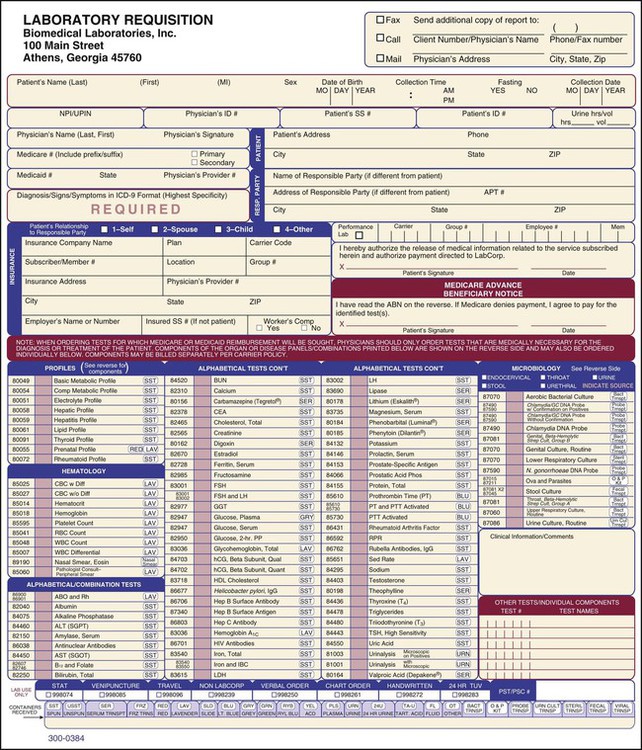
4. Describe the relationship between the medical office and an outside laboratory. 5. List the information included in a laboratory directory. 6. Identify the purpose of a laboratory request form. List and explain the function of each type of information included on the form. 7. Identify the use of each of the following profiles, and list the tests included in each: 8. Identify the purpose of the laboratory report form, and list the information included on it. 9. Describe the advantages of using a computer to send and receive laboratory documents. 12. List examples of specimens. 13. Identify and explain the guidelines that should be followed during specimen collection. 14. Explain why specimens must be handled and stored properly. 15. Identify the proper handling and storage techniques for each of the following specimens: blood, urine, microbiologic specimen, and stool specimen. 18. List the advantages of an automated blood analyzer. 19. Explain the purpose of quality control in the laboratory, and list quality control methods that should be employed when a CLIA-waived laboratory test is performed. 20. List the laboratory safety guidelines that should be followed in the medical office to prevent accidents. 1. Laboratory tests are most frequently ordered by the physician to assist in the diagnosis of pathologic conditions. Along with the health history and the physical examination, laboratory test results provide the physician with essential data needed to arrive at a diagnosis and prescribe treatment. After obtaining the health history and performing the physical examination, the physician may order laboratory tests for these reasons: • To confirm a clinical diagnosis. A clinical diagnosis is defined as a tentative diagnosis of a patient’s condition obtained through the evaluation of the health history and the physical examination, without the benefit of laboratory or diagnostic tests. • The patient’s signs and symptoms may provide a strong clinical diagnosis of a particular condition, and the physician may order laboratory tests simply to confirm that diagnosis. For example, the patient may have the typical signs and symptoms of diabetes mellitus, which would provide the physician with a fairly certain clinical diagnosis. In this instance, an oral glucose tolerance test (OGTT) may be ordered to confirm the diagnosis and to institute therapy. • To assist in the differential diagnosis of a patient’s condition. Two or more diseases may have similar signs and symptoms; the physician orders laboratory tests to assist in the differential diagnosis of the patient’s condition. A diagnosis of streptococcal sore throat must be made with a laboratory test to differentiate it from other pathologic conditions with similar signs and symptoms, such as pharyngitis. • To obtain information regarding a patient’s condition when not enough concrete evidence exists to support a clinical diagnosis. The patient sometimes may have vague signs and symptoms, and laboratory tests are ordered to obtain information on what may be causing the patient’s problem. For example, the patient may have nonspecific abdominal pain, and the physical examination may not yield enough information to support a clinical diagnosis. In this case, the physician may order a series of laboratory and diagnostic tests to assist in pinpointing the cause of the patient’s problems. 2. To evaluate the patient’s progress and to regulate treatment. When a diagnosis has been made, laboratory testing may be performed to evaluate the patient’s progress and to regulate treatment. On the basis of the laboratory results, the therapy may need to be adjusted or further treatment prescribed. A patient undergoing iron therapy for iron-deficiency anemia should have a complete blood count (CBC) performed every month to assess the response to treatment and to ensure that the condition is improving. Another example is a patient who has had a cardiac valve replaced and is taking warfarin (Coumadin), an anticoagulant used to inhibit blood clotting. The patient must have a prothrombin time test at regular intervals to assess the clotting ability of the blood. On the basis of the test results, the medication may need to be adjusted to ensure the dosage is at a safe level. A patient with diabetes who measures his or her blood glucose level each day to regulate insulin dosage provides another example of laboratory tests used to regulate treatment. 3. To establish a baseline level. On the basis of such factors as age, gender, race, and geographic location, individuals have different normal levels within the established reference range for a particular test. In this respect, laboratory tests also can serve to establish each patient’s baseline level with which future results can be compared. A patient who is going to receive warfarin (Coumadin) therapy should have a blood specimen drawn for a prothrombin time test before administration of this anticoagulant. The results serve as a baseline recording for that particular patient against which future prothrombin time test results can be compared. 