Chapter 19 Inflammation and the Immune Response
1. Describe the concept of self-tolerance.
2. Explain the differences between inflammation and immunity in terms of cells, functions, and features.
3. Use knowledge of physiology to describe the basis for the five cardinal manifestations of inflammation.
4. Discuss the influences of the aging process on inflammation and immunity and how these changes increase health risks for older adults.
5. Interpret a white blood cell count with differential to indicate no immune problems, immune suppression, infection, or an allergic reaction.
6. Differentiate the protection provided by active immunity, passive immunity, and cell-mediated immunity.
7. Describe the expected immune system responses to the presence of transplanted organs and the need for drug therapy to prevent transplant rejection.
http://evolve.elsevier.com/Iggy/
Animation: Function of B Cells
Animation: Function of T Cytotoxic Cells
Animation: Inflammatory Response
Review Questions for the NCLEX® Examination
Immune function is reduced by many diseases, injuries, and medical therapies. Reduction of immune function may be temporary or permanent, but it always endangers the patient’s health. Chapter 21 discusses issues related to reduced protection from inadequate immunity or inflammatory responses. Other problems occur when immunity overfunctions or functions at inappropriate times, at which time this normally protective response becomes an enemy (Braun, 2010; Stevens, 2009). Chapters 20 and 22 discuss issues related to damage from excess or inappropriate inflammatory or immune responses.
Overview
Self Versus Non-Self
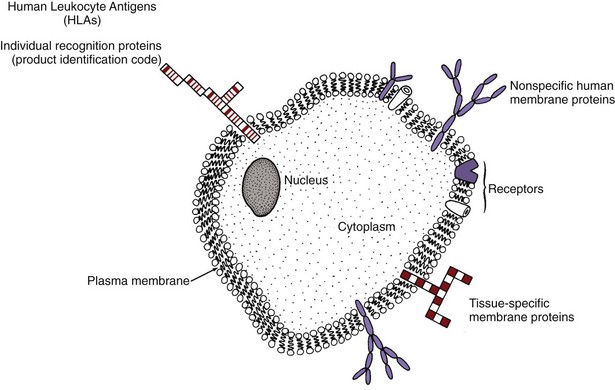
Each cell is surrounded by a plasma membrane with different proteins protruding through the surface (Fig. 19-1). For example, in liver cells, many different protein types are present on the cell membrane surface. The amino acid sequence of each protein type differs from that of all other protein types. Some of these proteins are found on the liver cells of all animals (including humans) that have livers, because these protein types are specific to the liver and serve as a marker for liver tissues. Other protein types are found only on the liver cells of humans, because these protein types are specific markers for human tissues. In addition, each person’s liver cells have surface proteins that are specific to that person. These unique proteins would be identical only to the proteins of an identical sibling. These unique proteins, known as human leukocyte antigens (HLAs), are found on the surface of all body cells of that person and serve as a “universal product code” or a “cellular fingerprint” for that person. One person’s HLAs are recognized as “foreign,” or non-self, by the immune system of another person. Because the cell-surface proteins are non-self to another person’s immune system, they are antigens, which are proteins capable of stimulating an immune response.
Humans have about 40 major HLAs that are determined by a set of genes called the major histocompatibility complex (MHC). The specific antigens that any person has (of a large number of possible antigens) are determined by which MHC gene alleles were inherited from his or her parents (Nussbaum et al., 2007).
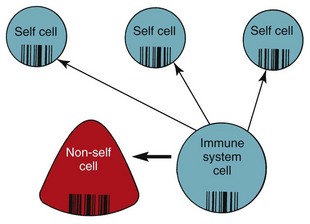
The HLAs are key for recognition and self-tolerance. The immune system cells constantly come into contact with other body cells and with any invader that enters the body. At each encounter, the immune system cells compare the surface protein HLAs to determine whether the encountered cell belongs in the body (Fig. 19-2). If the encountered cell’s HLAs perfectly match the HLAs of the immune system cell, the encountered cell is “self” and is not attacked by the immune system cell. If the encountered cell’s HLAs do not perfectly match the HLAs of the immune system cell, the encountered cell is non-self, or foreign. The immune system cell then takes action to neutralize, destroy, or eliminate this foreign invader.
Immune function changes during a person’s life, according to nutritional status, environmental conditions, drugs, disease, and age. Immune function is most efficient when people are in their 20s and 30s and slowly declines with increasing age (Graham et al., 2006; Touhy & Jett, 2010). Older adults have decreased immune function, increasing their risk for many health problems (Chart 19-1).
Chart 19-1 Nursing Focus on the Older Adult
Changes in Immune Function Related to Aging
| IMMUNE COMPONENT | FUNCTIONAL CHANGE | NURSING IMPLICATIONS |
|---|---|---|
| Inflammation | There is a probable defect in neutrophil function. | Neutrophil counts may be normal, but activity is reduced or impaired, increasing the risk for infection. |
| Leukocytosis does not occur during episodes of acute infection. | Patients may have an infection but not show expected changes in white blood cell counts. | |
| Older adults may not have a fever during inflammatory or infectious episodes. | Not only is there potential loss of protection through inflammation, but also minor infections may be overlooked until the patient becomes severely infected or septic. | |
| Antibody-mediated immunity | The total number of colony-forming B-lymphocytes and the ability of these cells to mature into antibody-secreting cells are diminished. | Older adults are less able to make new antibodies in response to the presence of new antigens. Thus they should receive immunizations, such as “flu shots,” the pneumococcal vaccination, and the shingles vaccination. |
| There is a decline in natural antibodies, decreased response to antigens, and reduction in the amount of time the antibody response is maintained. | Older adults may not have sufficient antibodies present to provide protection when they are re-exposed to microorganisms against which they have already generated antibodies. Thus older patients need to avoid people with viral infections and need to receive “booster” shots for old vaccinations and immunizations, especially tetanus and pertussis (whooping cough). | |
| Cell-mediated immunity | Thymic activity decreases with aging, and the number of circulating T-lymphocytes decreases. | Skin tests for tuberculosis may be falsely negative. Older patients are more at risk for bacterial and fungal infections, especially on the skin and mucous membranes, in the respiratory tract, and in the genitourinary tract. |
Organization of the Immune System
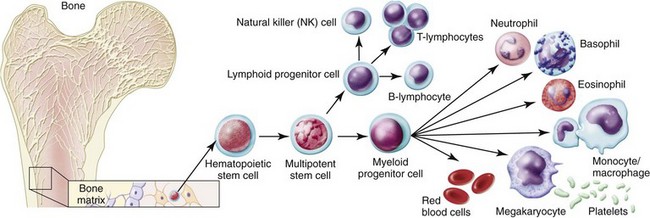
The bone marrow is the source of all blood cells, including immune system cells. The bone marrow produces immature, undifferentiated cells called stem cells (Abbas et al., 2010, Kaufman, 2011). Stem cells are pluripotent, meaning that each cell has more than one potential outcome. When the stem cell is first created in the bone marrow, it is undifferentiated. The cell is not yet committed to maturing into a specific blood cell type. At this stage, the stem cell is flexible (pluripotent) and could become any one of many mature blood cells. Fig. 19-3 shows the possible outcomes for maturation of stem cells. The type of mature cell that the stem cell becomes depends on which pathway it follows.
White blood cells (leukocytes or WBCs) protect the body from the effects of invasion by organisms. These cells are the immune system cells—the knight and soldiers protecting the castle inhabitants after invaders get through the castle wall. Table 19-1 lists the functions of different immune system cells. The leukocytes provide protection through many defensive actions (Abbas et al., 2010; Stevens, 2009). These actions include:
• Recognition of self versus non-self
• Destruction of foreign invaders, cellular debris, and unhealthy or abnormal self cells
• Production of antibodies directed against invaders
• Production of cytokines that stimulate increased formation of leukocytes in bone marrow and increase specific leukocyte activity
TABLE 19-1 IMMUNE FUNCTIONS OF SPECIFIC LEUKOCYTES
| VARIABLE | LEUKOCYTE | FUNCTION |
|---|---|---|
| Inflammation | Neutrophil | Nonspecific ingestion and phagocytosis of microorganisms and foreign protein |
| Macrophage | Nonspecific recognition of foreign proteins and microorganisms; ingestion and phagocytosis | |
| Monocyte | Destruction of bacteria and cellular debris; matures into macrophage | |
| Eosinophil | Weak phagocytic action; releases vasoactive amines during allergic reactions | |
| Basophil | Releases histamine and heparin in areas of tissue damage | |
| Antibody-mediated immunity | B-lymphocyte | Becomes sensitized to foreign cells and proteins |
| Plasma cell | Secretes immunoglobulins in response to the presence of a specific antigen | |
| Memory cell | Remains sensitized to a specific antigen and can secrete increased amounts of immunoglobulins specific to the antigen on re-exposure | |
| Cell-mediated immunity | Helper/inducer T-cell | Enhances immune activity through secretion of various factors, cytokines, and lymphokines |
| Cytotoxic/cytolytic T-cell | Selectively attacks and destroys non-self cells, including virally infected cells, grafts, and transplanted organs | |
| Natural killer cell | Nonselectively attacks non-self cells, especially body cells that have undergone mutation and become malignant; also attacks grafts and transplanted organs |
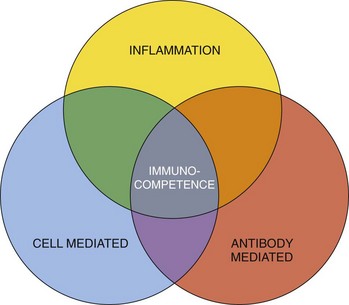
The three processes needed for human protection through immunity are (1) inflammation, (2) antibody-mediated immunity (AMI), and (3) cell-mediated immunity (CMI). Each process uses different defensive actions, and each influences or requires assistance from the other two processes (Fig. 19-4). Therefore full immunity (immunocompetence) requires the function and interaction of all three processes.
Inflammation
The inflammatory responses are part of innate immunity. Other parts of innate immunity include skin, mucosa, antimicrobial chemicals on the skin, complement, and natural killer cells (Abbas et al., 2010; Stevens, 2009).
• Inflammatory protection is immediate but short-term against injury or invading organisms. It does not provide true immunity on repeated exposure to the same organisms.
• Inflammation is a nonspecific body defense to invasion or injury and can be started quickly by almost any event, regardless of where it occurs or what causes it.
Inflammatory responses start tissue actions that cause visible and uncomfortable symptoms. Despite the discomfort, these actions are important in ridding the body of harmful organisms. However, if the inflammatory response is excessive, tissue damage may result (Landis, 2009). Inflammatory responses also help start both antibody-mediated and cell-mediated actions to activate a full immune response.
Cell Types Involved in Inflammation
Neutrophils
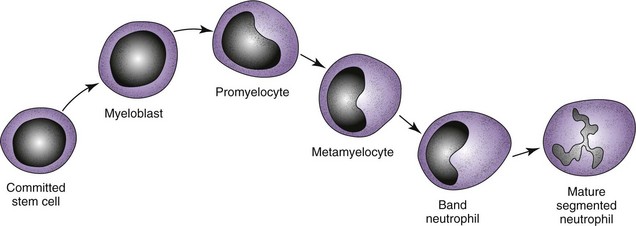
Mature neutrophils make up between 55% and 70% of the normal total white blood cell (WBC) count. Neutrophils come from the stem cells and complete the maturation process in the bone marrow (Fig. 19-5). They are also called granulocytes because of the large number of granules present inside each cell. Other names for neutrophils are based on their appearance and maturity. Mature neutrophils are also called segmented neutrophils (“segs”) or polymorphonuclear cells (“polys,” PMNs) because of their segmented nucleus. Less mature neutrophils are called band neutrophils (“bands” or “stabs”) because of their nuclear shape.
In the immunocompetent healthy person, more than 100 billion fresh, mature neutrophils are released from the bone marrow into the circulation daily (Abbas et al., 2010; Stevens, 2009). This huge production is needed because the life span of each neutrophil is short—about 12 to 18 hours.
The differential of a normal white blood cell count shows the number and percent of the different types of circulating leukocytes (Table 19-2). Usually, most neutrophils released into the blood from the bone marrow are segmented neutrophils; only a small percentage are band neutrophils. Less mature neutrophil forms should not be in the blood. Some problems, such as sepsis, cause the neutrophils in the blood to change from being mostly segmented neutrophils to being less mature forms. This situation is termed a left shift or bandemia because the segmented neutrophil, which is seen at the far right of the neutrophil pathway (see Fig. 19-5), is no longer the most numerous type of circulating neutrophils. Instead, more of the circulating cells are bands—the less mature cell type found farther left on the neutrophil pathway.
TABLE 19-2 VALUES OF A WHITE BLOOD CELL DIFFERENTIAL FOR PERIPHERAL BLOOD REPRESENTING A NORMAL COUNT
| WBC TYPE | % | /MM3 |
|---|---|---|
| TOTAL WBC | 100 | 10,000 |
| Segs | 62 | 6200 |
| Bands | 5 | 500 |
| Monos | 3 | 300 |
| Lymphs | 28 | 2800 |
| Eosins | 1.5 | 150 |
| Basos | 0.5 | 50 |
Macrophages
Macrophages come from the committed myeloid stem cells in the bone marrow and form the mononuclear-phagocyte system. The stem cells first form monocytes, which are released into the blood at this stage. Until they mature, monocytes have limited activity. Most monocytes move from the blood into body tissues, where they mature into macrophages. Some macrophages become “fixed” in position within the tissues, whereas others can move within and between tissues. Macrophages in various tissues have slightly different appearances and names (Table 19-3). The liver, spleen, and intestinal tract contain large numbers of these cells.
| TISSUE | MACROPHAGE |
|---|---|
| Lung | Alveolar macrophage |
| Connective tissue | Histiocyte |
| Brain | Microglial cell |
| Liver | Kupffer cell |
| Peritoneum | Peritoneal macrophage |
| Bone | Osteoclast |
| Joint | Synovial type A cell |
| Kidney | Mesangial cell |
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree