Identify the common etiologies of inflammation.
 Discuss the pathophysiology of inflammation.
Discuss the pathophysiology of inflammation.
 Describe, in general, the groups of drugs used to treat inflammation.
Describe, in general, the groups of drugs used to treat inflammation.
 Identify the common pathogens and methods of infection control.
Identify the common pathogens and methods of infection control.
 Discuss the pathophysiology of infection.
Discuss the pathophysiology of infection.
 Discuss ways to minimize emergence of drug-resistant microorganisms.
Discuss ways to minimize emergence of drug-resistant microorganisms.
 Discuss ways to increase the benefits and decrease the risk associated with antimicrobial drug therapy.
Discuss ways to increase the benefits and decrease the risk associated with antimicrobial drug therapy.
 Know how to apply the nursing process to the care of the patient who is receiving antimicrobial therapy.
Know how to apply the nursing process to the care of the patient who is receiving antimicrobial therapy.
Clinical Application Case Study
Alisa Warren is a 25-year-old woman with early-onset rheumatoid arthritis who works as a social worker in a pediatric hospital. She has a heavy caseload, and her lunch often consists of a soda, chips, and a sweet roll from the snack machine. She and her husband spend most evenings watching movies and television because her pain prevents her from participating in many activities. Recently, her practitioner prescribed methylprednisolone, a corticosteroid, to help manage the inflammation associated with the arthritis.
KEY TERMS
Antibacterial: ability to kill bacteria or interfere with the ability of bacteria to grow and replicate
Antibiotic: drug that has the ability to kill or inhibit bacterial growth and replication
Antibiotic resistance: ability of certain bacteria to survive and multiply in the presence of antibiotics
Anti-infective: agent or substance with antibacterial, antiviral, and antifungal properties
Anti-inflammatory agent: drug indicated when the inflammatory response is inappropriate, abnormal, or persistent, or destroys tissue
Antimicrobial agent: drug used to prevent or treat infections caused by pathogenic (disease-producing) microorganisms such as bacteria, fungi, viruses, and parasites
Bacteria: single-celled microorganisms that do not have nuclei and reproduce by fission or splitting
Bactericidal: agent that kills bacteria
Bacteriostatic: agent that inhibits bacterial growth and replication
Broad spectrum: effective against a wide range of bacteria
Colonization: presence and growth of microorganisms on host tissues
Community-acquired infection: infection caused by microorganisms that originated in a setting outside of a health care facility
Detection of antigens: technique to identify pathogens that uses features of culture and serology but reduces the time required for diagnosis
Fungi: plant-like microorganisms that live as parasites on living tissue or as saprophytes on decaying organic matter
Inflammation: immunological response to allergy, infection, or injury that increases the migration of leukocytes and blood flow to assist in repairing tissues
Nosocomial infection: infection acquired from microorganisms in hospitals and other health care facilities
Opportunistic: microorganisms in normal flora that become pathogenic under conditions that are favorable for their (over)growth
Penicillin-binding proteins: proteins in bacteria that serve as target sites for penicillin to bind
Serology: method of identifying infectious agents by measuring the antibody level (titer) in the serum of an infected host
Susceptibility: vulnerability of the bacteria to an antibiotic’s effects
Viruses: intracellular parasites that survive only in living tissues
Introduction
This chapter is an introduction to the pathophysiological effects of inflammation and infection. Readers should note that the format of this chapter is different from previous chapters. This chapter presents an overview of the anti-inflammatory and antimicrobial therapy to allow an understanding of a broad classification of the drugs involved and their impact on decreasing inflammation associated with infection and the infective process.
To help prevent inflammation caused by allergy, injury, or infection, the nurse should be familiar with anti-inflammatory agents. The anti-inflammatory agents administered to reduce the inflammatory process include aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroids. These drugs are indicated when the inflammatory response is inappropriate, abnormal, or persistent, or in the presence of tissue destruction. Health care providers use medicines known as antimicrobial agents to prevent or treat infections caused by pathogenic (disease-producing) microorganisms such as bacteria, fungi, viruses, and parasites. They treat inflammation resulting from infectious processes with antimicrobial drugs.
Most microorganisms live in equilibrium with the human host and do not cause disease; however, even beneficial bacteria may cause infections in certain conditions. When the balance is upset and infection occurs, characteristics of the infecting microorganisms and the adequacy of host defense mechanisms are major factors in determining the severity of the infection and the person’s ability to recover. In addition, overuse of antimicrobial agents may lead to serious infections caused by drug-resistant microorganisms. To help prevent infectious diseases and participate effectively in antimicrobial drug therapy, the nurse must be knowledgeable about microorganisms, host responses to microorganisms, and antimicrobial drugs.
Overview of Inflammation
To adequately understand the pharmacologic treatment of inflammation, it is important to understand the causes, pathophysiology, and clinical manifestations of inflammation. This will make it easier to understand the drug therapy associated with the treatment of inflammation, as addressed in Chapters 14 and 15.
Etiology
Inflammation is the cellular response of the body to injury. The cells and tissues of the body are killed or injured by chemical, physical, or infectious agents. The immunological response of the body produces increased migration of leukocytes and flow of blood to the cells and tissues affected to help repair the tissues.
Pathophysiology
There are two types of inflammation. Acute inflammation is the immediate response to injury of local tissues. The body responds by attempting to remove the offending agent to limit the amount of damage to the tissues affected. Chronic inflammation occurs over longer periods, even years. An acute inflammatory response may become chronic.
Acute Inflammation
The process of acute inflammation occurs in three stages. The first stage is the vascular stage; notable changes occur in the small blood vessels at the site of the cellular and tissue injury. At the time of the injury, vasoconstriction results, followed by vasodilation of the capillaries and venules to increase capillary blood flow, increasing temperature and redness at the site. The body then increases protein exudates into the extravascular spaces. As protein exudates occupy the extravascular spaces, the capillary osmotic pressure diminishes and the interstitial osmotic pressure increases, resulting in increasing amounts of fluid in the tissue spaces causing swelling, pain, and diminished function or mobility. In the event that the inflammation is caused by an infectious agent, the localizing effects increase the risk of the spread of infection (Fig. 13.1).
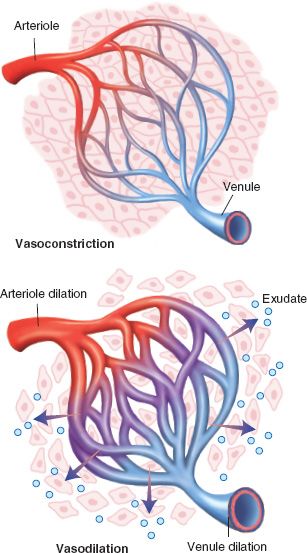
Figure 13.1 Stage 1: vascular stage. The vascular stage of acute inflammation, which is characterized by changes in the small blood vessels at the site of injury. It begins with vasoconstriction followed rapidly by vasodilation. Vasodilation results in an increase in capillary blood flow, causing heat and redness, which are two of the cardinal signs of inflammation. This is accompanied by an increased in vascular permeability with outpouring of protein-rich fluid (exudate) into the extravascular spaces. The loss of proteins reduces the capillary osmotic pressure and increases the interstitial osmotic pressure. This, coupled with an increase in capillary pressure, causes a marked outflow of fluid and its accumulation in the tissue spaces, producing the swelling, pain, and impaired function that represent the other cardinal signs of acute inflammation. As fluid moves out of the vessels, stagnation of flow and clotting of blood occur. This aids in localizing the spread of infectious microorganisms.
The second stage of acute inflammation is also known as the cellular stage. At this time, there is an influx of leukocytes, primarily neutrophils, to the injury site. As the leukocytes invade, there is a slowing of the blood flow and margination, which is the adhesion of the leukocytes to the wall of the blood vessels. The leukocytes then transmigrate from the vascular space to the extravascular tissue. They travel to the tissue injury site by chemotaxis (Fig. 13.2).
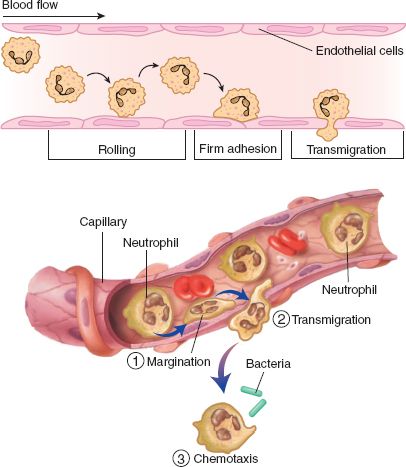
Figure 13.2 Stage 2: leukocyte margination, adhesion, and transmigration. The cellular stage of acute inflammation, which involves the delivery of leukocytes, mainly neutrophil, to the site of injury so they can perform their normal functions of host defense. The delivery and activation of leukocytes can be divided into the following steps: adhesion and margination, transmigration, and chemotaxis. The recruitment of leukocytes to the precapillary venules, where they exit the circulation, is facilitated by the slowing of blood flow and margination along the vessel surface. Leukocyte adhesion and transmigration from the vascular space into the extravascular tissue is facilitated by adhesion molecules on the leukocyte and endothelial surfaces. After extravasation, leukocytes migrate in the tissues toward the site of injury by chemotaxis, or locomotion oriented along a chemical gradient.
The third stage involves opsonization, which facilitates phagocytosis. During opsonization, a substance coats the foreign antigens, producing inflammation. This inflammation makes the antigens more susceptible to the macrophages and leukocytes, thus increasing phagocytic activity. The two opsonins are complement factor C3b and antibodies (Fig. 13.3).
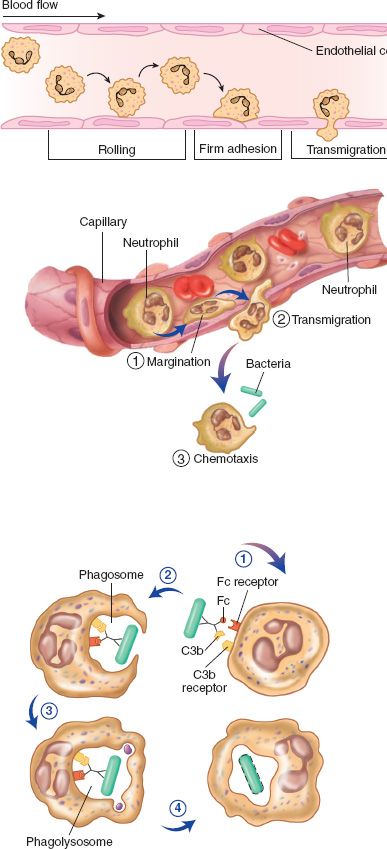
Figure 13.3 Stage 3: opsonization and phagocytosis. Once at the site of injury, the products generated by tissue injury trigger a number of leukocyte responses, including phagocytosis and cell killing. Opsonization of microbes (1) by complement factor C3b and antibody facilitates recognition by neutrophil C3b and the antibody Fc receptor. Receptor activation (2) triggers intracellular signaling and actin assembly in the neutrophil, leading to formation of pseudopods that enclose the microbe within a phagosome. The phagosome (3) then fuses with an intracellular lysosome to form a phagolysosome into which lysosomal enzymes and oxygen radicals (4) are released to kill and degrade the microbe.
Chronic Inflammation
There are two kinds of chronic inflammation. Nonspecific chronic inflammation is a diffuse accumulation of macrophages and lymphocytes in the area of tissue destruction, yielding fibroblast proliferation and scarring. Granulomatous chronic inflammation generates 1 to 2 mm granulomas made up of macrophages surrounded by lymphocytes. The granulomatous process results from foreign bodies that have not been controlled by the acute inflammatory process.
Clinical Manifestations
In acute inflammation, pain, redness, and swelling are apparent. Breaks in the integumentary system result in the drainage of exudate. In the event of a viral or bacterial infection associated with the inflammation, fever and general malaise sometimes occur. In chronic inflammation, tissue destruction and scarring may develop, resulting in diminished mobility. As previously stated, granulomas may occur because of an uncontrolled acute inflammatory process.
Drug Therapy
Aspirin, NSAIDs, and corticosteroids are administered to decrease inflammation (see Chaps. 14 and 15). Aspirin and NSAIDs block the synthesis of prostaglandin in the central and peripheral nervous systems. The anti-inflammatory response produced by the administration of corticosteroids occurs through the inhibition of interleukin-1, cytokines, and the tumor necrosis factor. Corticosteroids also impair phagocytosis by preventing phagocytic cells from leaving the bloodstream. They decrease the amount of lymphocytes, fibroblasts, and collagen needed for tissue repair.
Clinical Application 13-1
 Now that Ms. Warren has been given a corticosteroid to decrease the inflammation of her joints, what is she at risk for developing?
Now that Ms. Warren has been given a corticosteroid to decrease the inflammation of her joints, what is she at risk for developing?
Overview of Microorganisms
Infections occur when microorganisms invade a host, attach to host cell receptors, and multiply in sufficient numbers to cause injury. The infection stimulates the body’s immune response. In many instances, this immune response is sufficient to contain an infection. However, most microorganisms have characteristics that allow them to adapt to ensure their survival, and these adaptations help protect them from normal body defense mechanisms.
Antimicrobial drugs are an important intervention to treat infections that could otherwise cause significant injury and harm to the human host. To understand antimicrobial drug use, it is important to have a basic understanding of the microorganisms that they target. The following sections provide information about microorganisms and how they interact with human hosts.
Microorganisms that cause infectious disease include bacteria, viruses, fungi, and parasites. Bacteria are single-celled microorganisms without nuclei that reproduce by fission or splitting. They are classified according to whether they are aerobic (require oxygen) or anaerobic (cannot live in the presence of oxygen, their ability to retain Gram’s stain [gram positive] or to reject Gram’s stain [gram negative], and their shape [e.g., cocci, rods]). Antibiotics are antimicrobial drugs used to treat bacterial infections. Viruses are intracellular parasites that survive only in living tissues. They are officially classified according to their structure but are more commonly described according to origin and the disorders or symptoms they produce. Human pathogens include adenoviruses, herpesviruses, and retroviruses (see Chap. 21). Fungi are plant-like microorganisms that live as parasites on living tissue or as saprophytes on decaying organic matter. Approximately 50 species are pathogenic in humans (see Chap. 22). Parasites are microorganisms in the animal kingdom that infect other animals. Parasites that infect human hosts include arthropods, protozoa, and helminths (see Chap. 23).
Etiology
Normal Flora
Colonization is the presence and growth of microorganisms. The microorganisms do not necessarily cause tissue injury or elicit an immune response in the human body. The human body also has sterile areas, in which microorganisms do not live. Sterile areas that do not communicate directly with the external environment include organs such as the heart and liver, the musculoskeletal system, and body fluids such as urine. Areas typically populated by microorganisms include the skin, upper respiratory tract, and colon.
Normal skin flora includes staphylococci, streptococci, diphtheroids, and transient environmental microorganisms. The upper respiratory tract contains staphylococci, streptococci, pneumococci, and diphtheroids, as well as Haemophilus influenzae. The external genitalia contain skin organisms, and the vagina contains lactobacilli, Candida, and Bacteroides. The colon contains Escherichia coli, Klebsiella, Enterobacter, Proteus, Pseudomonas, Bacteroides, clostridia, lactobacilli, streptococci, and staphylococci.
Normal flora protects the human host in a variety of ways. For example, normal bowel flora synthesizes vitamin K and vitamin B complex. The intestinal flora also plays a role in digestion. Furthermore, by competing with potential pathogens for nutrients and by preventing adhesion and growth of pathogens, beneficial microorganisms interfere with the ability of potential pathogens to cause infections.
In certain instances, normal flora can become pathogenic. For example, microorganisms that are part of the normal flora and nonpathogenic in one area of the body may be pathogenic in other parts of the body; for example, E. coli is part of the normal intestinal flora but it is a common cause of urinary tract infections.
Host Defense Mechanisms
Although the numbers and virulence of microorganisms help determine whether a person acquires an infection, another major factor is the host’s ability to defend itself against the would-be invaders.
Major defense mechanisms of the human body are intact skin and mucous membranes, various anti-infective secretions, mechanical movements, phagocytic cells, and the immune and inflammatory processes. The skin prevents penetration of foreign particles, and its secretions and normal bacterial flora inhibit growth of pathogenic microorganisms. Secretions of the gastrointestinal, respiratory, and genitourinary tracts (e.g., gastric acid, mucus) kill, trap, or inhibit growth of microorganisms. Coughing, swallowing, and peristalsis help remove foreign particles and pathogens trapped in mucus, as does the movement of cilia. Phagocytic cells in various organs and tissues engulf and digest pathogens and cellular debris. The immune system produces lymphocytes and antibodies. The inflammatory process is the body’s response to injury by microorganisms, foreign particles, chemical agents, or physical irritation of tissues. Inflammation localizes, destroys, dilutes, or removes the injurious agents so tissue healing can occur (see previous discussion).
Many factors impair host defense mechanisms and predispose to infection by disease-producing microorganisms. These factors include the following:
• Breaks in the skin and mucous membranes related to trauma, inflammation, open lesions, or insertion of prosthetic devices, tubes, and catheters for diagnostic or therapeutic purposes
• Impaired blood supply
• Neutropenia and other blood disorders
• Malnutrition
• Poor personal hygiene
• Suppression of normal bacterial flora by antimicrobial drugs
• Suppression of the immune system and the inflammatory response by immunosuppressive drugs, cytotoxic anti- neoplastic drugs, and adrenal corticosteroids
• Diabetes mellitus and other chronic diseases
• Advanced age
Clinical Application 13-2
 Which alteration in Ms. Warren’s defense mechanisms places her at risk for the development of an infection?
Which alteration in Ms. Warren’s defense mechanisms places her at risk for the development of an infection?
NCLEX Success
1. A college student is seen in the campus health center with a sore throat. Examination of the throat reveals redness and swelling but no sign of infection. Which of the following is an accurate description of the inflammatory process?
A. A granuloma will develop if the inflammation is unresolved.
B. The student is not at risk for the development of an infection.
C. There is an influx of leukocytes to the throat.
D. Scarring will result from phagocytic action.
2. A sputum specimen report from the laboratory states, “Contamination with typical oral flora.” Which interpretation is correct?
A. Bacteria in the mouth are growing in the lungs.
B. The normal flora has become pathogenic.
C. The patient has a pulmonary infection.
D. The sputum from the lungs has mixed with bacteria in the mouth.
Pathophysiology
Infection begins with colonization by microorganisms. Infectious disease occurs when growth of microbial pathogens results in injury and is accompanied by clinical signs and symptoms indicative of an infection. Box 13.1 describes common bacterial pathogens of humans. Accurate assessment and documentation of symptoms can aid in early detection and diagnosis of infectious disease.
BOX 13.1 Common Bacterial Pathogens
Gram-Positive Bacteria
Staphylococci
Staphylococcus aureus bacteria are part of the normal microbial flora of the skin and upper respiratory tract and also are common pathogens. Some people carry (are colonized with) S. aureus in the anterior nares. The bacteria are spread mainly by direct contact with people who are infected or who are carriers. The hands of health care workers are considered a major source of indirect spread and nosocomial infections. The bacteria also survive on inanimate surfaces for long periods of time.
S. aureus organisms can cause skin infections such as boils and carbuncles. When burns or surgical wounds become contaminated with S. aureus, they often produce endotoxins that destroy erythrocytes, leukocytes, platelets, fibroblasts, and other human cells. These bacteria may also cause infections of the respiratory tract and urinary tract. Also, when many strains are ingested, they produce enterotoxins that cause food poisoning. The enterotoxins survive heating at temperatures high enough to kill the bacteria, so reheating foods does not prevent food poisoning.
High-risk groups for staphylococcal infections include newborns, older adults, and people who are malnourished or obese, or who have diabetes. In children, staphylococcal infections of the respiratory tract are most common in those younger than 2 years of age. In adults, staphylococcal pneumonia often occurs in people with chronic lung disease or as a secondary bacterial infection after influenza. The influenza virus destroys the ciliated epithelium of the respiratory tract and thereby aids bacterial invasion.
Staphylococcus species, nonaureus (SSNA) describes a group of bacteria that are also part of the normal microbial flora of the skin and mucosal surfaces and are increasingly common pathogens. The most common member of this group involved in infections is S. epidermidis.
Infections due to SSNA are often associated with the use of treatment devices such as intravascular catheters, prosthetic heart valves, cardiac pacemakers, orthopedic prostheses, cerebrospinal fluid shunts, and peritoneal catheters. SSNA infections include endocarditis, bacteremia, and other serious infections and are especially hazardous to immunocompromised patients. Treatment usually requires removal of any infected medical device as well as appropriate antibiotic therapy.
Streptococci
Certain streptococci are part of the normal microbial flora of the throat and nasopharynx in many healthy people. These bacteria do not usually cause disease unless the mucosal barrier is damaged by trauma, previous infection, or surgical manipulation. Such damage allows the bacteria to enter the bloodstream and gain access to other parts of the body where they colonize and then cause an infection.
S. pneumoniae bacteria, often called “pneumococci,” are common bacterial pathogens. They cause pneumonia, sinusitis, otitis media, and meningitis. Pneumococcal pneumonia usually develops when the mechanisms that normally expel inhaled microorganisms (i.e., the mucociliary blanket and cough reflex) are impaired by viral infection, smoking, immobility, or other insults. When S. pneumoniae reach the alveoli, they proliferate, cause acute inflammation, and spread rapidly to involve one or more lobes. Alveoli fill with proteinaceous fluid, neutrophils, and bacteria. Older adults have high rates of illness and death from pneumococcal pneumonia, which can often be prevented by pneumococcal vaccine (see Chap. 10). Pneumococcal sinusitis and otitis media usually follow a viral illness, such as the common cold. The viral infection injures the protective ciliated epithelium and fills the air spaces with nutrient-rich tissue fluid, in which the pneumococci thrive. S. pneumoniae is a common pathogen in bacterial sinusitis. In young children, upper respiratory tract infections may be complicated by acute sinusitis. Many children have repeated episodes of pneumococcal otitis media by 6 years of age. Recurrent otitis media during early childhood may result in reduced hearing acuity. Pneumococcal meningitis may develop from sinus or middle ear infections or an injury that allows pneumococcal bacteria from the nasopharynx to enter the meninges. S. pneumoniae infection is a common cause of bacterial meningitis in adults. Other potential secondary complications include septicemia, endocarditis, pericarditis, and empyema.
Streptococcus pyogenes (beta-hemolytic streptococcus) bacteria are often part of the normal flora of the skin and oropharynx that may become pathogenic in other body regions. The bacteria spread from person to person by direct contact with oral or respiratory secretions. They cause severe streptococcal pharyngitis (“strep throat”), scarlet fever, and rheumatic fever. Endocarditis and glomerulonephritis may occur as sequelae following untreated or inadequately treated streptococcal pharyngitis.
Enterococci
Enterococci are normal flora in the human intestine but are also found in soil, food, water, and animals. Although the genus Enterococcus contains approximately 12 species, the main pathogens are Enterococcus faecalis and Enterococcus faecium. Most enterococcal infections occur in hospitalized patients, especially those in critical care units. Risk factors for nosocomial infections include serious underlying disease, prior surgery, renal impairment, and the presence of urinary or vascular catheters. These bacteria, especially E. faecalis, are usually secondary invaders in urinary tract or wound infections. Enterococci may also cause endocarditis. This serious infection occurs most often in people with underlying heart disease, such as an injured valve. When the bacteria reach a heart valve, they multiply and release emboli of foreign particles into the bloodstream. Symptoms of endocarditis include fever, heart murmurs, enlarged spleen, and anemia. This infection is diagnosed by isolating enterococci from blood cultures. If not treated promptly and appropriately, enterococcal endocarditis may be fatal.
Gram-Negative Bacteria
Bacteroides
Bacteroides are anaerobic bacteria normally found in the digestive, respiratory, and genital tracts. They are the most common bacteria in the colon. Bacteroides fragilis, the major human pathogen, causes intraabdominal and pelvic abscesses (e.g., after surgery or trauma that allows fecal contamination of these tissues), brain abscesses (e.g., from bacteremia or spread from a middle ear or sinus infection), and bacteremia, which may spread the bacteria throughout the body.
Escherichia coli
E. coli inhabit the intestinal tract of humans. They are normally nonpathogenic in the intestinal tract where they serve a beneficial role by synthesizing vitamins and by competitively discouraging growth of potential pathogens. In other parts of the body, however, they act as pathogens.
E. coli cause most urinary tract infections. They also cause pneumonia and sepsis in immunocompromised hosts and meningitis and sepsis in newborns. E. coli pneumonia often occurs in debilitated patients after colonization of the oropharynx. In healthy people, the normal gram-positive bacteria of oral cavities attach to material that coats the surface of oral mucosa and prevents transient E. coli from establishing residence. Debilitated or severely ill people produce an enzyme that destroys the material that allows gram-positive flora to adhere to oral mucosa. This allows E. coli (and other gram-negative enteric bacteria) to compete successfully with the normal gram-positive flora and colonize the oropharynx. Then, droplets of the oral flora are aspirated into the respiratory tract, where impaired protective mechanisms allow survival of the aspirated bacteria.
E. coli also cause enteric gram-negative sepsis, which is acquired from the normal enteric bacterial flora. When E. coli and other gram-negative bacteria reach the bloodstream of healthy people, host defenses eliminate the organisms; however, when the organisms reach the bloodstream of people with severe illnesses or immunocompromised status, the host is unable to mount adequate defenses and sepsis occurs. In newborns, E. coli are the most common gram-negative bacteria causing nosocomial septic shock and meningitis.
E. coli often cause diarrhea and dysentery. One strain, called O157:H7, causes hemorrhagic colitis, a disease characterized by severe abdominal cramps, copious bloody diarrhea, and hemolytic-uremic syndrome (hemolytic anemia, thrombocytopenia, and acute renal failure). Hemolytic-uremic syndrome occurs most often in children. The main reservoir of this strain is the intestinal tract of animals, especially cattle, and several epidemics have been associated with ingestion of undercooked ground beef. Other sources include contaminated water and milk and person-to-person spread.
Klebsiella
Klebsiella bacteria, which are normal bowel flora, may infect the respiratory tract, urinary tract, bloodstream, burn wounds, and meninges, most often as opportunistic infections in debilitated persons. Klebsiella pneumoniae are a common cause of pneumonia, especially in people with pulmonary disease, bacteremia, and sepsis.
Proteus
Proteus bacteria are normally found in the intestinal tract and in decaying matter. They most often cause urinary tract and wound infections but may infect any tissue, especially in debilitated people. Infection often occurs with antibiotic therapy, which decreases drug-sensitive bacteria and allows drug-resistant Proteus bacteria to proliferate.
Pseudomonas
Pseudomonas bacteria are found in water, soil, skin, and intestines. They are found in the stools of some healthy people and possibly 50% of inpatients. Pseudomonas aeruginosa, the species most often associated with human disease, can cause infections of the respiratory tract, urinary tract, wounds, burns, meninges, eyes, and ears. Because of its resistance to many antibiotics, it can cause severe infections in people receiving antibiotic therapy for burns, wounds, and cystic fibrosis. P. aeruginosa colonizes the respiratory tract of most patients with cystic fibrosis and infects approximately 25% of burn patients. Infection is more likely to occur in hosts who are very young or very old or who have an impaired immune system. Sources of infection include catheterization of the urinary tract, trauma or procedures involving the brain or spinal cord, and contamination of respiratory ventilators.
Serratia
Serratia marcescens bacteria are found in infected people, water, milk, feces, and soil. They cause serious nosocomial infections of the urinary tract, respiratory tract, skin, burn wounds, and bloodstream. They also may cause hospital epidemics and produce drug-resistant strains. High-risk patients include newborns, the debilitated, and the immunosuppressed.
Salmonella
Approximately 1400 Salmonella species have been identified; several are pathogenic to humans. The bacteria cause gastroenteritis, typhoid fever, septicemia, and a severe, sometimes fatal type of food poisoning. The primary reservoir is the intestinal tract of many animals. Humans become infected through ingestion of contaminated water or food. Water becomes polluted by introduction of feces from any animal excreting salmonellae. Infection via food usually results from ingestion of contaminated meat or by hands transferring organisms from an infected source. In the United States, undercooked poultry and eggs are common sources.
Salmonella enterocolitis is a common cause of food- borne outbreaks of gastroenteritis. Diarrhea usually begins several hours after ingesting contaminated food and may continue for several days, along with nausea, vomiting, headache, and abdominal pain.
Shigella
Shigella species cause gastrointestinal problems ranging from mild diarrhea to severe bacillary dysentery. Humans, who seem to be the only natural hosts, become infected after ingestion of contaminated food or water. Effects of shigellosis are attributed to loss of fluids, electrolytes, and nutrients and to the ulceration that occurs in the colon wall.



