1. Define, spell, and pronounce the terms listed in the vocabulary. 2. Apply critical thinking skills in performing patient assessment and care. 3. Describe the characteristics of pathogenic microorganisms and the diseases they cause. 4. Apply the chain-of-infection process to healthcare practice. 5. Compare viral and bacterial cell invasion. 6. Differentiate between humoral and cell-mediated immunity. 8. Analyze the differences among acute, chronic, latent, and opportunistic infections. 9. Specify potentially infectious body fluids. 11. Explain the major areas included in the OSHA Compliance Guidelines. 12. Remove contaminated gloves while following Standard Precautions principles. 13. Perform an eye wash procedure to remove contaminated material. 14. Summarize the management of postexposure evaluation and follow-up. 15. Participate in a mock environmental exposure event with documentation of the steps taken. 16. Apply the concepts of medical and surgical asepsis to the healthcare setting. 17. Demonstrate the proper hand-washing technique for medical asepsis. 18. Differentiate among sanitization, disinfection, and sterilization procedures. 19. Demonstrate the correct procedure for sanitizing contaminated instruments. 20. Apply patient education concepts to infection control. 21. Discuss the legal and ethical concerns regarding medical asepsis and infection control. anaphylaxis (an-uh-fuh-lak′-sis) An exaggerated hypersensitivity reaction that in severe cases leads to vascular collapse, bronchospasm, and shock. antibodies (an′-ti-bah-dees) Immunoglobulins produced by the immune system in response to bacteria, viruses, or other antigenic substances. antigen (an′-ti-juhn) A foreign substance that causes the production of a specific antibody. antiseptics (an-ti-sep-tik) Substances that inhibit the growth of microorganisms on living tissue (e.g., alcohol and povidone-iodine solution [Betadine]). autoimmune (o-to-im′-yuhn) Pertaining to a disturbance in the immune system in which the body reacts against its own tissue. Examples of autoimmune disorders include multiple sclerosis, rheumatoid arthritis, and systemic lupus erythematosus. candidiasis (kan-duh-de-uh′-sis) An infection caused by a yeast that typically affects the vaginal mucosa and skin. coagulate (ko-ag′-yuh-late) To form into clots. contaminated Soiled with pathogens or infectious material; nonsterile. disinfectant A liquid chemical that is capable of eliminating many or all pathogens but is not effective against bacterial spores. germicides (jur′-muh-sids) Agents that destroy pathogenic organisms. hereditary (huh-re′-duh-ter-e) Pertaining to a characteristic, condition, or disease transmitted from parent to offspring on the DNA chain. interferon (in′-tuhr-fir-on) A protein formed when a cell is exposed to a virus; the protein blocks viral action on the cell and protects against viral invasion. opportunistic infections Infections caused by a normally nonpathogenic organism in a host whose resistance has been decreased. palliative A substance that relieves or alleviates the symptoms of a disease without curing the disease. parenteral (puh-ren′-tuh-ruhl) The injection or introduction of substances into the body by any route other than the digestive tract (e.g., subcutaneous, intravenous, or intramuscular administration). pathogenic (path′-o-jen-ik) Pertaining to a disease-causing microorganism. permeable (pur′-me-uh-buhl) Allowing a substance to pass or soak through. pyemia (pi-em′-e-uh) The presence of pus-forming organisms in the blood. relapse The recurrence of the symptoms of a disease after apparent recovery. resident bacteria Bacteria that live in or on a certain part of the body, such as the skin or mucosa. rhinitis (rin-i′-tis) Inflammation of the mucous membranes of the nose. spores A thick-walled, dormant form of bacteria that is very resistant to disinfection measures. sterile (ster′-il) Free of all microorganisms, pathogenic and nonpathogenic. tinea (tin′-e-uh) Any fungal skin disease that results in scaling, itching, and inflammation. transient bacteria Bacteria temporarily living in or on a certain body part, such as the hands. urticaria (uhr-tuh-kar′-e-uh) A skin eruption that creates inflamed wheals; hives. vectors Animals or insects (e.g., ticks) that transmit the causative organisms of disease. Rosa Lucia is a certified medical assistant working in a multiphysician pediatric practice. She is quite concerned about contracting an infectious disease while caring for her patients. Rosa learned about Standard Precautions while enrolled in her medical assisting program and now must implement that knowledge in the workplace. Two important factors in preventing the spread of infection are understanding how to break the chain of infection and recognizing the importance of correct and frequent hand washing. While studying this chapter, think about the following questions: The concepts of disease transmission and the body’s response to infection form the basis for understanding the importance of the first line of defense in preventing disease. Before we can assist in the prevention of disease, we have to look at methods we can use to minimize the chances of being a carrier of disease. One of the simplest ways to prevent the spread of disease is to wash your hands or use alcohol-based hand rubs. As you continue through the remainder of this textbook, you should refer to the fundamental concepts of this chapter when faced with an infection control issue. Because of the need for infection control and the impact on medical practice of the guidelines established by the Occupational Safety and Health Administration (OSHA), every procedure must begin and end with hand hygiene practices. The concepts in this chapter are basic to all clinical skills, and following them can reduce the transmission of disease organisms and lessen the severity of disease. They also may save a patient’s or co-worker’s life, or even your own. Disease is defined as any sustained, harmful alteration of the normal structure, function, or metabolism of an organism or cell. This pathologic condition of the body presents a group of clinical signs, symptoms, and laboratory findings that set it apart as an abnormal entity, different from other normal and pathologic conditions. We recognize and categorize many types of diseases: hereditary (genetic), drug-induced, autoimmune, degenerative, communicable, and infectious, to name only a few. Sometimes a specific disease may fit two or more categories. Any disease caused by the growth of pathogenic microorganisms in the body falls into the category of infectious diseases. The entrance of a living microbe into the body is not disease, because until the infected cell or individual shows a harmful alteration in structure, physiology, or biochemistry, disease either is not detected or is not considered present. In fact, a pathogen may be ingested, injected, or inhaled and never cause disease. However, an unaffected person still can transmit the infection to another person. In this case we call the unaffected person a carrier. Microorganisms are almost everywhere. We carry them on our skin, in our bodies, and on our clothing. They can be in ice, boiling water, the soil, and the air. The only places free of microorganisms are certain internal body organs and tissues and sterilized medical equipment and supplies. In the normal state, organs and tissues that do not connect with the outside by means of mucus-lined membranes are free of all living microorganisms. Certain factors are required for an infectious disease to spread. These factors, or links, make up the chain of infection. Break the chain, and you break the infectious process (Figure 27-1). The chain of infection starts with the infectious agent. Five groups make up the potentially pathogenic agents or microorganisms: viruses, bacteria, protozoa, fungi, and rickettsiae. (Additional information about typical diseases caused by these pathogens is presented in Chapter 55.) Infection cannot occur without the presence of an infectious microorganism, so the best way for healthcare workers to prevent the spread of disease is to use adequate infection control procedures, such as consistent hand washing and proper use of antiseptics, in addition to effective disinfection and sterilization methods. The smallest of all pathogens, viruses, lead the list of important disease-causing agents. Viral microorganisms are intracellular parasites that take over the deoxyribonucleic acid (DNA) or ribonucleic acid (RNA) of the invaded cell. Viral invasion may not cause significant immediate symptoms, because host cells infected with viruses can produce a substance called interferon, which protects nearby cells. Interferon leaves the infected cell and acts somewhat like a Paul Revere, warning neighboring cells that “a virus is coming!” The neighboring cells then produce antiviral proteins that may destroy the viruses once they enter. Antibiotics are unable to destroy viral invaders that enter a normal cell and multiply within the cell. The only way to destroy a viral invader is to destroy the host cell. Therefore, the treatment for viral infections typically focuses on relieving symptoms, or palliative treatment. To counteract and slow the rate of viral replication, interferon and the antiviral agents acyclovir (Zovirax), valacyclovir hydrochloride (Valtrex), adefovir dipivoxil (Adefovir), penciclovir (Denavir), and famciclovir (Famvir) may be prescribed, depending on the specific viral agent. Viral diseases include the common cold, influenza, herpes, infectious hepatitis, and acquired immunodeficiency syndrome (AIDS), which is caused by the human immunodeficiency virus (HIV). Bacteria are tiny, simple cells that produce disease in a variety of ways. Pathogenic bacteria can secrete toxic substances that damage human tissues, act as parasites inside human cells, or grow on body surfaces, disrupting normal human functions. Bacteria are classified according to their shape, or morphology; they may be spherical (cocci), rod shaped (bacilli), or spiral shaped (spirilla) (see Chapter 55). Some bacteria can produce resistant internal structures, called spores, that make treatment difficult. When bacteria invade the body, the patient can be treated in a number of ways. The most common approach is to use antibiotics to destroy the invader or inhibit its growth. We all have nonpathogenic bacteria that reside in various body systems; for example, a harmless form of Escherichia coli (E. coli) lives in the large intestine. These bacteria protect against disease by competing for nutrients that pathogenic bacteria require to grow and multiply. Common diseases caused by bacteria include tuberculosis, urinary tract infections, pneumonia, and strep throat. Protozoa are unicellular parasites that can replicate and multiply rapidly once inside the host. Examples of diseases caused by protozoa include giardiasis, which typically is caused by the ingestion of water contaminated by feces, and malaria, in which Plasmodium organisms invade the blood system. Protozoal infections frequently are seen in tropical climates, which have large insect populations. These insects serve as vectors for many protozoal diseases. For example, the mosquito transmits the organisms that cause malaria. Fungi may be unicellular or multicellular; they include such organisms as mushrooms, molds, and yeasts. Many forms are pathogenic and can cause disease, such as candidiasis and tinea infections. Fungi grow best in warm, moist environments. Treatment with antifungal agents includes application of topical preparations (e.g., Lotrimin) for tinea infections; vaginal suppositories (e.g., Monistat) for candidiasis; and oral medications, such as fluconazole (Diflucan), ketoconazole (Nizoral), and terbinafine (Lamisil). Fungal infections also are called mycotic infections. Rickettsiae are microorganisms that have characteristics of both bacteria and viruses. Like viruses, they are obligate parasites that must live within a host cell for growth; however, they are larger than viruses, so they can be viewed with a microscope. Vectors such as fleas, ticks, and mites usually transmit pathogenic forms of rickettsiae. Diseases caused by rickettsiae can be treated with antibiotics; they include Rocky Mountain spotted fever, which is transmitted by a tick. The second link in the chain of infection is the reservoir. Reservoirs may be people, insects, animals, water, food, or contaminated instruments. Most pathogens must gain entrance into a host or else they will die. The reservoir host supplies nutrition for the organism, allowing it to multiply. The pathogen either causes infection in the host or, in the case of vector-borne diseases, exits the host in great enough numbers to cause disease in another host. The chain of infection continues with the means, or portal, of exit; that is, how the pathogen escapes the reservoir host. Exits include the mouth, nose, eyes, ears, intestines, urinary tract, reproductive tract, and open wounds. The use of Standard Precautions (e.g., latex gloves, masks, proper wound care, correct disposal of contaminated products, hand washing) helps control the ability of infectious material to spread from one host to another. After exiting the reservoir host, organisms spread by transmission. Transmission either is direct or indirect. Direct transmission occurs from contact with an infected person or with discharges from an infected person, such as feces or urine. Indirect transmission occurs from droplets in the air expelled by coughing, speaking, or sneezing; vectors that harbor pathogens; contaminated food or drink; and/or contact with contaminated objects (called fomites). Proper sanitation of water and food; the use of sanitization, disinfection, and sterilization procedures; and the use of germicides, such as Wavicide and Cidex, help control the transmission of pathogens. The next step in the chain of infection is the means, or portal, of entry. This is how the transmitted pathogen gains entry into a new host. Like the means of exit, the means of entry may be the mouth, nose, eyes, intestines, urinary tract, reproductive system, or an open wound. The first line of defense against pathogenic invasion is the intact integumentary system, or skin, which serves as a mechanical barrier to infection. Anatomic defense mechanisms also include tears, cilia, mucous membranes, and the pH of body fluids. The body’s second line of defense includes the inflammatory process and immune system response. The immune system responds by producing antibodies specifically designed to combat the presence of a foreign substance, or antigen. This process is called humoral immunity and is the responsibility of the body’s B cells. The immune system also reacts at the cellular level with T-cell activity in cell-mediated immunity by causing the destruction of pathogenic cells at the site of invasion. An example of cell-mediated immunity is phagocytosis, in which specialized immune system cells called macrophages actually ingest and destroy pathogenic microbes (see Chapter 54). If the host is susceptible (i.e., capable of supporting the growth of the infecting organism), the organism multiplies. Factors that affect a host’s susceptibility include the location of entry, the dose of organisms, and the individual’s state of health. If conditions are right, the organism reaches infectious levels, and the susceptible host can start the chain of infection all over. Individuals who are effectively immunized against a disease, such as hepatitis B, are not susceptible to the disease even if they are exposed to the pathogen, because their immune system has created antibodies to protect them. In addition to immunization, other ways to reduce susceptibility to disease organisms are proper nutrition and a healthy lifestyle. When trauma occurs to the body or it is exposed to pathogens, protective mechanisms are alerted, and the body responds in a predictable manner, called the inflammatory response (Figure 27-2). To defend itself, the body initiates specific responses to destroy and remove pathogenic organisms and their byproducts; or, if this is not possible, to limit the extent of damage caused by the invading pathogen. This process results in the four classic symptoms of inflammation: erythema (redness), edema (swelling), pain, and heat. When the body is exposed to an infectious agent or a foreign substance, cellular damage occurs at the site. Inflammation mediators (i.e., histamine, prostaglandins, and kinins) are released and cause three different responses at the cellular level. All three actions are designed to increase the number of white blood cells (WBCs) at the injury site. First, blood vessels at the site dilate, causing an increase in local blood flow, which results in redness (inflammation) and heat. Blood vessel walls become more permeable, which assists in the release of WBCs to the site. The WBCs begin to form a fibrous capsule around the site to protect surrounding cells from damage or infection. Blood plasma also filters out of the more permeable vessel walls, resulting in edema, which puts pressure on the nerves and causes pain. Finally, chemotaxis, or the release of chemical agents, occurs, attracting even more WBCs to the site. The increased number of WBCs at the site results in phagocytosis, or the engulfing and destruction of microorganisms and damaged cells. Destroyed pathogens, cells, and WBCs collect in the area and form a thick, white substance called pus. If the pathogenic invasion is too great for localized control, the infection may collect in the body’s lymph nodes, where more WBCs are present to help fight the battle. This causes swollen glands, or lymphadenopathy. If the body is too weak or the number of pathogens is too great, the infection may spread to the bloodstream. A systemic infection, called septicemia or blood poisoning, may occur that ultimately could affect the entire body. Another term for septicemia is pyemia. Without appropriate medical intervention, death can occur. An acute infection has a rapid onset of symptoms but lasts a relatively short time. The prodromal period is that time when the patient first shows vague, nonspecific symptoms of disease. In an acute viral infection, the host cell typically dies within hours or days. Symptoms appear after the tissue damage begins. In most acute infections, such as the common cold, the body’s defense mechanisms eliminate the virus within 2 to 3 weeks. An infection that persists for a long period, sometimes for life, is called a chronic infection. In the case of chronic viral hepatitis B, patients are asymptomatic, or without symptoms, but the virus is detectable with blood tests and remains transmissible throughout the person’s life. Hepatitis B, or serum hepatitis, is transmitted by blood or blood products and by all body fluids. It is a serious health hazard to medical personnel. All individuals employed in a healthcare setting should be immunized against hepatitis B. A latent infection is a persistent infection in which the symptoms cycle through periods of relapse and remission. Cold sores and genital herpes are latent viral infections caused by the herpes simplex virus (HSV) types I and II, respectively. The virus enters the body and causes the original lesion. It then lies dormant, in nerve cells away from the surface, until a certain provocation (illness with fever, sunburn, or stress) causes it to leave the nerve cell and seek the surface again. Once the virus reaches the superficial tissues, it becomes detectable for a short time and causes a new outbreak at the site. Another herpes virus, varicella-zoster virus, causes chickenpox (varicella). This virus may lie dormant along a nerve pathway for years and later erupt as the painful disease shingles (zoster). Opportunistic infections are caused by organisms that are not typically pathogenic but that occur in hosts with an impaired immune system response, such as individuals infected with HIV. Over time, the person’s immune system becomes weakened, and diseases result that are not typically seen in patients with a healthy immune system, such as certain types of pneumonia and oral candidiasis. Chapter 7 introduced the role of OSHA in protecting patients and healthcare personnel from potentially harmful substances in the medical facility. In 1987, in response to concern about the increasing prevalence of HIV and the hepatitis B virus (HBV), the Centers for Disease Control (now the CDC) recommended a new approach to potentially infectious materials called Universal Precautions. The underlying concept of Universal Precautions is that because healthcare workers cannot know whether a patient has an infectious disorder, all blood and certain body fluids must be treated as if known to be infectious for blood-borne pathogens. Therefore, precautions must be implemented for all patients, regardless of the information available about the person’s individual health history. In turn, Universal Precautions protect patients from any blood-borne infection the healthcare worker may carry. OSHA recognizes that healthcare employees face significant health risks as the result of occupational exposure to blood or other potentially infectious materials that may contain HBV, the hepatitis C virus (HCV), or HIV. In July 1992, OSHA began enforcing work practice controls to reduce or eliminate occupational exposure to blood-borne pathogens. Employers whose workers are at risk for occupational exposure to blood or other infectious materials must implement an Exposure Control Plan that details employee protection procedures. The Exposure Control Plan must identify job classifications and/or specific work-related tasks in which an employee potentially may be exposed to blood and/or body fluids. The plan must describe how an employer will use a combination of controls, including personal protective equipment (PPE), training, medical surveillance, hepatitis B immunizations, record keeping of occupational injuries, postexposure follow-up, and labeling of hazardous materials. Engineering controls, such as safer medical equipment, puncture-proof sharps containers, and shielded needle devices, in addition to PPE (e.g., gloves, gowns, and face shields), are recommended as the primary ways to reduce or eliminate employee exposure. The plan must be reviewed and updated at least annually to incorporate the use of safer medical devices designed to eliminate or minimize occupational exposure to contaminated waste. In addition, the Exposure Control Plan must be readily available to all employees for review and training. It does not have to be a separate document and may be included as part of the facility’s procedures manual or in the health and safety manual developed by the site.
Infection Control
Learning Objectives
Vocabulary
Scenario
Disease
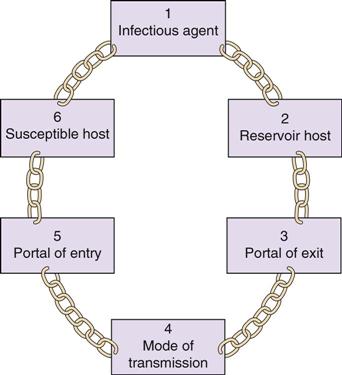
The Chain of Infection
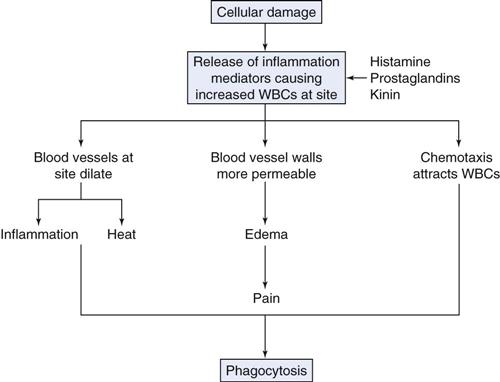
The Inflammatory Response
Types of Infections
Acute Infection
Chronic Infection
Latent Infection
Opportunistic Infections
Osha Standards for the Healthcare Setting
Exposure Control Plan
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Infection Control
Get Clinical Tree app for offline access