4. To prevent or reduce the severity of disease. Laboratory tests also can help to prevent or reduce the severity of disease through early detection of abnormal findings. Certain conditions, such as high cholesterol, anemia, and diabetes, are relatively common disorders and sometimes may exist without symptoms in a patient, especially early in the development of the disease. Laboratory tests known as routine tests are performed on a routine basis on apparently healthy patients (usually as part of a general physical examination) to assist in the early detection of disease. These tests are relatively easy to perform and present a minimal hazard to the patient. The most commonly used routine tests are urinalysis, CBC, and routine blood chemistries. 5. To comply with state laws. Another reason for a laboratory test is its requirement by state law. The statutes of most states require a gonorrhea and syphilis test to be performed on pregnant women. The purpose of these tests is to protect the mother and fetus from harm by screening for the presence of these sexually transmitted diseases. Generally, laboratory tests that are CLIA-waived and commonly required, such as glucose determination and urinalysis, are performed in the POL (Figure 29-1). CLIA (Clinical Laboratories Improvement Amendments) consists of regulations developed in 1988 by the federal government to improve the quality of laboratory testing in the United States. A waived test is a laboratory test that has been determined by CLIA to be a simple procedure that is easy to perform and has a low risk of erroneous test results. CLIA regulations are described in greater detail later in this chapter. Equipment and supplies necessary to comply with the OSHA Standard should be readily accessible in the POL. These supplies include handwashing facilities, alcohol-based hand rubs, gloves, safety goggles and masks, safety-engineered syringes and needles, and biohazard sharps containers and biohazard trash bags. An eyewash station (Figure 29-2) is also recommended in the event of an exposure incident to the mucous membranes of the eyes, nose, or mouth. The outside laboratory provides the medical office with a laboratory directory (Figure 29-3), which serves as a valuable reference source for the proper collection and handling of specimens for transport to the outside laboratory. The laboratory may also maintain a website that includes a test menu of the specimen collection and handling requirements for each test performed by that laboratory. This allows the medical assistant to access this information easily and quickly using one or more of the following: a search box, an alphabetical index, or drop-down lists. If, after referring to the laboratory directory (or laboratory website), the medical assistant has a question regarding any aspect of the collection and handling of the specimen that is not clear, the laboratory should be contacted before proceeding. • Name and CPT code of the test • Amount and type of specimen required • Supplies necessary for collection of the specimen (e.g., blood tubes) • Techniques to be used for collection of the specimen • Proper handling and storage of the specimen • Instructions for transporting the specimen • Causes for rejection of the specimen by the laboratory • Uses and limitations of the test Table 29-1 is a (modified) table of representative tests included in a laboratory directory to provide an overall understanding of the information included in a laboratory directory. The information presented in this modified directory includes all of the categories listed above with the exception of the following: special instructions, instructions for transporting the specimen, uses and limitations of the test, and methodology used to perform the test. (Note: Refer to Figure 29-8 for an example of a laboratory test exactly as it is presented in a laboratory directory.) Table 29-1 Representative Tests from a (Modified) Laboratory Directory Collection and testing of a specimen can be categorized as follows: 1. The specimen is collected and tested at the medical office. 2. The specimen is collected at the medical office and transferred to an outside laboratory for testing. 3. The patient is given a laboratory request to have the specimen collected and tested at an outside laboratory. A laboratory request is a printed form that contains a list of the most frequently ordered laboratory tests (Figure 29-4). A laboratory request is required when the specimen is collected at the medical office and transferred to an outside laboratory for testing, or when the specimen is to be collected and tested at an outside laboratory, in which case the request is given to the patient at the medical office to take to the laboratory. The request provides the outside laboratory with essential information necessary for accurate testing, reporting of results, and billing. Organizational formats for the request forms vary, depending on the laboratory. In general, most outside laboratories find it more convenient and economical to provide the medical office with one form for designating all tests, with the possible exception of the Pap test, in which case a separate form, known as a cytology request, is provided. 