High dependency care requiring a nurse-to-patient ratio of 0.5:1
Intensive care requiring a nurse-to-patient ratio of 1:1
The dependency of a Level 1 patient increases to Level 2 if the child is nursed in a cubicle.
Intensive care requiring a nurse-to-patient ratio of 1.5:1
The dependency of a Level 2 patient increases to Level 3 if the child is nursed in a cubicle.
Intensive care requiring a nurse-to-patient ratio of 2:1
Commissioning Auditing and Costing
The DH utilises a non-clinical system to assess levels of care and dependency for audit and costing purposes. Health care Resource Groups (HRGs) have been used to cost care since 2007, based on seven levels:
- HRG1 – High Dependency (HD1)
- HRG2 – High Dependency Advanced (HD2)
- HRG3 – Intensive Care Basic (IC1)
- HRG4 – Intensive Care Basic Enhanced (IC2)
- HRG5 – Intensive Care Advanced (IC3)
- HRG6 – Intensive Care Advanced Enhanced (IC4)
- HRG7 – Intensive Care – ECMO/ECLS (IC5)
While this further division of dependency may be more sensitive, it is widely regarded as too cumbersome and complex for clinical use and takes no account of the individual and holistic care needs for the child’s parents or carers and siblings.
Standards for Staffing and Skill Mix
A fundamental issue in the commissioning and management of paediatric intensive care services is the number of nurses required to ensure safe, high quality care, bearing in mind the unpredictable dependency of patients and rate of bed occupancy. Murphy and Morris (2008) performed an audit of 10 PICUs and found that 83% of costs were staff-related, with the largest being nursing. Workforce planning is also affected by the number of beds, the layout of the unit and the number of single rooms. The recent introduction of Agenda for Change has also increased the whole-time equivalent (WTE) from the traditional benchmark of 6.4 WTE per bed to 6.7 WTE on an average unit due to the increased annual leave entitlement for experienced nurses (Paediatric Intensive Care Society 2010).
Commissioners of paediatric intensive care services have had to take into consideration the seasonal fluctuation many units experience and the effect this has on bed capacity. Many commissioners plan nursing staff levels based on an average bed capacity of 80%, however this can be problematic at times of peak capacity when it may be necessary to ask staff who are already working to their full capacity to undertake extra shifts or employ bank and agency staff, which can both impact on quality of care and be costly. Some units have used annualised hours for part-time staff, enabling them to undertake more planned shifts in busy periods and more leave in the summer.
In addition to annual leave, workforce planning needs to take into consideration additional burdens on staffing. Associated with the levels of patient dependency in paediatric intensive care are minimum recommended nurse-to-patient ratios, Level 2 being 1:1; Level 3 1.5:1 and Level 4 2:1. Furthermore, the need for a nurse in charge who has no direct responsibility for a particular patient, the need for a runner, staffing of retrieval teams, calculations for sickness (thought to be 5% of a WTE) and study leave for mandatory training need to be considered. The calculation of 6.7 WTE per bed the Paediatric Intensive Care Society recommend PICUs work towards does not include factors that can increase the WTE considerably, for example maternity leave which is difficult to anticipate and has to be incorporated into workforce planning on a case-by-case basis, as does study leave to undertake specialist paediatric intensive care courses and the level of supervision and induction new staff require and for how long. Table 1.2 summarises the Paediatric Intensive Care Society’s calculations.
Table 1.2 Summary of the Paediatric Intensive Care Society’s calculations
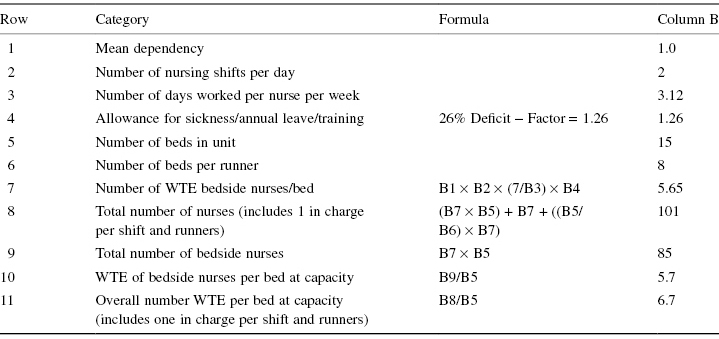
A worked example – A PICU with 15 beds with nurses working a two-shift/day roster (each nurse working 3–4 days a week). The mean dependency on the unit is a 1.0 nurse per patient per shift ratio and the average occupancy is 80%. The unit uses nurse runners, that is nurses with no allocated patient who check drugs and infusions, help set up equipment, assist with more dependent patients and cover meal-breaks.
The unit requires 4.65 WTE bedside nurses per bed for 80% occupancy. When one includes the runners and the nurse in charge (who should not be providing bedside care or meal-break cover) this rises to 5.38 WTE per bed. Commissioners must decide whether they want to staff to capacity (6.7 WTE/bed) to allow for peak demand (Paediatric Intensive Care Society 2010).
Consideration of the skill mix alongside minimum staffing levels is essential. However, it is difficult to match skill mix on a shift-by-shift basis, when the severity of illness of patients presenting may vary enormously. Current standards for nursing skill mix from the Paediatric Intensive Care Society recommend ‘that all PICUs should have a senior and experienced practitioner to coordinate and supervise less experienced nurses to ensure high quality care over the 24-hour period with a Registered Children’s Nurse at Band 7 or above and that all units should be managed overall by a Senior Nurse/Matron, Band 8a or above’ (Paediatric Intensive Care Society 2010, p. 44).
The most recent report of the UK PICU Staffing Survey (Tucker et al. 2009) indicates that the PICU workforce is highly qualified and highly skilled: 93% of nurses hold a children’s nursing registration, a third are senior nurses at Grade F or higher (pre-Agenda for Change) and identified in the skill mix for some units were advanced practitioners and nurse consultants. However, the survey did find that staffing, education and skill mix were increasingly problematic areas for some units, specifically in managing long-term sickness, difficulties in recruitment and retention, cuts in training budgets and increased pressure on beds. Furthermore, the reduction in junior doctors’ hours resulting from the European Working Time Directive seems to have had an impact, and the survey identified the substitution of junior medical staff with advanced nursing posts in some units.
Developing Roles in PICU
The current developments in nursing roles are underpinned by the policy document Modernising Nursing Careers (DH 2006) and the subsequent Towards a Framework for Post-Registration Nursing Careers: Consultation response report
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


