Chapter 38. Inherited conditions and the family
Maggie Kirk and Emer Parker
LEARNING OUTCOMES
• Appreciate the impact that a genetic illness may have on family life.
• Apply basic genetic principles to understand how genetic conditions can be passed on in families.
• Evaluate the role of the children’s nurse in helping families to access genetic information and supporting their decision making based on this.
• Appreciate some of the ethical issues surrounding the application of genetic technologies of relevance to children and their families.
Glossary
Alleles
The different forms that a gene may have at one particular position (or locus) on a chromosome.
Autosome
An ‘ordinary’ or non-sex chromosome.
Carrier
An individual who has a copy of a disease-causing gene, but does not have the disease. Such individuals are usually heterozygous for a recessive condition.
Dominant
A characteristic that is evident in an individual even when there is only one altered copy of a particular gene present.
Expressivity
The severity or extent to which a disease or condition is expressed.
Gene
The functional unit of inheritance, composed of a sequence of DNA.
Genome
All of the genetic information contained in the 23,000 or so genes carried on an individual’s chromosomes. The normal human genome comprises 22 pairs of autosomes, and one pair of sex chromosomes, as well as mitochondrial DNA.
Genotype
The genetic make-up of a person.
Hemizygous
Having just a single copy of a gene or DNA sequence, rather than the usual two. Men are normally hemizygous for most genes on the sex chromosomes.
Heterozygote
An individual who has two different forms of a particular gene.
Homozygote
An individual who has the same form of an allele on both chromosomes.
Karyotype
The chromosome make-up of an individual.
Multifactorial
Traits or conditions that are the result of interactions between different genes, and between genes and the environment.
Penetrance
The proportion of a population with a particular genotype that actually express that genotype. A condition that is not always expressed, even though the individual has the associated genotype, is said to have reduced penetrance.
Pharmacogenetics
The study of how different people respond to drugs due to their genetic make-up, in order to identify new, more specific and more effective drug targets with fewer side effects.
Phenotype
The observed characteristics of an individual.
Recessive
A characteristic that is apparent in an individual only when it is not masked by a dominant allele. Thus it is seen in the homozygous state (i.e. when both copies of the particular allele have been inherited), or in the hemizygous state.
Sex chromosomes
The X and Y chromosomes in humans.
Introduction: the genetics revolution
The interest that we have in how characteristics are passed down through the generations is demonstrated at a typical family gathering following the birth of a new baby. We like to identify who the baby most resembles, what features he or she may have inherited from a particular ‘side’ of the family. As the child grows and develops, the attribution of characteristics may be broadened from the mainly physical (he has his mother’s eyes) to include aspects of temperament (she has her father’s quick temper). With the advances in knowledge and understanding of the role that inheritance plays in our health and development, we have the potential to become more specific about the contribution of each parent to the features observed in their children. The range of features for which we can identify a genetic component will also increase, such as musicality, reading ability or sports performance. Of course parents (and grandparents) take pride in the positive attributes but how do they feel when a child has inherited a less desirable characteristic, such as an illness?
With the ‘genetics revolution’ we are beginning to appreciate far more the extent of the role that genes play in health and illness – and it is far more extensive than most people imagined, and more complex. Genes and environment interact along a continuum, with relatively rare disorders at the one end where genes alone will dictate the existence of disease, and at the other end, a few diseases in which environmental factors only play a part (Fig. 38.1). Most diseases, though, represent the outcome of the interactions between different genes, and between genes and the environment. Alongside our growing understanding of the nature and function of these genes and their interactions, we are also gaining knowledge of the role of some genes in protecting against disease, and of others in influencing our responses to medicines.
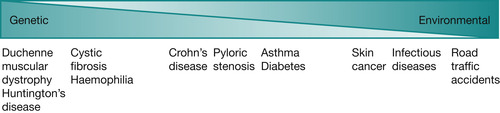 |
| Fig. 38.1 The contribution of genetic and environmental factors to health and disease. |
What is behind the genetics revolution is the Human Genome Project, the first phase of which was completed in 2003, 2 years ahead of schedule. This ambitious international project has deciphered the sequence of the chemicals that make up the DNA within the human blueprint (genome), paving the way for the next phase as our 23,000 or so genes are identified. Such advances in knowledge will have a profound impact on health care, with an increasing focus on individualised preventive medicine based on genetic risk, informed by environmental risk assessment. Bell (1998) outlined how genetics research would lead to the following:
• A new disease classification: based on the molecular mechanisms that cause disease rather than the clinical manifestation, e.g. in type 2 diabetes with the identification in particular of the maturity onset diabetes of the young (MODY) subtypes, based on the particular gene involved. There is also now a range of subsets of childhood leukaemia based on gene expression, chromosomal and molecular abnormalities. This will go alongside a better understanding of the pathological mechanisms of disease, and of the influence of environmental factors.
• The possibility of earlier detection of disease, with an increasing range of genetic tests: currently there are tests for around 200 of the 10,000 or so single gene disorders, and this number will grow as more and more genes are identified that account for these conditions. Genetic tests are also being developed to identify the genetic component of common diseases, and these will help identify people who may be at greater risk. Some genetic tests may become available commercially, as is already seen for example, for cystic fibrosis.
• Greater opportunities for prevention: by identifying individuals and sub-populations who might be more at risk, and identifying ways of modifying or preventing this risk.
• Better targeted and more effective treatments: using genotype to identify subtypes of populations who are more likely to display an enhanced response or increased toxicity. Those with the MODY subset HNF1α mutation are very sensitive to sulfonylureas for example.
• New types of treatment: with rational drug development based on an understanding of the pathogenesis, with a longer-term focus on gene therapy. Gene therapy trials are already being conducted worldwide for a range of conditions, including cystic fibrosis, inherited childhood blindness and leukaemia.
The implications of all these for individuals, families and professionals are far-reaching. Iredale (2000) reminds us that with earlier genetic testing and more prompt, targeted and improved treatments, including the potential for gene therapy, some diseases that were once fatal are being considered more as chronic. Thus children with such conditions are being seen not only by nurses in paediatric intensive care but in ambulatory paediatric and adolescent care settings.
The potential for misuse of new knowledge and technologies has also to be considered. We are in a unique position of knowing ahead of time the potential impact and in the UK new initiatives are already underway to help the health professional workforce to prepare for these advances.
The genetics White Paper
The UK government’s genetics White Paper ‘Our inheritance, our future’ detailed how the NHS should prepare for and respond to scientific advances to maximise the opportunities presented by genetics and meet the challenges it poses (Department of Health (DoH) 2003):
The new genetics knowledge and technology has the potential to bring enormous benefits for patients: more personalised prediction of risk, more accurate diagnosis, safer use of medicines and new treatment options
(DoH 2003 p 22).
The paper outlined that existing specialist genetics centres would continue to play a leading role in maximising the benefits of new genetics knowledge, and would be strengthened to cope with the increasing demand through capacity-building investment. In recognition of the need to prepare other (non-genetic) healthcare professionals as the impact of genetics moves across all areas of the NHS, the NHS National Genetics Education and Development Centre was established in 2004. Its role is to act as a catalyst in driving and coordinating activity to boost capability of the NHS workforce to incorporate genetics into healthcare practice.
 www
www
 www
wwwRead the genetics White Paper on line:
What are the four key action strands? Which do you think has the potential to impact most on your professional practice?
The White Paper acknowledged that the exact timing of the different advances is uncertain and this was echoed in the progress review of the White Paper (DoH 2008). The review outlined progress against a number of initiatives, including gene therapy and newborn screening, also reiterating that genetic testing will become increasingly widespread and useful, facilitating more accurate diagnosis. This will affect not only children and families with new conditions, but also those with pre-existing conditions where previously no diagnosis was available. What will this mean for families and what do we know already about how genetic diseases can affect family life?
The impact of genetic diseaseon family life
Family functioning is affected when a child becomes ill because of the usual stresses and practical problems associated with this. If the illness becomes prolonged, or if the child has a chronic condition, in particular one that is degenerative, these stresses are exacerbated. What part might the fact that a disease is ‘genetic’ play in this? Does it make any difference to the family?
The question of whether genetic conditions bring added stresses is an important one. Over the next 10–15 years there will be an increase in the number of children for whom a genetic diagnosis becomes possible, not only for children newly affected by a condition but also for those with existing, previously undiagnosed conditions, as genetic discoveries are made. Depending on the current policies surrounding the testing of children, there could also be an increase in the number of children for whom predictive testing would reveal a high risk of developing a condition, such as cardiomyopathy.
A mother’s account of her experiences following the diagnosis of two of her sons with adrenoleucodystrophy offers a powerful insight into how genetic diseases can impact on family life (McGowan 1999). Adrenoleucodystrophy is a degenerative metabolic disorder inherited as an X-linked condition; the variable range of symptoms is associated with a build up of fatty acids. McGowan says: ‘The diagnosis of an inherited condition can drop a bombshell into family relationships’ (p 197). She states earlier that: ‘We now take nothing for granted, such as the simple hopes that our sons will become teenagers or adult men’ (p 195).
Two mothers tell their stories of the impact of a genetic disease on family life on the website Telling Stories, Understanding Real Life Genetics (www.geneticseducation.nhs.uk/tellingstories). Sarah talks movingly of how she felt on being told her son’s diagnosis of Niemann–Pick disease, a lipid storage condition:
It’s such an overwhelming thing to be told that your son’s got a genetic disorder because your children’s lives are mapped out and you have hopes and dreams for them and to be told that things are going to be different for one of your children – it’s very hard.
Rachel has two children with cystic fibrosis. She writes:
How has it changed our life? In every way imaginable. Not expecting grandchildren. Spend a lot of time at the hospital. Daily routine is EXTREMELY different from that of parents of healthy children, we spend 2–2½ hours a day doing physio, three hours a day giving intravenous medicine at the moment, and have to give my son a total of 26 doses of oral medications per day, and my daughter a total of 11 doses of oral medications per day.
My marriage has been put under intense strain from all the emotional stress involved in caring for our children. Our children can’t live a normal life, and we can’t be normal parents. We don’t think the thoughts that normal parents would. We don’t take their health or life expectancy for granted. We try to make every moment count for them, because we don’t know how many they have. We take tons of photos, to remember as much as we can of them growing up.
Whyte (1992) studied four families caring for children with cystic fibrosis. As well as describing the stresses associated with the ‘chronic burden of care’, she analyses the part that the genetic nature of the illness plays and concluded that it has a profound effect. The assault on self-image and self-esteem of parents who feel they are unable to produce healthy children can be devastating, and the implications of this for future childbearing are keenly felt. Related to this are the tough decisions that parents may have to face about their reproductive options. This is especially challenging when parents may be considering an option to terminate a pregnancy following prenatal diagnosis. If they have an existing child with the condition, there may be worries that this could devalue that child, and explanations to the child could be difficult.
 Activity
Activity
 Activity
ActivityWhat circumstances can you think of where genetics will have an impact on family life? Make a list of the instances and compare these with those shown in the companion PowerPoint presentation. Read Rachel’s story in full at www.geneticseducation.nhs.uk/tellingstories/stories.asp?id=20 for the direct link.
So how do families with children affected by, or at risk of, genetic conditions adapt to the situation?Canam (1993) describes the tasks that parents have to face in adapting to chronic childhood illness:
• Accept the child’s condition
• Meet the normal developmental needs of the child
• Meet the developmental needs of other family members
• Cope with continuous stress and periodic crises
• Assist family members to manage their feelings
• Educate others about the child’s condition
• Establish a support system.
We will consider each of the stages in relation to genetic diseases.
Accepting the condition
Canam (1993) identifies acceptance as the first phase in the process. Seeking answers and a reduction of uncertainty are integral to this but a definitive diagnosis is not always available, particularly if the condition is rare. If the condition is one that is already ‘in the family’ the difficulties can vary. Many families may be accepting, with an established support system, but other parents have to cope with accusations of ‘irresponsibility’.
One factor that can have an impact on accepting a condition is its visibility. The shock of a major physical abnormality can be profound and the reactions of others on first meeting the child serve as a reminder of this. Lack of visibility can also make it more difficult for the family and others to accept. When the condition is associated with behavioural problems (such as autism or Tourette syndrome) its physical invisibility frequently presents problems with tolerance and understanding from others, both within and outside the family.
Fanos (1999) reported how acceptance by siblings may be influenced by the visibility of a condition in an affected brother or sister. She noted that the visibility of ataxia telangiectasia (a recessive condition characterised by unsteady gait and involuntary movements) caused less resentment of the time given to the child, less guilt and less tendency to idealise the affected sibling, than children with cystic fibrosis. However, it was associated with more embarrassment and shame.
Manage the condition on a day-to-day basis
The problems of coping with the practical matters of everyday living when a child (or any family member) has a chronic illness have been widely reviewed (see Chapter 44). A crucial factor in dealing with the problems are resources, including time, energy, money and social support systems, and the availability of all of these over an extended time. The extent of the resources needed will vary according to the specific condition. With a condition such as cystic fibrosis, for example, the child will need daily physiotherapy, regular visits to clinics, careful supervision of diet and may require frequent periods of hospitalisation. Medication will need to be given and regular supplies maintained. The extra workload may make full- or even part-time employment impractical for one parent. In managing the condition on a day-to-day basis, then, the parent may have to adjust to reduced career prospects, loss of role and problems with self-esteem. The latter may be a factor of the feelings of guilt at having passed on a condition to the child.
Meet the normal developmental needs of the child
The nature of the condition and how debilitating it is will clearly be a significant factor in how well the developmental needs of the child can be met. The instinctive desire to protect the child can be further fuelled by feelings of guilt, predisposing to ‘spoiling’ and children may take advantage of this. Labelling of the child by the family or by others can further compromise the situation.
 PROFESSIONAL CONVERSATION
PROFESSIONAL CONVERSATION

 PROFESSIONAL CONVERSATION
PROFESSIONAL CONVERSATIONI was enjoying my placement with the community paediatric team. I enjoyed meeting the families and seeing their care from another perspective, it is so different to the hospital setting. This particular visit was to see Lucy and her son Gareth. I knew them from previous admissions to the ward. Gareth is 7 years old and he has multiple problems – developmental delay, some autistic features and feeding problems. The reason for today’s visit was to discuss the genetic test results that Lucy was to have been given at the genetic clinic earlier that week.
The nurse spent the first few minutes catching up with Gareth’s progress, his feeding and his toilet training. Then she asked about the test results. Lucy started to cry as she explained that all the tests had come back negative. I did not understand why she was crying – surely this was good news to hear Gareth does not have a genetic condition. I listened while she talked about the guilt that she is responsible for Gareth’s problems, her description of her pregnancy, wondering if she had done something during this time that caused it all. I tried to reassure her reminding her that the geneticist had told her that it was not her fault. She turned to me and said ‘How can they say that if they do not know what did cause his problems?’
I did not know what to say.
Reflecting on this visit later I realised that my response to Lucy had been very naive. I had not thought about her position and that a positive result showing that her son had a serious genetic condition could be preferable to a negative one which left her with so many unanswered questions and a guilt that seemed could only be erased if she could replace it with certainty.

Meet the developmental needs of other family members
Fanos (1997) reminds us that the accessibility of a parent for the psychosocial support of a child is a crucial factor in his or her well-being. If the condition is an autosomal dominant one, a parent may already be trying to cope with his or her own illness, or that of the partner. With one (or more) child affected by a condition, the accessibility of the parents will be compromised – more so when they are grieving the death of an affected child. With frequent hospital stays, the availability of a parent on a day-to-day basis will also be severely limited. In a later study of the impact on siblings of boys with severe combined immunodeficiency disorder, most expressed distress over the prolonged absence of the mother during hospitalisation of the ill brother (Fanos & Puck 2001). They concluded that parents need help in balancing the needs of well siblings with those of an affected one.
 PROFESSIONAL CONVERSATION
PROFESSIONAL CONVERSATION
 PROFESSIONAL CONVERSATION
PROFESSIONAL CONVERSATIONThe Bradley family was well known to me – various members had been back and forth to the cystic fibrosis clinic over the years. Teresa was just 15 when she came and asked me about carrier testing for cystic fibrosis. Her cousin has the condition and her mum, older sister and another cousin are carriers, as well as her aunt and uncle of course. The family has always talked openly about cystic fibrosis and Teresa said she felt it was now her turn to be tested. I was a bit concerned because of her age, although she is quite mature and sensible, but also because I wondered how she might feel if she turned out not to have the gene. With so many of her family being carriers (in fact, all of the older females and the uncle) a negative result might exclude her from ‘the gang’. I don’t think the family had registered this and I know they would not knowingly exclude her but the potential for her to feel left out needed to be raised. 

Cope with continuous stress and periodic crises
Sickle-cell disease and cystic fibrosis (both autosomal recessive conditions) are typical examples of how the pattern of the illness is one of continuous stress, managing the condition on a daily basis with a regime of medication and other therapy, interspersed with crises, both familial and medical. A child in sickle-cell crisis (where the abnormally shaped red blood cells can cause infarction and necrosis) and a chest infection in a child with cystic fibrosis require prompt hospitalisation and aggressive clinical intervention. The gradual deterioration of a child with a degenerative condition such as Duchenne muscular dystrophy (X-linked) as he becomes increasingly dependent on his family, also provokes continuous stress.
The day-to-day fluctuations in condition and the uncertainty this brings make a major contribution to stress (Nereo et al., 2003 and Locker, 1991). To this symptomatic uncertainty is added the trajectory uncertainty of being able to predict the course and outcome of the disease. This is not only because of individual variation in gene expression, but also because of advances in management in a fast-moving research field, underpinning hopes for more effective treatments or even cure (through gene or stem cell therapy) in the future.
 Activity
Activity
 Activity
ActivityRead Merry France-Dawson’s story about her experiences of living with sickle-cell disease in ‘The troubled helix’ (France-Dawson 1996). She recalls overhearing her father being told she would not survive the night as a young girl in ITU over 30 years ago, and describes how she then ‘lived by instalments’.
Managing the family’s feelings
It is important to acknowledge the positive contribution that the child makes to the family, irrespective of the nature of the condition. Kearney & Griffin (2001) conceptualise the experiences of parents of children with developmental disability as being a dynamic between joy and sorrow. Although there are undoubtedly negative experiences, these can be balanced by positive feelings such as hope and humour. As McGowan expresses it: ‘My sons are special people, beyond their genetic flaw…’ (McGowan 1999 p 199).
Nonetheless, the sorrows can be profound and long-lasting, and other feelings such as guilt, blame, anger, fear, anxiety and depression can also be difficult to cope with. One factor that may be more apparent in families with a child affected by a genetic condition is the feeling of guilt. This can take the form of ‘survivor guilt’ in unaffected family members, including children. In one study examining the long-term psychological effects of genetic testing for a hereditary colorectal cancer, some children with a negative result and a positive-testing sibling demonstrated an increase in symptoms of anxiety at follow-up (Codori et al 2003).
The guilt that parents can feel can be overwhelming. In his book about his daughter Alex, Frank Deford recounts eloquently the impact of genetic disease on family life (Deford 1983). Alex had cystic fibrosis, and she lived until she was 8 years old. The story of Alex’s life, of the family’s struggle with her disease, and of her death is indescribably moving and essential reading for any children’s nurse. Deford captures some of the feelings that many parents may experience in this situation:
Ultimately, whether in my dealings with Carol [his wife], with Alex herself, with anyone involved with the disease – or with myself, for that matter – the major emotion pressing upon me was the feeling of inadequacy … And I could not explain how I felt, because of the shame, nor could I ever escape, because of the guilt.
(Deford 1983 p 96)
He goes on to say:
When our child was dying – when she was dying because of the genes we passed on to her – no matter how irrational it may have been to flagellate ourselves, there were times, in the mustiest corners of self-awareness, when we had to. Had to. I could not forgive Carol any more than I could forgive myself. After all, we quickly enough assume credit for the genes that make our children attractive and bright – she takes after me. It’s only human nature, then, that we also accept the responsibility when we pass on genes of destruction.
(Deford 1983 p 94)
Of course, such feelings are not the prerogative of parents in this situation. Many parents will blame themselves for contributing in some way to their child’s condition. However, with genetic disease, particularly the single gene disorders and chromosomal conditions, the cause may be clearly attributable to one or both parents. Furthermore, as the condition may be passed on to future generations, this may be accompanied by ongoing guilt and fear that subsequent children will also inherit it.
Get Clinical Tree app for offline access