1. Physician’s name and address. The physician’s name and address should be clearly indicated on the laboratory request form to facilitate the reporting of test results to the physician. Laboratory request forms are usually prenumbered with the physician’s account number, which assists in identification, reporting, and billing of laboratory tests. 2. Patient’s name and address. The patient’s name and address must be documented on the form as requested by the laboratory; for example, the laboratory may want the patient’s name designated with the last name first, middle initial, and then first name. The patient’s address is needed for billing purposes and must include the city, state, and zip code. 3. Patient’s age and gender. The reference ranges for some tests vary depending on the patient’s age and gender. The reference range for hemoglobin concentration varies according to gender (12 to 16 g/dL for a woman; 14 to 18 g/dL for a man). 4. Date and time of collection of the specimen. The date of the specimen collection indicates to the laboratory the number of days that have passed since the collection, providing the laboratory with information regarding the freshness of the specimen. A time lapse that is too long between collection and testing of a specimen may affect the accuracy of some test results. The time of collection is significant with respect to certain laboratory tests. The reference range for serum cortisol varies depending on whether the specimen is collected in the morning or in the afternoon. 5. Laboratory tests desired. The tests desired by the physician are usually indicated by marking a box adjacent to those tests (and their corresponding CPT code), as illustrated in Figure 29-3. A space designated as “additional tests” or “other tests” is provided on the laboratory request form for specifying the CPT code of a test that is desired but not listed on the request form. As previously indicated, the laboratory request form includes only the tests most frequently ordered. The laboratory directory contains a complete listing of all tests performed by the laboratory. 6. Profiles. Laboratory tests termed profiles may be ordered by the physician. A profile (also known as a panel) consists of an array of laboratory tests that have been determined to be the most sensitive and specific means of identifying a disease state or evaluating a particular organ or organ system. The profiles performed by an outside laboratory and the tests included in each are listed in the laboratory directory. A profile may be specific in nature, that is, all tests included relate to a specific organ of the body or a particular disease state. A specific profile is usually ordered when the physician does not have a definite clinical diagnosis but has a good idea of the patient’s condition or what organ or organs are involved in the patient’s condition. The physician orders a profile of the condition or organ in question. An example of a profile used to identify a disease state is the rheumatoid profile, which is used to assist in the diagnosis of rheumatoid arthritis. An example of a profile used to evaluate an organ is the hepatic function profile, which is used to assess liver function and to assist in the diagnosis of a pathologic condition that affects the liver. A profile also may be general in nature. A general metabolic profile contains numerous routine laboratory tests and is used primarily in a routine health screen of a patient. General metabolic profiles are used to detect any changes in the body’s biologic processes that may be present, although the patient may not have had any symptoms to indicate that these changes have occurred. General metabolic profiles also are used when the patient’s symptoms are so vague that the physician does not have enough concrete evidence to support a clinical diagnosis of a specific organ or disease state. An example of a general profile is the comprehensive metabolic profile; refer to Table 29-3 for a list of the tests included in this profile. The medical assistant should have knowledge of the names of common profiles and the tests generally contained in each, which are listed in Table 29-2. The tests contained in each profile may vary slightly from one laboratory to another. Table 29-2
Introduction to the Clinical Laboratory
LEARNING OBJECTIVES
PROCEDURES
Clinical Laboratory
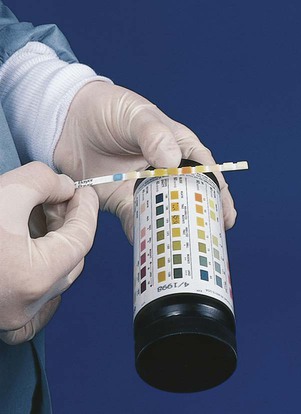
1. Explain the general purpose of a laboratory test.
Use a laboratory directory.
2. Identify and define the eight categories of a laboratory test on the basis of function. List examples of tests included under each category.
Complete a laboratory request form.
3. List and explain specific uses of laboratory test results.
Read a laboratory report.
Instruct a patient on the preparation necessary for a laboratory test that requires fasting.
10. Explain how an EMR program can be used to prepare a flow sheet for tests performed on a routine basis.
Maintain laboratory test results using flow sheets.
Collecting, Transporting, and Handling Specimens
11. Explain the purpose of advance patient preparation for the collection of a laboratory specimen.
Collect a specimen.
Handle and store a specimen.
Laboratory Testing in the Medical Office
16. Describe the following CLIA test categories: waived, moderately complex, and highly complex.
Perform a CLIA-waived laboratory test by following the manufacturer’s instructions.
Perform quality control procedures when utilizing a CLIA-waived laboratory test.
Practice laboratory safety.
Introduction to the Clinical Laboratory
Purpose of Laboratory Testing
Types of Clinical Laboratories
Physician’s Office Laboratory
Physical Structure of the POL

Laboratory Directory
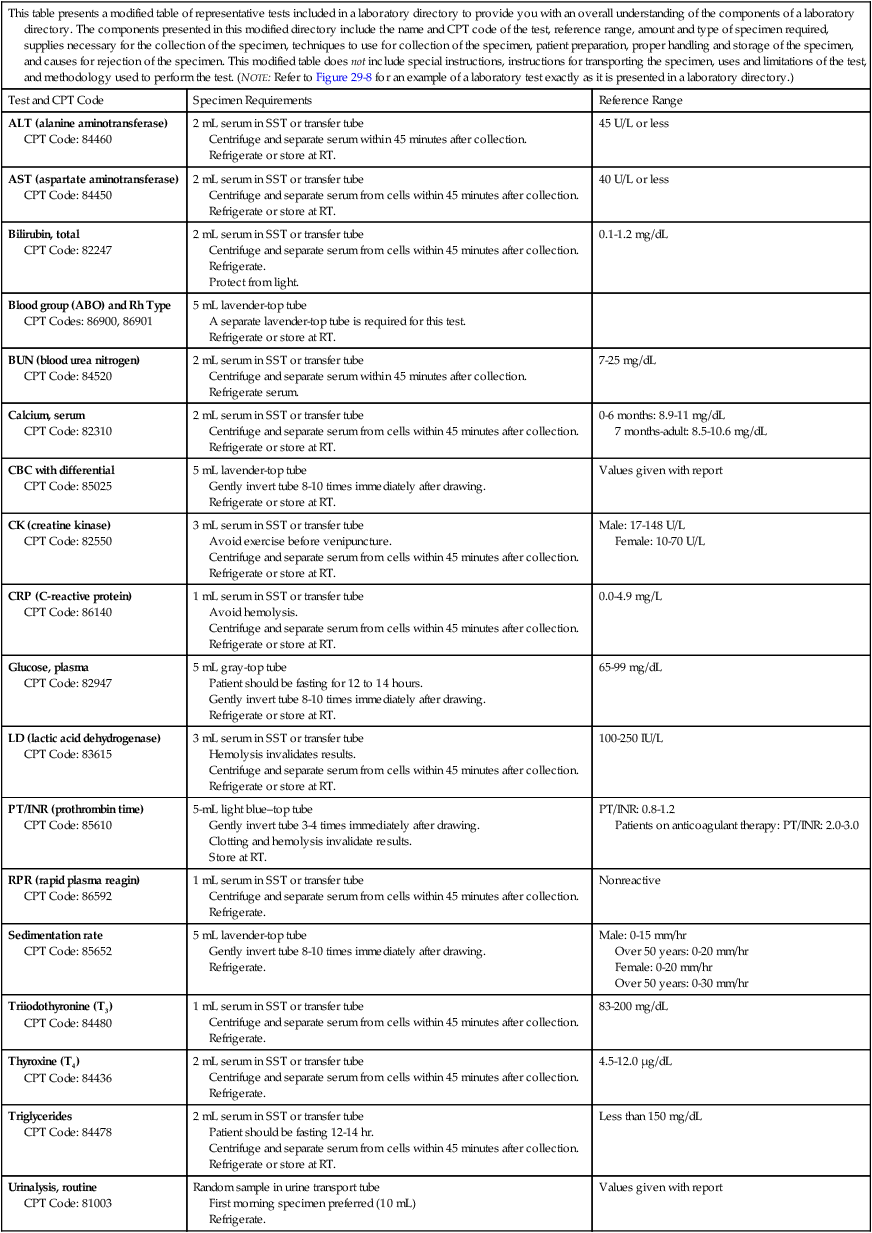
This table presents a modified table of representative tests included in a laboratory directory to provide you with an overall understanding of the components of a laboratory directory. The components presented in this modified directory include the name and CPT code of the test, reference range, amount and type of specimen required, supplies necessary for the collection of the specimen, techniques to use for collection of the specimen, patient preparation, proper handling and storage of the specimen, and causes for rejection of the specimen. This modified table does not include special instructions, instructions for transporting the specimen, uses and limitations of the test, and methodology used to perform the test. (NOTE: Refer to Figure 29-8 for an example of a laboratory test exactly as it is presented in a laboratory directory.)
Test and CPT Code
Specimen Requirements
Reference Range
ALT (alanine aminotransferase)
CPT Code: 84460
2 mL serum in SST or transfer tube
Centrifuge and separate serum within 45 minutes after collection.
Refrigerate or store at RT.
45 U/L or less
AST (aspartate aminotransferase)
CPT Code: 84450
2 mL serum in SST or transfer tube
Centrifuge and separate serum from cells within 45 minutes after collection.
Refrigerate or store at RT.
40 U/L or less
Bilirubin, total
CPT Code: 82247
2 mL serum in SST or transfer tube
Centrifuge and separate serum from cells within 45 minutes after collection.
Refrigerate.
Protect from light.
0.1-1.2 mg/dL
Blood group (ABO) and Rh Type
CPT Codes: 86900, 86901
5 mL lavender-top tube
A separate lavender-top tube is required for this test.
Refrigerate or store at RT.
BUN (blood urea nitrogen)
CPT Code: 84520
2 mL serum in SST or transfer tube
Centrifuge and separate serum within 45 minutes after collection.
Refrigerate serum.
7-25 mg/dL
Calcium, serum
CPT Code: 82310
2 mL serum in SST or transfer tube
Centrifuge and separate serum from cells within 45 minutes after collection.
Refrigerate or store at RT.
0-6 months: 8.9-11 mg/dL
7 months-adult: 8.5-10.6 mg/dL
CBC with differential
CPT Code: 85025
5 mL lavender-top tube
Gently invert tube 8-10 times immediately after drawing.
Refrigerate or store at RT.
Values given with report
CK (creatine kinase)
CPT Code: 82550
3 mL serum in SST or transfer tube
Avoid exercise before venipuncture.
Centrifuge and separate serum from cells within 45 minutes after collection.
Refrigerate or store at RT.
Male: 17-148 U/L
Female: 10-70 U/L
CRP (C-reactive protein)
CPT Code: 86140
1 mL serum in SST or transfer tube
Avoid hemolysis.
Centrifuge and separate serum from cells within 45 minutes after collection.
Refrigerate or store at RT.
0.0-4.9 mg/L
Glucose, plasma
CPT Code: 82947
5 mL gray-top tube
Patient should be fasting for 12 to 14 hours.
Gently invert tube 8-10 times immediately after drawing.
Refrigerate or store at RT.
65-99 mg/dL
LD (lactic acid dehydrogenase)
CPT Code: 83615
3 mL serum in SST or transfer tube
Hemolysis invalidates results.
Centrifuge and separate serum from cells within 45 minutes after collection.
Refrigerate or store at RT.
100-250 IU/L
PT/INR (prothrombin time)
CPT Code: 85610
5-mL light blue–top tube
Gently invert tube 3-4 times immediately after drawing.
Clotting and hemolysis invalidate results.
Store at RT.
PT/INR: 0.8-1.2
Patients on anticoagulant therapy: PT/INR: 2.0-3.0
RPR (rapid plasma reagin)
CPT Code: 86592
1 mL serum in SST or transfer tube
Centrifuge and separate serum from cells within 45 minutes after collection.
Refrigerate.
Nonreactive
Sedimentation rate
CPT Code: 85652
5 mL lavender-top tube
Gently invert tube 8-10 times immediately after drawing.
Refrigerate.
Male: 0-15 mm/hr
Over 50 years: 0-20 mm/hr
Female: 0-20 mm/hr
Over 50 years: 0-30 mm/hr
Triiodothyronine (T3)
CPT Code: 84480
1 mL serum in SST or transfer tube
Centrifuge and separate serum from cells within 45 minutes after collection.
Refrigerate.
83-200 mg/dL
Thyroxine (T4)
CPT Code: 84436
2 mL serum in SST or transfer tube
Centrifuge and separate serum from cells within 45 minutes after collection.
Refrigerate.
4.5-12.0 µg/dL
Triglycerides
CPT Code: 84478
2 mL serum in SST or transfer tube
Patient should be fasting 12-14 hr.
Centrifuge and separate serum from cells within 45 minutes after collection.
Refrigerate or store at RT.
Less than 150 mg/dL
Urinalysis, routine
CPT Code: 81003
Random sample in urine transport tube
First morning specimen preferred (10 mL)
Refrigerate.
Values given with report
Collection and Testing Categories
Laboratory Requests
Purpose
Parts of Laboratory Request Form
Profile
Tests Included
Use
Comprehensive metabolic profile
Albumin
ALP
ALT
AST
Bilirubin (Total)
BUN
Calcium
Carbon Dioxide
Chloride
Creatinine
Glucose
Inorganic Phosphorus
Potassium
Protein (Total)
Sodium
Triglycerides
General health screen that provides information on kidneys, liver, acid-base balance, blood glucose level, and blood proteins. Used to evaluate organ function and to check for conditions such as diabetes, liver disease, and kidney disease.
Routinely ordered as part of blood workup for physical examination or medical examination (particularly when patient’s symptoms are vague).
Abnormal test results are usually followed up with more specific tests before a diagnosis is made.
Electrolyte profile
Carbon Dioxide
Chloride
Potassium
Sodium
Screen for electrolyte or acid-base imbalance and monitor effect of treatment on disease or condition that causes electrolyte imbalance.
This profile also is used to evaluate patient taking medication that can cause electrolyte imbalance.
Hepatic profile
Albumin
ALP
ALT
AST
Bilirubin (Direct)
Bilirubin (Total)
Protein (Total)
Detection of pathologic conditions affecting the liver.
This test is often ordered when symptoms indicating a liver condition occur, such as jaundice, dark urine, light-colored bowel movements, or pain or swelling in the abdomen.
This profile may be ordered when an individual has been exposed to hepatitis, has a family history of liver disease, has excessive alcohol consumption, or is taking medication that can result in liver damage.
Hepatitis profile
Hepatitis A Antibody, IgM
Hepatitis B Core Antibody, Total
Hepatitis B Surface Antigen
Hepatitis C Antibody
Detection of viral hepatitis.
Lipid profile
Total Cholesterol
LDL Cholesterol
HDL Cholesterol
Triglycerides
VLDL Cholesterol (Calculation)
Total Cholesterol/HDL
Ratio (Calculation)
Determine risk of coronary artery disease.
Prenatal profile
ABO Grouping and Rh
Typing
CBC W/Diff and W/Plt
Hepatitis B Surface
Antigen
Red Cell Antibody Screen
Rubella Antibody Screen
Syphilis Serology (RPR)
Establish baseline recordings and screenings of prenatal patients for disease or potential problems.
Renal function profile
Albumin
BUN
Calcium
Carbon Dioxide
Chloride
Creatinine
Glucose
Phosphorus
Potassium
Sodium
Detection of kidney problems.
This profile shows how well the kidneys are functioning to remove excess fluid and waste.
When a problem is detected, diagnostic imaging tests may be used for further evaluation and diagnosis.
Rheumatoid profile
ANA
CRP
Rheumatoid Factor
Sedimentation Rate
Streptolysin O
Uric Acid
Assist in diagnosis of rheumatoid arthritis and help distinguish it from other forms of arthritis and conditions with similar symptoms.
This profile also is used to evaluate severity of rheumatoid arthritis, to monitor the condition and its complications, and to assess response to treatment.
Thyroid function profile
FTI
Thyroxine (T4)
Triiodothyronine (T3)
Uptake
Detection of conditions affecting the thyroid gland.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree