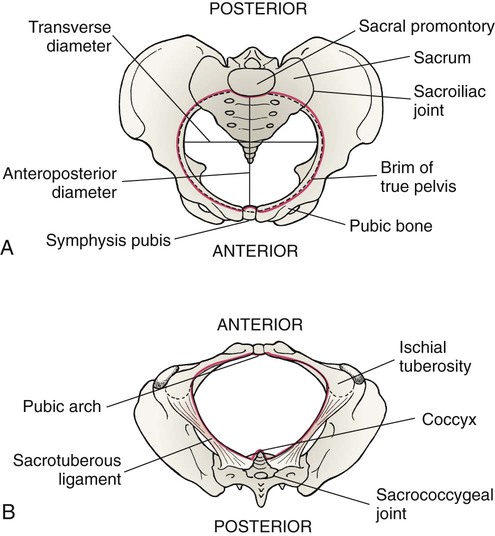
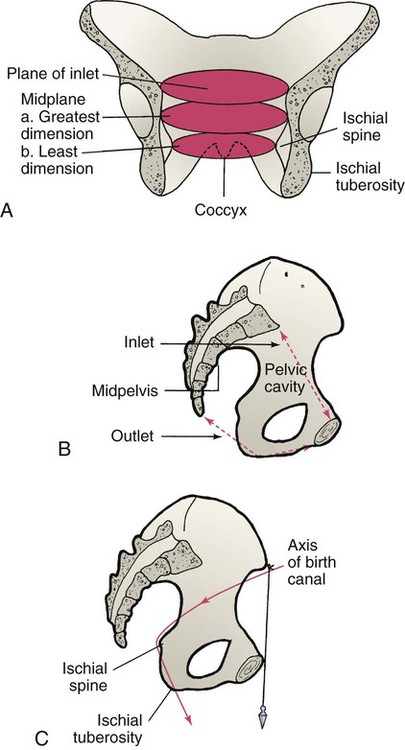
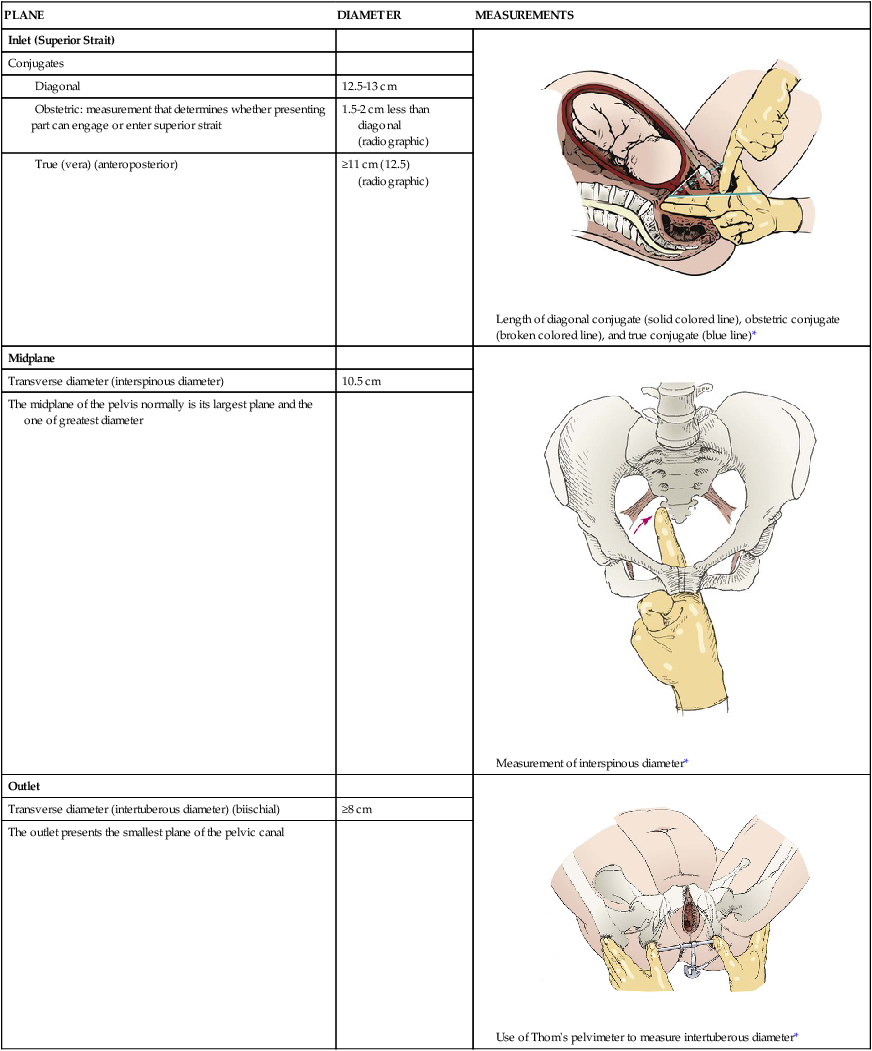
On completion of this chapter, the reader will be able to: • Explain the five major factors that affect the labor process. • Describe the anatomic structure of the bony pelvis. • Recognize the normal measurements of the diameters of the pelvic inlet, cavity, and outlet. • Explain the significance of the size and position of the fetal head during labor and birth. • Summarize the cardinal movements of the mechanism of labor for a vertex presentation. • Examine the maternal anatomic and physiologic adaptations to labor. • Describe factors thought to contribute to the onset of labor. At least five factors affect the process of labor and birth. These are easily remembered as the five Ps: passenger (fetus and placenta), passageway (birth canal), powers (contractions), position of the mother, and psychologic response. The first four factors are presented here as the basis of understanding the physiologic process of labor. The fifth factor is discussed in Chapter 16. Other factors that may be a part of the woman’s labor experience may be important as well. VandeVusse (1999) identified external forces, including place of birth, preparation, type of provider (especially nurses), and procedures. Physiology (sensations) was identified as an internal force. These factors are discussed generally in Chapter 16 as they relate to nursing care during labor. Further research investigating essential forces of labor is recommended. The movement of the passenger, or fetus, through the birth canal is determined by several interacting factors: the size of the fetal head, fetal presentation, fetal lie, fetal attitude, and fetal position. Because the placenta also must pass through the birth canal, it can be considered a passenger along with the fetus; however, the placenta rarely impedes the process of labor in normal vaginal birth. An exception is the case of placenta previa (see Chapter 12). Because of its size and relative rigidity, the fetal head has a major effect on the birth process. The fetal skull is composed of two parietal bones, two temporal bones, the frontal bone, and the occipital bone (Fig. 13-1, A). These bones are united by membranous sutures: the sagittal, lambdoidal, coronal, and frontal (see Fig. 13-1, B). Membrane-filled spaces called fontanels are located where the sutures intersect. During labor after rupture of membranes, palpation of fontanels and sutures during vaginal examination reveals fetal presentation, position, and attitude. The two most important fontanels are the anterior and posterior (see Fig. 13-1, B). The larger of these, the anterior fontanel, is diamond shaped, about 3 cm by 2 cm, and lies at the junction of the sagittal, coronal, and frontal sutures. It closes by 18 months after birth. The posterior fontanel lies at the junction of the sutures of the two parietal bones and the occipital bone, is triangular, and is about 1 cm by 2 cm. It closes 6 to 8 weeks after birth. Presentation refers to the part of the fetus that enters the pelvic inlet first and leads through the birth canal during labor at term. The three main presentations are cephalic presentation (head first), occurring in 96% of births (Fig. 13-2); breech presentation (buttocks, feet, or both first), occurring in 3% of births (Fig. 13-3, A-C); and shoulder presentation, seen in 1% of births (see Fig. 13-3, D). The presenting part is that part of the fetus that lies closest to the internal os of the cervix. It is the part of the fetal body first felt by the examining finger during a vaginal examination. In a cephalic presentation the presenting part is usually the occiput; in a breech presentation it is the sacrum; in the shoulder presentation it is the scapula. When the presenting part is the occiput, the presentation is noted as vertex (see Fig. 13-2). Factors that determine the presenting part include fetal lie, fetal attitude, and extension or flexion of the fetal head. Lie is the relation of the long axis (spine) of the fetus to the long axis (spine) of the mother. The two primary lies are longitudinal, or vertical, in which the long axis of the fetus is parallel with the long axis of the mother (see Fig. 13-2); and transverse, horizontal, or oblique, in which the long axis of the fetus is at a right angle diagonal to the long axis of the mother (see Fig. 13-3, D). Longitudinal lies are either cephalic or breech presentations, depending on the fetal structure that first enters the mother’s pelvis. Vaginal birth cannot occur when the fetus stays in a transverse lie. An oblique lie (i.e., one in which the long axis of the fetus is lying at an angle to the long axis of the mother) is less common and usually converts to a longitudinal or transverse lie during labor (Cunningham, Leveno, Bloom, et al., 2010). Attitude is the relation of the fetal body parts to one another. The fetus assumes a characteristic posture (attitude) in utero partly because of the mode of fetal growth and partly because of the way the fetus conforms to the shape of the uterine cavity. Normally the back of the fetus is rounded so the chin is flexed on the chest, the thighs are flexed on the abdomen, and the legs are flexed at the knees. The arms are crossed over the thorax, and the umbilical cord lies between the arms and the legs. This attitude is termed general flexion (see Fig. 13-2). Certain critical diameters of the fetal head are usually measured. The biparietal diameter, which is about 9.25 cm at term, is the largest transverse diameter and an important indicator of fetal head size (Fig. 13-4, B). In a well-flexed cephalic presentation the biparietal diameter is the widest part of the head entering the pelvic inlet. Of the several anteroposterior diameters, the smallest and most critical one is the suboccipitobregmatic diameter (about 9.5 cm at term). When the fetal head is in complete flexion, this diameter allows it to pass through the true pelvis easily (see Fig. 13-4, A; Fig. 13-5, A). As the head is more extended, the anteroposterior diameter widens, and the head may not be able to enter the true pelvis (see Fig. 13-5, B and C). The presentation or presenting part indicates the portion of the fetus that overlies the pelvic inlet. Position is the relationship of a reference point on the presenting part (occiput, sacrum, mentum [chin] or sinciput [deflexed vertex]) to the four quadrants of the mother’s pelvis (see Fig. 13-2). Position is denoted by a three-letter abbreviation. The first letter of the abbreviation denotes the location of the presenting part in the right (R) or left (L) side of the mother’s pelvis. The middle letter stands for the specific presenting part of the fetus (O for occiput, S for sacrum, M for mentum [chin], and Sc for scapula [shoulder]). The third letter stands for the location of the presenting part in relation to the anterior (A), posterior (P), or transverse (T) portion of the maternal pelvis. For example, ROA means that the occiput is the presenting part and is located in the right anterior quadrant of the maternal pelvis (see Fig. 13-2). LSP means that the sacrum is the presenting part and is located in the left posterior quadrant of the maternal pelvis (see Fig. 13-3). Station is the relationship of the presenting fetal part to an imaginary line drawn between the maternal ischial spines and is a measure of the degree of descent of the presenting part of the fetus through the birth canal. The placement of the presenting part is measured in centimeters above or below the ischial spines (Fig. 13-6). For example, when the lowermost portion of the presenting part is 1 cm above the spines, it is noted as being minus (−)1. At the level of the spines the station is referred to as 0 (zero). When the presenting part is 1 cm below the spines, the station is said to be plus (+)1. Birth is imminent when the presenting part is at +4 to +5 cm. The station of the presenting part should be determined when labor begins so the rate of descent of the fetus during labor can be determined accurately. The passageway, or birth canal, is composed of the mother’s rigid bony pelvis and the soft tissues of the cervix, the pelvic floor, the vagina, and the introitus (the external opening to the vagina). Although the soft tissues, particularly the muscular layers of the pelvic floor, contribute to vaginal birth of the fetus, the maternal pelvis plays a far greater role in the labor process because the fetus must successfully accommodate itself to this relatively rigid passageway. The size and shape of the pelvis can be determined at the initial prenatal visit or on admission in labor. This information can then be used in the assessment of labor progress (Thorp, 2009). The anatomy of the bony pelvis is described in Chapter 3. The following discussion focuses on the importance of pelvic configurations as they relate to the labor process. (It may be helpful to refer to Figs. 3-4 and 3-5.) The bony pelvis is formed by the fusion of the ilium, ischium, pubis, and sacral bones. The four pelvic joints are the symphysis pubis, the right and left sacroiliac joints (Fig. 13-7, A), and the sacrococcygeal joint (Fig. 13-7, B). The bony pelvis is separated by the brim, or inlet, into two parts: the false and the true pelves. The false pelvis is the part above the brim and plays no part in childbearing. The true pelvis, the part involved in birth, is divided into three planes: the inlet, or brim; the midpelvis, or cavity; and the outlet. The pelvic outlet is the lower border of the true pelvis. Viewed from below it is ovoid; somewhat diamond shaped; and bounded by the pubic arch anteriorly, the ischial tuberosities laterally, and the tip of the coccyx posteriorly (see Fig. 13-7, B). In the latter part of pregnancy the coccyx is movable unless it has been broken (e.g., in a fall during skiing or skating) and has fused to the sacrum during healing. The pelvic canal varies in size and shape at various levels. The diameters at the plane of the pelvic inlet, midpelvis, and outlet plus the axis of the birth canal (Fig. 13-8) determine whether vaginal birth is possible and the manner by which the fetus may pass down the birth canal. The subpubic angle, which determines the type of pubic arch, together with the length of the pubic rami and the intertuberous diameter, is of great importance. Because the fetus must first pass beneath the pubic arch, a narrow subpubic angle is less accommodating than a rounded wide arch. The method of measurement of the subpubic arch is shown in Fig. 13-9. A summary of obstetric measurements is given in Table 13-1. TABLE 13-1 *From Seidel HM, Ball JW, Dains JE, et al: Mosby’s guide to physical examination, ed 7, St Louis, 2011, Mosby.
Labor and Birth Processes
Factors Affecting Labor
Passenger
Size of the Fetal Head
Fetal Presentation
Fetal Lie
Fetal Attitude
Fetal Position
Passageway
Bony Pelvis
PLANE
DIAMETER
MEASUREMENTS
Inlet (Superior Strait)
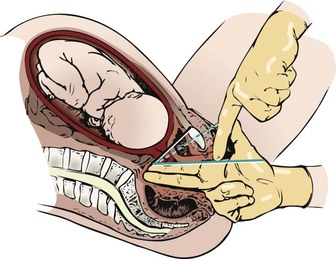
Length of diagonal conjugate (solid colored line), obstetric conjugate (broken colored line), and true conjugate (blue line)*
Conjugates
12.5-13 cm
1.5-2 cm less than diagonal (radiographic)
≥11 cm (12.5) (radiographic)
Midplane
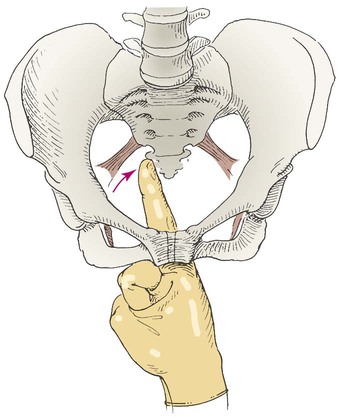
Measurement of interspinous diameter*
Transverse diameter (interspinous diameter)
10.5 cm
The midplane of the pelvis normally is its largest plane and the one of greatest diameter
Outlet
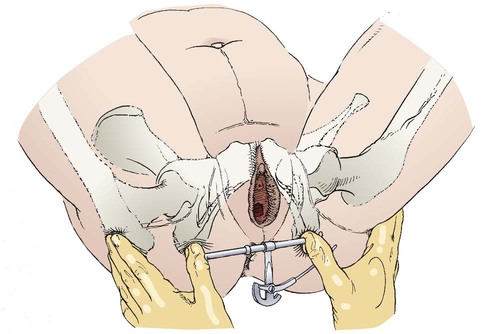
Use of Thom’s pelvimeter to measure intertuberous diameter*
Transverse diameter (intertuberous diameter) (biischial)
≥8 cm
The outlet presents the smallest plane of the pelvic canal
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Labor and Birth Processes
Get Clinical Tree app for offline access