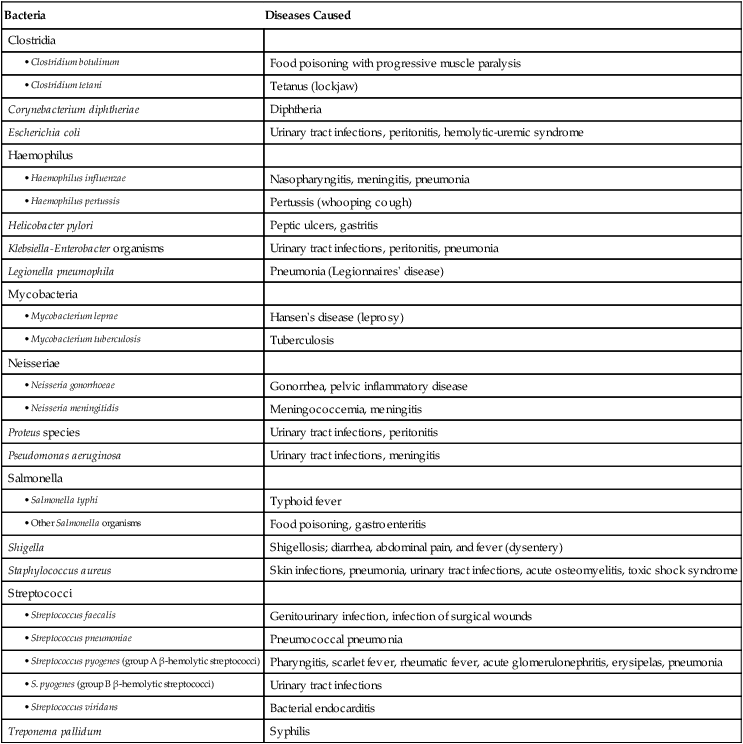
Jeffrey Kwong and Lucy Bradley-Springer 1. Evaluate the impact of emerging and reemerging infections on health care. 2. Identify ways to decrease the development of resistance to antibiotics. 3. Explain the ways human immunodeficiency virus (HIV) is transmitted and the factors that affect transmission. 4. Describe the pathophysiology of HIV infection. 5. Chart the spectrum of untreated HIV infection. 6. Identify the diagnostic criteria for acquired immunodeficiency syndrome (AIDS). 7. Describe methods used to test for HIV infection. 8. Discuss the collaborative management of HIV infection. 9. Summarize the characteristics of opportunistic diseases associated with AIDS. 10. Describe the potential complications associated with long-term treatment of HIV infection. 11. Compare and contrast HIV prevention methods. 12. Describe the nursing management of HIV-infected patients and HIV-at-risk patients. Infections, such as lower respiratory tract infections, malaria, HIV, and tuberculosis (TB), are responsible for a significant number of deaths worldwide.1 Infection occurs when a pathogen (a microorganism that causes disease) invades the body, begins to multiply, and produces disease, usually causing harm to the host. The signs and symptoms of infection are a result of specific pathogen activity, which triggers inflammation and other immune responses.2 eTABLE 15-1 CENTERS FOR DISEASE CONTROL AND PREVENTION (CDC) GUIDELINES FOR ISOLATION PRECAUTIONS eTABLE 15-2 TREATMENT OF COMMON OPPORTUNISTIC DISEASES ASSOCIATED WITH HIV INFECTION *If available. In most cases, effective antiretroviral therapy is the best prevention for all opportunistic diseases. †In most cases, adequate antiretroviral therapy is the best treatment for all opportunistic diseases. Sources: Centers for Disease Control and Prevention (CDC): Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents—April 10, 2009. Available at http://aidsinfo.nih.gov. eTABLE 15-3 DRUG THERAPY *Many of these drugs cause serious and potentially fatal interactions when used in combination with other commonly used drugs, some of which are available over the counter. Sources: Centers for Disease Control and Prevention (CDC): Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents, 2012. Available at aidsinfo.nih.gov. eTABLE 15-4 PATIENT TEACHING GUIDE eTABLE 15-5 PATIENT TEACHING GUIDE eTABLE 15-6 PATIENT TEACHING GUIDE eTABLE 15-7 NURSING INTERVENTIONS IN HIV INFECTION • Teach regarding HIV, the spectrum of infection, options for care, signs and symptoms to report, treatment options, immune enhancement, risk reduction, and ways to adhere to treatment regimens. • Establish long-term, trusting relationship with patient, family, and significant others. • Provide emotional and spiritual support. • Develop resources for legal needs: discrimination prevention, wills and powers of attorney, child care wishes. • Empower the patient to identify needs, direct care, and seek services. • Provide care during acute exacerbations: recognition of life-threatening developments, life support, rapid intervention with treatments and drugs, comfort, and hygiene needs. • Support patient and family during crisis. • Assist the patient with mental health issues and provide referral to mental health specialist as needed. • Continue physical care for chronic disease process: treatments, drugs, comfort, and hygiene needs. • Encourage health promotion measures (as above). • Refer the patient to resources to support finances. • Support patient and family or significant others in a trusting relationship. • Assist with end-of-life issues: resuscitation orders, comfort measures, funeral plans, estate planning, child care continuation, etc. • Assess desires and refer to resources that will assist in meeting identified spiritual needs. The many different kinds of pathogens can be classified into several groups, including bacteria, viruses, fungi, protozoa, and prions.3 Bacteria are one-celled organisms that are common throughout nature. Many bacteria are normal flora. They live harmoniously in or on the human body without causing disease under normal circumstances. Normal flora protect the human body by preventing the overgrowth of other microorganisms. For example, Escherichia coli is a bacteria that is part of the normal flora in the large intestine. Bacteria cause disease in two ways: by entering the body and growing inside human cells (e.g., TB) or by secreting toxins that damage cells (e.g., Staphylococcus aureus). Bacteria are divided into categories based on the shape of their cells. Cocci, such as streptococci and staphylococci, are round. Bacilli are rod shaped and include tetanus and TB. Curved rods include Vibrio bacteria, one of which causes cholera. Spirochetes are spiral shaped and include the organisms that cause leprosy and syphilis. Table 15-1 lists common pathogenic bacteria and the diseases that they cause. TABLE 15-1 Viruses, unlike bacteria, do not have a cellular structure. They are simple infectious particles that consist of a small amount of genetic material (either ribonucleic acid [RNA] or deoxyribonucleic acid [DNA]) and a protein envelope. Viruses can reproduce only after releasing their genetic material into the cell of another living organism. Examples of diseases caused by viruses are shown in Table 15-2. TABLE 15-2 Fungi are organisms similar to plants, but they lack chlorophyll. Mycosis is any disease caused by a fungus. Pathogenic fungi cause infections that are usually localized but can become disseminated in an immunocompromised person. Tinea pedis (athlete’s foot) and tinea corporis (ringworm) are two common mycotic infections. Some fungi are normal flora in the body, but when overgrowth occurs, disease can result. Overgrowth of Candida albicans, for example, can cause candidiasis in the mouth (thrush), esophagus, intestines, and vagina. Other fungi and their respective mycotic infections are listed in Table 15-3. TABLE 15-3 *See Table 28-14: Fungal Infections of the Lung. †See Table 24-6: Common Fungal Infections of the Skin. Prions are infectious particles that contain abnormally shaped proteins. Not all prions cause disease, but those that do typically affect the nervous system. They can cause a group of illnesses called transmissible spongiform encephalopathies (TSEs). Some of the more common TSEs are Creutzfeldt-Jakob disease and bovine spongiform encephalopathy in cattle (also known as mad cow disease).4 An emerging infection is an infectious disease that has recently increased in incidence or that threatens to increase in the immediate future. Examples of emerging infections are described in Table 15-4. Emerging infectious diseases can originate from unknown sources or from contact with animals, changes in known diseases, or biologic warfare. For example, severe acute respiratory syndrome (SARS) and the West Nile virus come from animal sources. Others emerged when a previously treatable organism (e.g., S. aureus) developed resistance to antibiotics. TABLE 15-4 The battle against infection is not new, but modern technologies have changed the rules of the game. Global travel, population density, encroachment into new environments, misuse of antibiotics, and bioterrorism have increased the risk for widespread distribution of emerging infections.5 Not too long ago many believed that science had conquered infectious disease. However, newly recognized infectious diseases have emerged in recent decades. These include HIV, Lyme disease, hepatitis C, SARS, Ebola virus, and influenza A (H1N1) virus. Some diseases once thought to be under control, such as TB, measles, and pertussis, have reemerged.6 Studies in zoonosis (the science of transmission of diseases from animals to humans) have shown that many known infectious diseases come from animal and insect vectors. The SARS outbreak in China in 2003, for instance, was linked to the civet cat, a small carnivorous mammal found throughout much of Asia and Africa. (SARS is discussed in Chapter 68.) West Nile virus is carried and transmitted by mosquitoes. Mosquitoes acquire the virus as they draw blood from infected animals and people. The virus does not cause illness in the mosquito, but can be transferred to uninfected animals and humans as the mosquito continues to feed. Bird deaths are an early warning sign of a West Nile virus outbreak, which can spread quickly if action is not taken in a timely manner. (West Nile virus is discussed in Chapter 57.) Influenza viruses are examples of how disease can spread between animals and humans. Variants of influenza A viruses were responsible for influenza epidemics. These include the 2009 influenza A (H1N1) outbreak that was traced back to pigs, hence the name swine flu. In 1997 and 2003 outbreaks of the influenza A (H5N1) strain of avian flu resulted from transmission of influenza virus from chickens to humans.7 Ebola virus has presented an ongoing challenge to public health since it was first seen in 1976. Ebola virus causes severe hemorrhagic fever and is usually lethal. Therapeutic and preventive measures are extremely limited. The natural reservoir and path of transmission are unknown, which makes it impossible to effectively combat Ebola virus and the disease it causes.8 Vaccines and proper medications have led to the near eradication of some infections (e.g., smallpox and polio), but infective agents can reemerge if conditions are right. Table 15-5 presents some diseases that have shown resurgence in recent decades. TABLE 15-5
Infection and Human Immunodeficiency Virus Infection
Infections
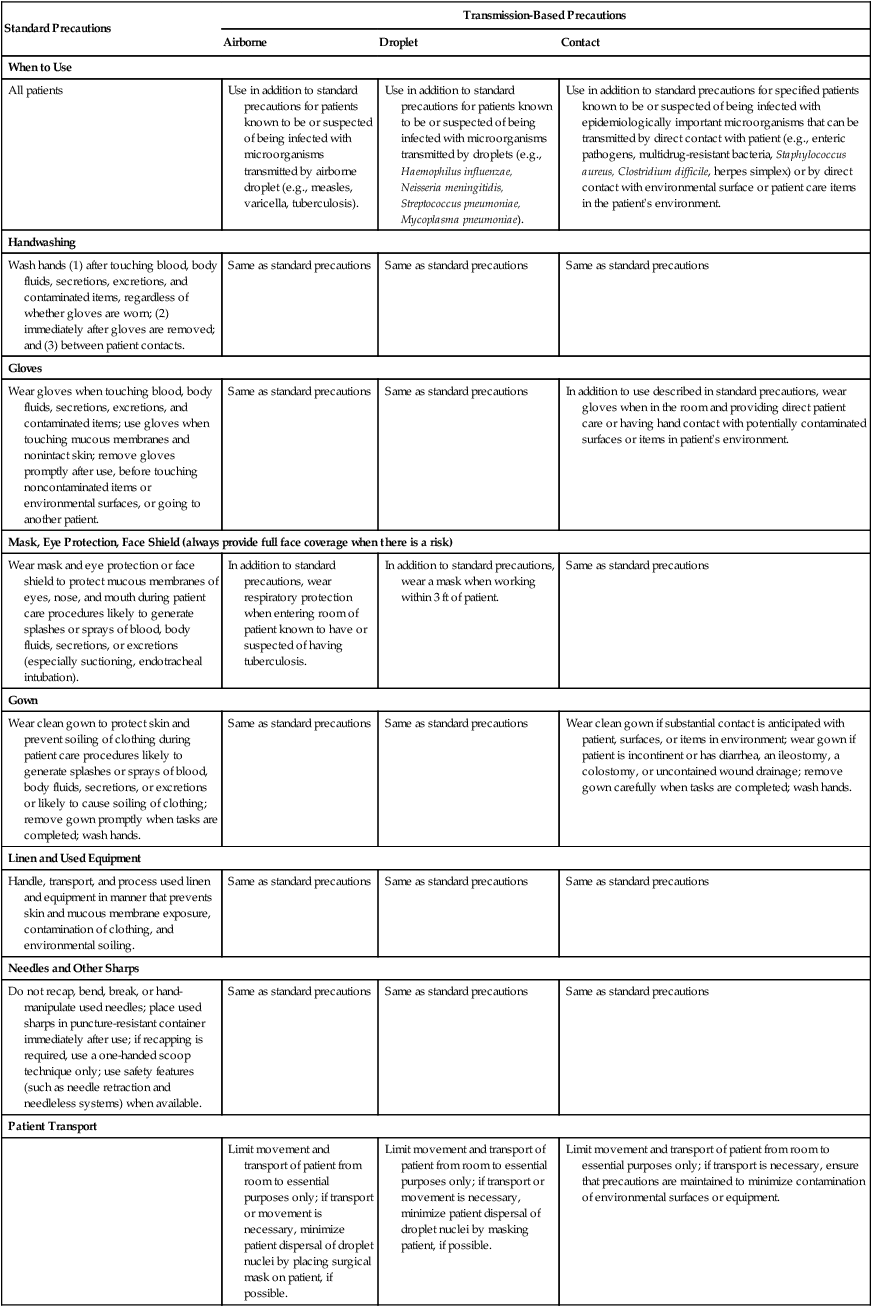
Standard Precautions
Transmission-Based Precautions
Airborne
Droplet
Contact
When to Use
All patients
Use in addition to standard precautions for patients known to be or suspected of being infected with microorganisms transmitted by airborne droplet (e.g., measles, varicella, tuberculosis).
Use in addition to standard precautions for patients known to be or suspected of being infected with microorganisms transmitted by droplets (e.g., Haemophilus influenzae, Neisseria meningitidis, Streptococcus pneumoniae, Mycoplasma pneumoniae).
Use in addition to standard precautions for specified patients known to be or suspected of being infected with epidemiologically important microorganisms that can be transmitted by direct contact with patient (e.g., enteric pathogens, multidrug-resistant bacteria, Staphylococcus aureus, Clostridium difficile, herpes simplex) or by direct contact with environmental surface or patient care items in the patient’s environment.
Handwashing
Wash hands (1) after touching blood, body fluids, secretions, excretions, and contaminated items, regardless of whether gloves are worn; (2) immediately after gloves are removed; and (3) between patient contacts.
Same as standard precautions
Same as standard precautions
Same as standard precautions
Gloves
Wear gloves when touching blood, body fluids, secretions, excretions, and contaminated items; use gloves when touching mucous membranes and nonintact skin; remove gloves promptly after use, before touching noncontaminated items or environmental surfaces, or going to another patient.
Same as standard precautions
Same as standard precautions
In addition to use described in standard precautions, wear gloves when in the room and providing direct patient care or having hand contact with potentially contaminated surfaces or items in patient’s environment.
Mask, Eye Protection, Face Shield (always provide full face coverage when there is a risk)
Wear mask and eye protection or face shield to protect mucous membranes of eyes, nose, and mouth during patient care procedures likely to generate splashes or sprays of blood, body fluids, secretions, or excretions (especially suctioning, endotracheal intubation).
In addition to standard precautions, wear respiratory protection when entering room of patient known to have or suspected of having tuberculosis.
In addition to standard precautions, wear a mask when working within 3 ft of patient.
Same as standard precautions
Gown
Wear clean gown to protect skin and prevent soiling of clothing during patient care procedures likely to generate splashes or sprays of blood, body fluids, secretions, or excretions or likely to cause soiling of clothing; remove gown promptly when tasks are completed; wash hands.
Same as standard precautions
Same as standard precautions
Wear clean gown if substantial contact is anticipated with patient, surfaces, or items in environment; wear gown if patient is incontinent or has diarrhea, an ileostomy, a colostomy, or uncontained wound drainage; remove gown carefully when tasks are completed; wash hands.
Linen and Used Equipment
Handle, transport, and process used linen and equipment in manner that prevents skin and mucous membrane exposure, contamination of clothing, and environmental soiling.
Same as standard precautions
Same as standard precautions
Same as standard precautions
Needles and Other Sharps
Do not recap, bend, break, or hand-manipulate used needles; place used sharps in puncture-resistant container immediately after use; if recapping is required, use a one-handed scoop technique only; use safety features (such as needle retraction and needleless systems) when available.
Same as standard precautions
Same as standard precautions
Same as standard precautions
Patient Transport
Limit movement and transport of patient from room to essential purposes only; if transport or movement is necessary, minimize patient dispersal of droplet nuclei by placing surgical mask on patient, if possible.
Limit movement and transport of patient from room to essential purposes only; if transport or movement is necessary, minimize patient dispersal of droplet nuclei by masking patient, if possible.
Limit movement and transport of patient from room to essential purposes only; if transport is necessary, ensure that precautions are maintained to minimize contamination of environmental surfaces or equipment.
Organism/Disease
Clinical Manifestations
Prophylaxis* and Treatment†
Candida albicans
Thrush (see Fig. 15-5), esophagitis, vaginitis; whitish yellow patches in mouth, esophagus, GI tract, vagina
Treatment: fluconazole (Diflucan), clotrimazole (Lotrimin), nystatin (Mycostatin), itraconazole (Sporanox); if fluconazole refractory, amphotericin B (Fungizone)
2° Prophylaxis (only if subsequent episodes are frequent or severe recurrences): fluconazole (Diflucan), itraconazole (Sporanox)
Coccidioides immitis
Pneumonia/fever, weight loss, cough
Treatment: amphotericin B (Fungizone), fluconazole (Diflucan), itraconazole (Sporanox)
2° Prophylaxis (to prevent recurrence of documented disease): fluconazole (Diflucan), amphotericin B (Fungizone), itraconazole (Sporanox)
CNS lymphoma
Cognitive dysfunction, motor impairment, aphasia, seizures, personality changes, headache
Treatment: radiation, chemotherapy
Cryptococcus neoformans
Meningitis, cognitive impairment, motor dysfunction, fever, seizures, headache
Treatment: amphotericin B (Fungizone), fluconazole (Diflucan), itraconazole (Sporanox)
2° Prophylaxis (to prevent recurrence of documented disease): fluconazole (Diflucan), amphotericin B (Fungizone), itraconazole (Sporanox)
Cryptosporidium muris
Gastroenteritis, diarrhea, abdominal pain, weight loss
Treatment: initiation of ART is the primary treatment in persons with CD4+ T-cell count <100 cells/µL, antidiarrheals, nitazoxanide (Alinia), paromomycin (Humatin)
Cytomegalovirus (CMV)
Retinitis: retinal lesions, blurred vision, loss of vision
Esophagitis/stomatitis: difficulty swallowing; colitis/gastritis: bloody diarrhea, pain, weight loss
Pneumonitis: respiratory symptoms
Neurologic disease: CNS manifestations
Treatment: ganciclovir (Cytovene), foscarnet (Foscavir), cidofovir (Vistide), valganciclovir (Valcyte)
2° Prophylaxis (to prevent recurrence of documented disease): ganciclovir (Cytovene), foscarnet (Foscavir), cidofovir (Vistide), valganciclovir (Valcyte)
Hepatitis B virus (HBV)
Jaundice, fatigue, abdominal pain, loss of appetite, nausea, vomiting, joint pain; 30% may have no signs or symptoms
1° Prevention: hepatitis B vaccine series; screen and vaccinate those with no evidence of previous HBV infection; encourage for IDU, sexually active MSM, sexual partners or household contacts of HBV-infected individuals, and those with hepatitis C virus; hepatitis A vaccine series should be given to prevent additive effects and advanced liver damage; screen and vaccinate those without evidence of previous HAV infection
Treatment: tenofovir (Viread), emtrictabine (Emtriva), adefovir dipivoxil (Hepsera), α-interferon, lamivudine (Epivir), entecavir (Baraclude)
Monotherapy is not recommended; must treat with at least two active agents
Hepatitis C virus (HCV)
Jaundice, fatigue, abdominal pain, loss of appetite, nausea, vomiting, dark urine; 80% may have no signs or symptoms
Prophylaxis: none for HCV. Hepatitis A and B vaccine series should be given to prevent additive affects and advanced liver damage; screen and vaccinate those without evidence of previous HAV/HBV infection
Treatment: peginterferon α-2a (Pegasys), ribavirin (Copegus). Treatment with HCV protease inhibitors is currently under investigation
Herpes simplex
HSV1 (type 1): orolabial and mucocutaneous vesicular and ulcerative lesions; keratitis: visual disturbances; encephalitis: CNS manifestations
HSV2 (type 2): genital and perianal vesicular and ulcerative lesions
Treatment: acyclovir (Zovirax), famciclovir (Famvir), valacyclovir (Valtrex), foscarnet (Foscavir), cidofovir (Vistide)
2° Prophylaxis (only if subsequent episodes are frequent or severe): acyclovir (Zovirax), famciclovir (Famvir), valacyclovir (Valtrex)
Histoplasma capsulatum
Pneumonia: fever, cough, weight loss
Meningitis: CNS manifestations; disseminated disease
Treatment: amphotericin B (Fungizone), itraconazole (Sporanox), fluconazole (Diflucan)
2° Prophylaxis (to prevent recurrence of documented disease): itraconazole (Sporanox), amphotericin B (Fungizone)
Influenza virus
Fever (usually high), headache, extreme tiredness, dry cough, sore throat, runny or stuffy nose, muscle aches; nausea, vomiting, and diarrhea can occur
1° Prevention: inactivated trivalent influenza virus vaccine; provide annually before influenza virus season; revaccinate if initial vaccine was given when CD4+ T cell count <200/µL
Treatment: supportive therapy
JC papovavirus
Progressive multifocal leukoencephalopathy (PML), CNS manifestations, mental and motor declines
Treatment: supportive therapy
Kaposi sarcoma (KS) caused by human herpesvirus 8 (HHV8)
Vascular lesions on the skin (see Fig. 15-6), mucous membranes, and viscera with wide range of presentation: firm, flat, raised, or nodular; pinpoint to several centimeters in size; hyperpigmented, multicentric; can cause lymphedema and disfigurement, particularly when confluent; not usually serious unless it occurs in the respiratory or gastrointestinal systems
Treatment (dependent on severity of lesions): initiation of ART should be the first priority; cancer chemotherapy, α-interferon, local radiation; cryotherapy for skin lesions
Mycobacterium avium complex (MAC)
Gastroenteritis, diarrhea, weight loss
1° Prophylaxis: initiate when CD4+ T cells <50/µL; rule out disseminated disease or tuberculosis: azithromycin (Zithromax), clarithromycin (Biaxin), or rifabutin (Mycobutin). Prophylaxis may be stopped when CD4+ T-cell count of >100/µL is documented for 6-12 mo; restart if CD4+ T-cell count falls to <50/µL
Treatment: clarithromycin (Biaxin), ethambutol (Myambutol), rifabutin (Mycobutin), azithromycin (Zithromax), ciprofloxacin (Cipro), levofloxacin (Levaquin), amikacin (Amikin)
Mycobacterium tuberculosis
Respiratory and disseminated disease; productive cough, fever, night sweats, weight loss
1° Prophylaxis: initiate if TST testing is ≥0.5 mm or reactive result on interferon gamma release assay, after high-risk exposure, or if prior positive TB testing without treatment: isoniazid (INH) + pyridoxine for 9 mo; consider directly observed therapy. Rule out active disease, extrapulmonary disease, or drug-resistant strain, all of which require multidrug therapy
Treatment: isoniazid (INH), rifampin (Rifadin), rifabutin (Mycobutin), pyrazinamide, ethambutol (Myambutol)
Pneumocystis jiroveci pneumonia (PCP)
Pneumonia, nonproductive cough, hypoxemia, progressive shortness of breath, fever, night sweats, fatigue
1° Prophylaxis: initiate when CD4+ T cells <200/µL: trimethoprim/sulfamethoxazole (TMP/SMX), dapsone, dapsone with pyrimethamine + folinic acid, aerosolized pentamidine, atovaquone. Side effects of TMP/SMX and dapsone (especially rash, fever, and anemia) are common and may limit use
Treatment: trimethoprim/sulfamethoxazole (Bactrim), pentamidine (NebuPent), dapsone + trimethoprim, clindamycin (Cleocin) + primaquine, atovaquone (Mepron); with hypoxia, use corticosteroids
Toxoplasma gondii
Encephalitis, cognitive dysfunction, motor impairment, fever, altered mental status, headache, seizures, sensory abnormalities
1° Prophylaxis: initiate with positive toxoplasmosis IgG titer when CD4+ T cells <100/µL: trimethoprim/sulfamethoxazole (TMP/SMX) or dapsone with pyrimethamine + folinic acid or atovaquone ± pyrimethamine + folinic acid
Treatment: pyrimethamine + folinic acid + sulfadiazine, clindamycin (Cleocin), azithromycin (Zithromax), atovaquone (Mepron)
Varicella-zoster virus (VZV)
Shingles: erythematous maculopapular rash along dermatomal planes, pain, pruritis
Ocular: progressive outer retinal necrosis (PORN)
1° Prophylaxis: varicella-zoster immune globulin (VZIG) administered only after significant exposure to chickenpox or shingles for patients with no history of disease or negative VZV antibody test
Treatment: acyclovir (Zovirax), famciclovir (Famvir), valacyclovir (Valtrex)
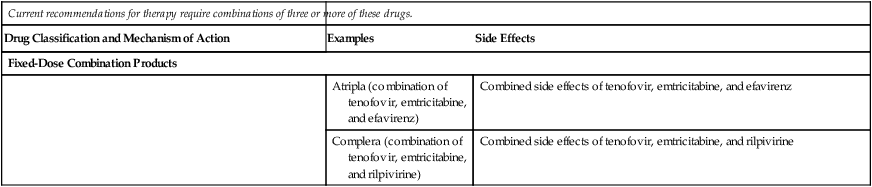
Side Effects of Antiretroviral Agents Used in Human Immunodeficiency Virus (HIV) Infection*
Current recommendations for therapy require combinations of three or more of these drugs.
Drug Classification and Mechanism of Action
Examples
Side Effects
Entry Inhibitors
Prevent binding of HIV to cells, thus preventing entry of HIV into cells where replication would occur
enfuvirtide (Fuzeon)
Injection site reactions (ISRs), fatigue, nausea, diarrhea, insomnia, peripheral neuropathy, hypersensitivity reaction, pneumonia
maraviroc (Selzentry)
Cough, fever, upper respiratory infection, rash, myalgias, dizziness
Reverse Transcriptase Inhibitors
Nucleoside Reverse Transcriptase Inhibitors (NRTIs)
Side effects common to NRTIs: lactic acidosis with hepatic steatosis is a rare but potentially life-threatening problem; lipodystrophy, especially lipoatrophy and mitochondrial toxicity
Insert a piece of DNA into the developing HIV DNA chain, blocking further development of the chain and leaving the production of the new strand of HIV DNA incomplete
zidovudine (AZT, ZDV, Retrovir)
Nausea, vomiting, anemia, leukopenia, fatigue, headache, insomnia, pancreatitis
didanosine (ddI, Videx, Videx-EC [time-released])
Nausea, diarrhea, peripheral neuropathy (dose related and reversible), pancreatitis
stavudine (d4T, Zerit)
Peripheral neuropathy, nausea, pancreatitis
lamivudine (3TC, Epivir)
Minimal toxicities, nausea, nasal congestion
abacavir (Ziagen)
Nausea; hypersensitivity reaction, including fever, nausea, vomiting, diarrhea, lethargy, malaise, sore throat, shortness of breath, cough, rash; may produce life-threatening event if hypersensitivity is rechallenged
emtricitabine (FTC, Emtriva)
Headache, diarrhea, nausea, rash, skin discoloration
Combivir (lamivudine and zidovudine combination)
Combines side effects of lamivudine and zidovudine
Trizivir (lamivudine, zidovudine, and abacavir combination)
Combines side effects of lamivudine, zidovudine, and abacavir
Epizicom (lamivudine and abacavir combination)
Combines side effects of lamivudine and abacavir
Nucleotide Reverse Transcriptase Inhibitors (NtRTI)
Inhibit the action of reverse transcriptase
tenofovir DF (Viread)
Nausea, vomiting, diarrhea
Truvada (tenofovir and emtricitabine combination)
Combines side effects of tenofovir and emtricitabine
Nonnucleoside Reverse Transcriptase Inhibitors (NNRTIs)
Side effects common to NNRTIs: Rash, erythema multiforme, increased liver enzymes, hepatotoxicity
Combine with reverse transcriptase enzyme to block the process needed to convert HIV RNA into HIV DNA
nevirapine (Viramune)
Gastrointestinal (GI) upset, headache
delavirdine (Rescriptor)
Headache, fatigue, GI upset, neutropenia, pruritis
efavirenz (Sustiva)
Dizziness, trouble concentrating, unusual dreams, confusion, anxiety, depression, diarrhea, encephalopathy; false-positive cannabinoid test
etravirine (Intelence)
Rash, nausea
rilpivirine (Edurant)
Headache, insomnia, depression, rash
Integrase Inhibitor
Binds with the integrase enzyme and prevents HIV from incorporating its genetic material into the host cell
raltegravir (Isentress)
Diarrhea, nausea, headache, dizziness
Protease Inhibitors (PIs)
Prevent the protease enzyme from cutting HIV proteins into the proper lengths needed to allow viable virions to assemble and bud out from the cell membrane
Adverse effects common to PIs: hyperglycemia, hyperlipidemia, lipodystrophy
saquinavir (Fortovase, Invirase)
Diarrhea, nausea, headache
indinavir (Crixivan)
Nausea, diarrhea, asymptomatic hyperbilirubinemia, interstitial nephritis, kidney stones (patient should drink 2-4 L of fluid a day)
ritonavir (Norvir) most often used in low doses with other PIs to boost effect
Nausea, diarrhea, vomiting, taste perversion, circumoral and perioral paresthesia, hepatitis
nelfinavir (Viracept)
Diarrhea, flatulence, nausea, rash
amprenavir (Agenerase)
Nausea, vomiting, headache, taste perversion, perioral paresthesia, severe skin rashes, diarrhea, periorbital paresthesia
Kaletra (lopinavir and ritonavir combination)
Nausea, diarrhea, taste perversion, perioral and circumoral paresthesia, hepatitis
atazanavir (Reyataz)
Nausea, diarrhea, hyperbilirubinemia, scleral icterus
fosamprenavir (Lexiva)
Diarrhea, nausea, vomiting, headache
tipranavir (Aptivus)
Nausea, diarrhea, headache, clinical hepatitis, increased transaminases, hepatic decompensation, symptoms of sulfa allergy, rash, or photosensitivity
darunavir (Prezista)
Diarrhea, nausea, headache
Fixed-Dose Combination Products
Atripla (combination of tenofovir, emtricitabine, and efavirenz)
Combined side effects of tenofovir, emtricitabine, and efavirenz
Complera (combination of tenofovir, emtricitabine, and rilpivirine)
Combined side effects of tenofovir, emtricitabine, and rilpivirine

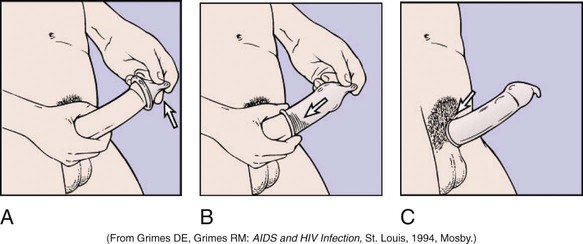
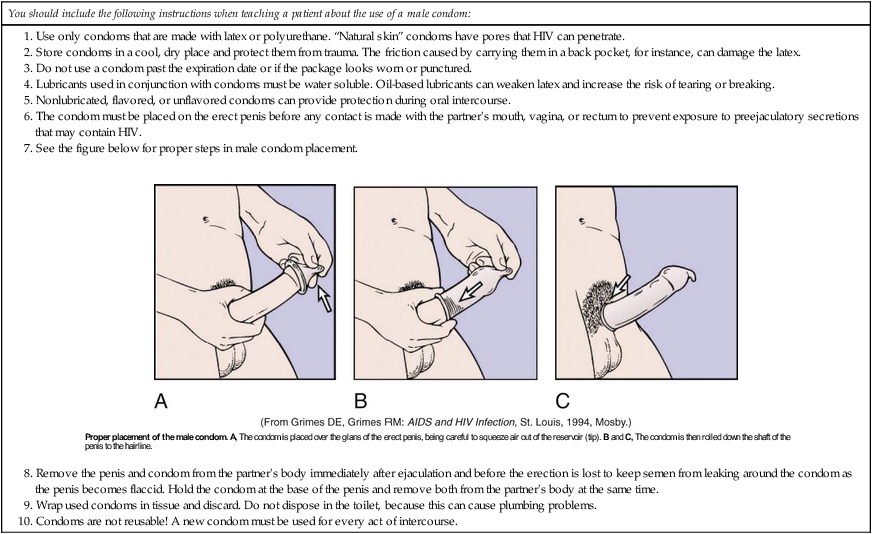
Proper Use and Placement of Male Condom
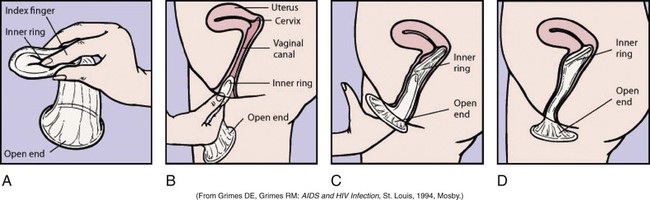
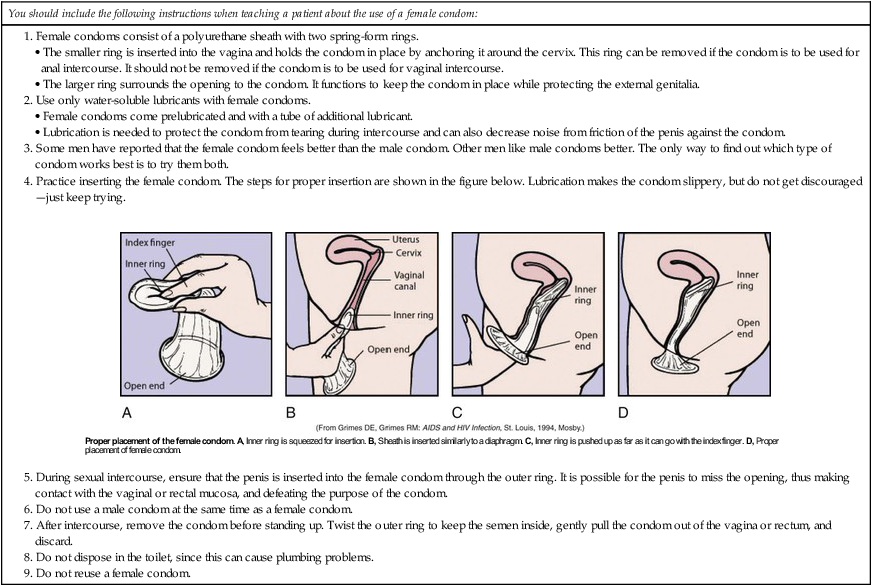
Proper Use and Placement of Female Condom
Proper Use of Drug-Using Equipment
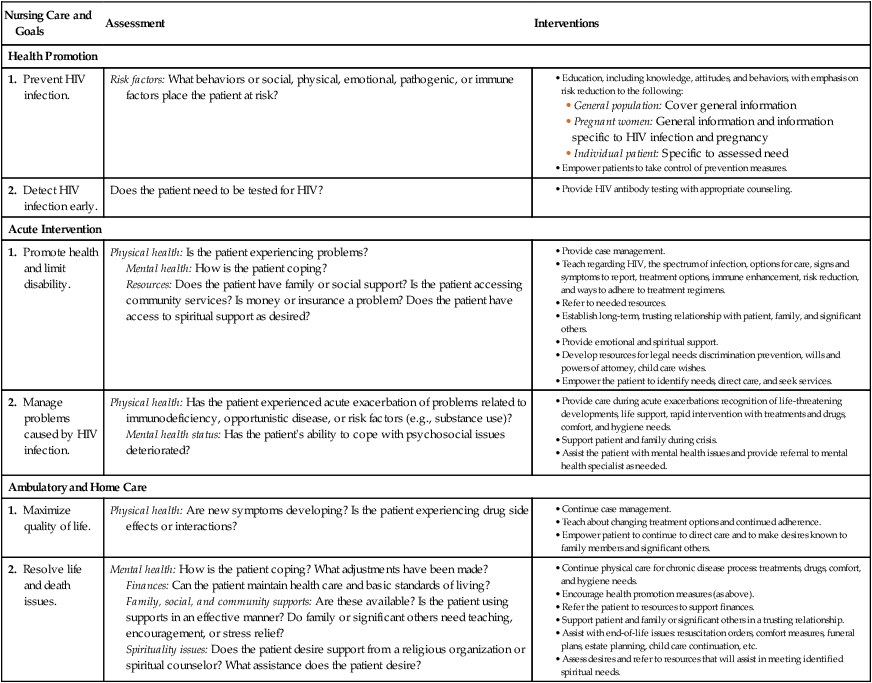
Nursing Care and Goals
Assessment
Interventions
Health Promotion
1. Prevent HIV infection.
Risk factors: What behaviors or social, physical, emotional, pathogenic, or immune factors place the patient at risk?
2. Detect HIV infection early.
Does the patient need to be tested for HIV?
Acute Intervention
1. Promote health and limit disability.
Physical health: Is the patient experiencing problems?
Mental health: How is the patient coping?
Resources: Does the patient have family or social support? Is the patient accessing community services? Is money or insurance a problem? Does the patient have access to spiritual support as desired?
2. Manage problems caused by HIV infection.
Physical health: Has the patient experienced acute exacerbation of problems related to immunodeficiency, opportunistic disease, or risk factors (e.g., substance use)?
Mental health status: Has the patient’s ability to cope with psychosocial issues deteriorated?
Ambulatory and Home Care
1. Maximize quality of life.
Physical health: Are new symptoms developing? Is the patient experiencing drug side effects or interactions?
2. Resolve life and death issues.
Mental health: How is the patient coping? What adjustments have been made?
Finances: Can the patient maintain health care and basic standards of living?
Family, social, and community supports: Are these available? Is the patient using supports in an effective manner? Do family or significant others need teaching, encouragement, or stress relief?
Spirituality issues: Does the patient desire support from a religious organization or spiritual counselor? What assistance does the patient desire?
Types of Pathogens
Bacteria
Diseases Caused
Clostridia
Food poisoning with progressive muscle paralysis
Tetanus (lockjaw)
Corynebacterium diphtheriae
Diphtheria
Escherichia coli
Urinary tract infections, peritonitis, hemolytic-uremic syndrome
Haemophilus
Nasopharyngitis, meningitis, pneumonia
Pertussis (whooping cough)
Helicobacter pylori
Peptic ulcers, gastritis
Klebsiella-Enterobacter organisms
Urinary tract infections, peritonitis, pneumonia
Legionella pneumophila
Pneumonia (Legionnaires’ disease)
Mycobacteria
Hansen’s disease (leprosy)
Tuberculosis
Neisseriae
Gonorrhea, pelvic inflammatory disease
Meningococcemia, meningitis
Proteus species
Urinary tract infections, peritonitis
Pseudomonas aeruginosa
Urinary tract infections, meningitis
Salmonella
Typhoid fever
Food poisoning, gastroenteritis
Shigella
Shigellosis; diarrhea, abdominal pain, and fever (dysentery)
Staphylococcus aureus
Skin infections, pneumonia, urinary tract infections, acute osteomyelitis, toxic shock syndrome
Streptococci
Genitourinary infection, infection of surgical wounds
Pneumococcal pneumonia
Pharyngitis, scarlet fever, rheumatic fever, acute glomerulonephritis, erysipelas, pneumonia
Urinary tract infections
Bacterial endocarditis
Treponema pallidum
Syphilis
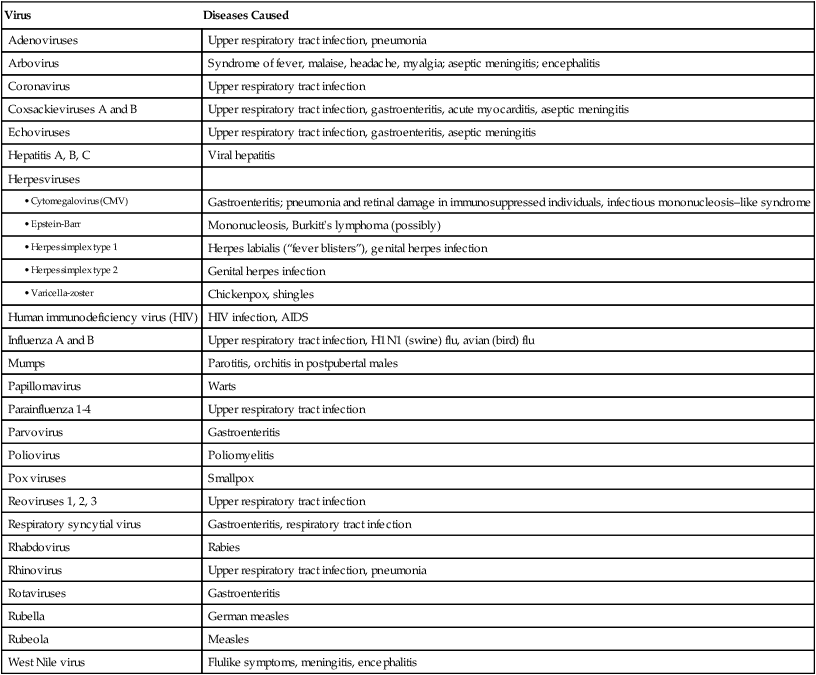
Virus
Diseases Caused
Adenoviruses
Upper respiratory tract infection, pneumonia
Arbovirus
Syndrome of fever, malaise, headache, myalgia; aseptic meningitis; encephalitis
Coronavirus
Upper respiratory tract infection
Coxsackieviruses A and B
Upper respiratory tract infection, gastroenteritis, acute myocarditis, aseptic meningitis
Echoviruses
Upper respiratory tract infection, gastroenteritis, aseptic meningitis
Hepatitis A, B, C
Viral hepatitis
Herpesviruses
Gastroenteritis; pneumonia and retinal damage in immunosuppressed individuals, infectious mononucleosis–like syndrome
Mononucleosis, Burkitt’s lymphoma (possibly)
Herpes labialis (“fever blisters”), genital herpes infection
Genital herpes infection
Chickenpox, shingles
Human immunodeficiency virus (HIV)
HIV infection, AIDS
Influenza A and B
Upper respiratory tract infection, H1N1 (swine) flu, avian (bird) flu
Mumps
Parotitis, orchitis in postpubertal males
Papillomavirus
Warts
Parainfluenza 1-4
Upper respiratory tract infection
Parvovirus
Gastroenteritis
Poliovirus
Poliomyelitis
Pox viruses
Smallpox
Reoviruses 1, 2, 3
Upper respiratory tract infection
Respiratory syncytial virus
Gastroenteritis, respiratory tract infection
Rhabdovirus
Rabies
Rhinovirus
Upper respiratory tract infection, pneumonia
Rotaviruses
Gastroenteritis
Rubella
German measles
Rubeola
Measles
West Nile virus
Flulike symptoms, meningitis, encephalitis
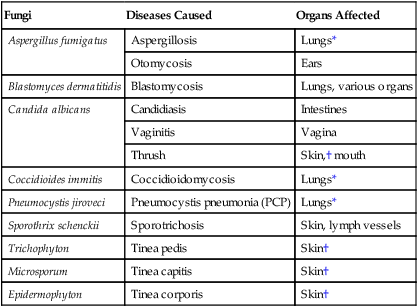
Fungi
Diseases Caused
Organs Affected
Aspergillus fumigatus
Aspergillosis
Lungs*
Otomycosis
Ears
Blastomyces dermatitidis
Blastomycosis
Lungs, various organs
Candida albicans
Candidiasis
Intestines
Vaginitis
Vagina
Thrush
Skin,† mouth
Coccidioides immitis
Coccidioidomycosis
Lungs*
Pneumocystis jiroveci
Pneumocystis pneumonia (PCP)
Lungs*
Sporothrix schenckii
Sporotrichosis
Skin, lymph vessels
Trichophyton
Tinea pedis
Skin†
Microsporum
Tinea capitis
Skin†
Epidermophyton
Tinea corporis
Skin†
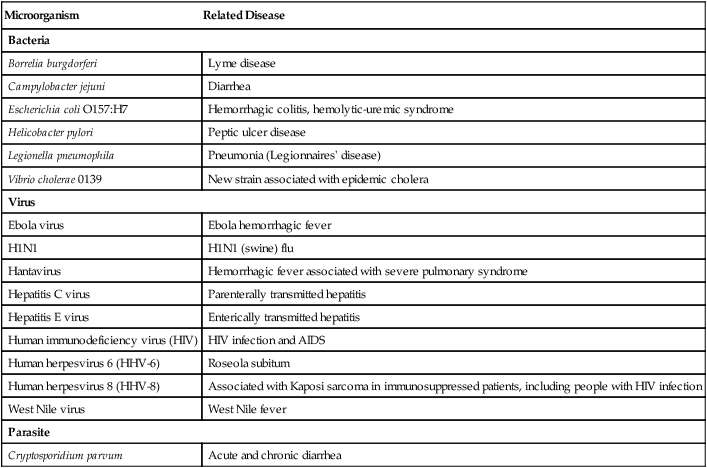
Emerging Infections
Microorganism
Related Disease
Bacteria
Borrelia burgdorferi
Lyme disease
Campylobacter jejuni
Diarrhea
Escherichia coli O157:H7
Hemorrhagic colitis, hemolytic-uremic syndrome
Helicobacter pylori
Peptic ulcer disease
Legionella pneumophila
Pneumonia (Legionnaires’ disease)
Vibrio cholerae 0139
New strain associated with epidemic cholera
Virus
Ebola virus
Ebola hemorrhagic fever
H1N1
H1N1 (swine) flu
Hantavirus
Hemorrhagic fever associated with severe pulmonary syndrome
Hepatitis C virus
Parenterally transmitted hepatitis
Hepatitis E virus
Enterically transmitted hepatitis
Human immunodeficiency virus (HIV)
HIV infection and AIDS
Human herpesvirus 6 (HHV-6)
Roseola subitum
Human herpesvirus 8 (HHV-8)
Associated with Kaposi sarcoma in immunosuppressed patients, including people with HIV infection
West Nile virus
West Nile fever
Parasite
Cryptosporidium parvum
Acute and chronic diarrhea
Reemerging Infections
Microorganism
Infection
Description
Bacteria
Corynebacterium diphtheriae
Diphtheria
Localized infection of mucous membranes or skin.
Bordetella pertussis
Pertussis
Acute, highly contagious respiratory disease characterized by loud whooping inspiration. Also known as whooping cough.
Yersinia pestis
Plague
Bubonic: swollen glands, fever, chills, headache, and extreme exhaustion.
Pneumonic: overwhelming pneumonia with high fever, cough, bloody sputum, and chills.
Mycobacterium tuberculosis
Tuberculosis
Chronic infection transmitted by inhalation of infected droplets (see Chapter 28).
Virus
Dengue viruses (flaviviruses)
Dengue fever
Acute infection transmitted by mosquitoes and occurring mainly in tropical and subtropical regions.
Parasite
Giardia
Giardiasis
Diarrheal illness that usually originates in water contaminated with fecal matter. Also known as traveler’s diarrhea. ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree