Chapter 54 Bleeding in pregnancy
Bleeding before the 24th week of pregnancy
Abortion
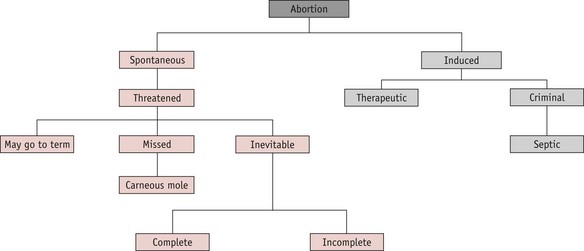
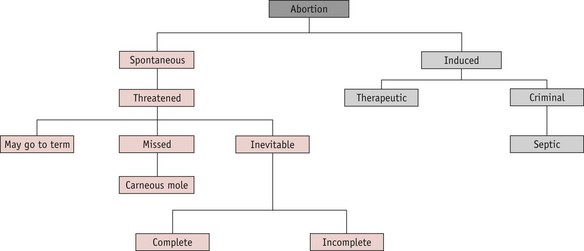
A pregnancy that ends before 24 completed weeks of gestation, and where the fetus is not alive, is termed an abortion. The classification is shown in Figure 54.1.
Spontaneous abortion
Causes
Despite detailed investigations, no cause can be found in the majority of cases.
Inevitable abortion
Medical management of inevitable or incomplete abortion is possible, using prostaglandin analogues such as misoprostol or gemeprost. Once the uterus is empty, vulval hygiene is important for comfort and to reduce the likelihood of infection: the woman should be advised to change her sanitary towels frequently and keep the vulva clean, using a bidet or shower if possible. All women who have required surgical evacuation should be screened for chlamydial infection (RCOG 2006).
Missed abortion (delayed abortion, silent abortion)
The diagnosis is confirmed by ultrasound. The uterus would eventually expel the fetus spontaneously, but this may not occur for some time. Treatment is usually to evacuate the uterus, either surgically or with misoprostol, either alone or in combination with methotrexate (Creinin et al 2003, Neilson et al 2006). ‘Expectant’ management may be offered: the woman is given the option of returning home for a few days to await spontaneous expulsion of the fetus.
If a well-formed fetus is retained in the uterus, it can become flattened and mummified as a fetus papyraceous (Fig. 54.2), rather than being reabsorbed. This is more commonly associated with a multiple pregnancy.
Recurrent abortion
Psychological effects
Many women experience a marked grief reaction following abortion and may require considerable counselling and support. Psychological distress may be severe and some women become clinically depressed. The grief experienced by the partner may be as intense as that of the woman, though he is less likely to receive support (Conway & Russell 2000). Staff should treat the parents with sensitivity. The couple may wish to see their baby and staff should take account of their wishes. The guidelines written by the Stillbirth and Neonatal Death Society are useful (SANDS 2009).
After the end of the 24th week of pregnancy, the infant must be registered as a stillbirth (Home Office 2008). Many maternity hospitals offer a funeral or memorial service for pre-viable fetuses and all must offer respectful disposal. In this situation, the hospital chaplain may be a valuable source of support and advice. Antenatal Results and Choices (ARC) can provide non-directive support and counselling for parents who have received high-risk antenatal screening results or diagnosis of a fetal abnormality (ARC 2009).
Induced abortion
Therapeutic abortion
In current legislation, the upper gestation limit for legal termination is defined as the end of the 24th week (Dimond 2001, Human Fertilization and Embryology Act 1990). The only circumstances in which therapeutic abortion may be carried out after the 24th week are:
The law also allows for selective fetal reduction in multifetal pregnancy (see website),
Abortions after 24 weeks may only be carried out in NHS hospitals.
Criminal abortion
This is the termination of a pregnancy outside the terms of the Abortion Act, possibly by unauthorized and untrained persons, and is an offence punishable by law. The incidence has fallen sharply since the introduction of the 1967 Abortion Act. However, cases still occur: four such offences were detected in the year 2000–2001 (Home Department 2001) and seven in 2004–2005 (Home Office 2009). The abortion may be induced either by the woman herself or by some other person, by use of drugs or instruments. Whether successful or not, the action is illegal. The methods used may cause sudden death from haemorrhage, air embolus or vagal inhibition. Because of lack of asepsis, infection readily occurs and may lead to chronic ill-health or salpingitis and sterility (see website).
Septic abortion
Uterine infection may occur after spontaneous or induced abortion. It is more likely to occur following criminal abortion or spontaneous abortion where there are retained products of conception. The incidence of septic abortion has declined in countries that allow legal termination of pregnancy but it is still a cause of maternal death: five maternal deaths from sepsis following spontaneous abortion were recorded in the UK between 1997 and 1999 (Lewis 2001), and five in the triennium 2003–2005 (Lewis 2007) (see website).
Gestational trophoblastic disease (hydatidiform mole and choriocarcinoma)
Hydatidiform mole
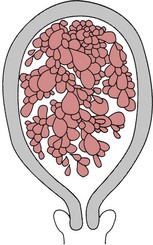
This condition occurs as a result of degeneration of the chorionic villi at an early stage of pregnancy (Fig. 54.4). Usually, the embryo is absent; occasionally, a hydatidiform mole may be found in a twin pregnancy alongside a viable fetus (Kauffman et al 1999). Molar pregnancy may be complete, with an intrauterine multivesicular mass composed of hydropic chorionic villi, or partial, where vesicular tissue is present, but less well developed, along with a fetus. Vesicle formation may occur within the placenta of an apparently normal pregnancy.
Signs and symptoms
Often, the minor disorders of pregnancy, such as nausea and breast tenderness, are more severe. The woman may complain of intermittent bleeding per vaginam from around the 12th week of pregnancy. When the mole begins to abort, there may be profuse haemorrhage. Pre-eclampsia may develop even in the early weeks of pregnancy. Severe nausea and vomiting may occur. On abdominal examination, the uterus is usually large for the period of gestation and may feel soft and doughy to the fingers. No fetal parts are palpable and the fetal heart is absent. There may be signs of mild thyrotoxicosis due to the thyroid-stimulating hormone (TSH)-like activity of human chorionic gonadotrophin (hCG) which is secreted in large amounts by the molar vesicles. The diagnosis is suggested by the clinical findings and is confirmed by an ultrasound scan which will reveal no fetal parts but only a speckled or snowstorm appearance (Oats & Abraham 2004). Urinary or serum hCG levels wiil be high.
Treatment
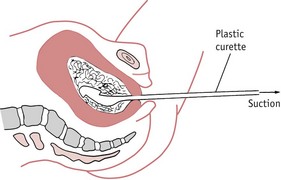
Once the diagnosis of molar pregnancy is confirmed, the uterus must be completely evacuated at once. This is achieved by careful suction curettage (see Fig. 54.3). Uterine contractions may cause molar tissue to enter the circulation via the sinuses of the placental bed. These emboli may set up metastatic disease in other sites, commonly the lungs. Medical termination should therefore be avoided. Unless the woman is haemorrhaging, oxytocic drugs are withheld until the uterus has been surgically emptied. A Syntocinon infusion may then be used to maintain uterine contraction and haemostasis. The woman should be registered at a specialist follow-up centre in London, Sheffield or Dundee (RCOG 2004a).
After treatment for hydatidiform mole, careful observation is required as approximately 3% of these women will develop malignant trophoblastic disease (choriocarcinoma). Partial moles are less likely to become malignant but still require follow-up (Seckl et al 2000). Serum beta-hCG levels are monitored fortnightly until the values fall to within the normal range. Urine samples are then normally tested every 4 weeks until 1 year after evacuation. In the second year of follow-up, urinary hCG testing is carried out every 3 months.
Choriocarcinoma
Choriocarcinoma is a malignant disease of trophoblastic tissue. It occurs following approximately 3% of complete moles (Seckl et al 2000). hCG levels will rise and the pregnancy test will become strongly positive again. Choriocarcinoma may occur in the next normal pregnancy following an evacuation of a mole.
Choriocarcinoma responds extremely well to chemotherapy. Cytotoxic drugs, such as methotrexate, etoposide and actinomycin-D, are used singly or as combination therapy, and are nearly always completely successful. The woman should avoid another pregnancy for at least 1 year after the completion of treatment and will require hCG monitoring after any future pregnancy, as there is a risk of disease recurrence (Oats & Abraham 2004).
Ectopic or extrauterine gestation
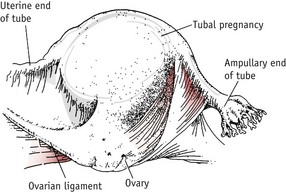
Ectopic pregnancy occurs when the fertilized ovum implants outside the uterine cavity. In 95% of cases the site of implantation is the uterine tube and these are known as tubal pregnancies. Occasionally, the site may be the ovary, the abdominal cavity or the cervical canal, but these are rare. The incidence of ectopic pregnancy is 1 : 150 pregnancies (Baker 2006). Ectopic pregnancy is the major cause of maternal death before 20 weeks’ gestation in the industrialized world (Benrubi 2005, Lewis 2007).
Tubal pregnancy
This is the commonest type of ectopic pregnancy and the incidence has increased two- to threefold in the last 30 years (Wiznitzer & Shener 2007). Tubal pregnancy occurs when there is a delay in the transport of the zygote along the fallopian tube. This may be due to a congenital malformation of the uterine tubes or more commonly to tubal scarring following pelvic infection. The ovum implants and begins to develop in the lining of the tube. The ampulla is the most common site (Fig. 54.5).
Although tubal pregnancy may occur in the absence of any significant history, there are certain risk factors (Lemus 2000, Wiznitzer & Shener 2007):
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree