Chapter 7 Governance in midwifery
Introduction
This chapter will initially focus on systems of governance within the NHS, primarily in England though the importance of governance in healthcare systems is highlighted in the World Health Organization (WHO) and European Health Observatory (for example, WHO 1997). This chapter intentionally provides a broad perspective on governance, because to improve midwifery care, midwives need to be politically astute and be aware of quality improvement practices both within and outside midwifery. For the purposes of this chapter, integrated governance, which encompasses both financial and clinical governance, is defined as:
Good governance in healthcare is considered essential by the Council of Europe, which sets standards for health policy and considers the inclusion of ethics and human rights as essential within the framework of good governance (Council of Europe 2009).
NHS governance systems
The governance of maternity care is measured by outcomes for mothers and babies, particularly in relation to morbidity and mortality and, importantly, the satisfaction for women and their families with the service (see Ch. 16). Whilst governance encompasses quality, overall governance is reflected in the outcomes of providing a service that meets the needs of the population it serves and achieved within budgetary systems. Governance includes planning, strategic development, policy and guidance for practice with standards, audit and measurement linked to governmental strategic goals of the healthcare service and for maternity care, being mindful of the ethical nature of care. This includes clinical governance (see website).
The NHS
The NHS management and governance
The UK Health Departments are accountable to Parliament for the management of the public money invested in health and social care (DH 2008a) (see website for further information) and the work includes setting national standards, shaping the direction of the NHS and social care services, and promoting healthier living. Figure 7.1 provides an outline of the different levels and networks of the NHS structure, some of which are referred to in this chapter and website.
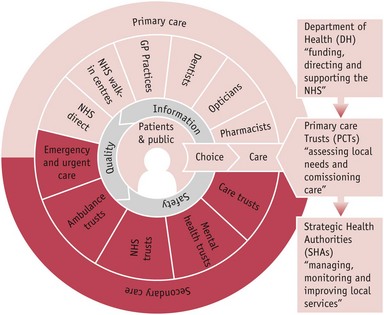
Figure 7.1 NHS structure. (NHS structures are due to change in 2012/3.)
(Courtesy of NHS Choice website: www.nhs.uk/aboutnhs/howthenhsworks/pages/nhsstructure.aspx. Reproduced with permission.)
The Department of Health outlines the Government’s national priorities for the NHS and social care services through the annual publication of an ‘Operating framework’ (DH 2008b) (see Box 7.1). Each of these components of quality is expanded into activities, for example the NICE guidelines (NICE 2004, 2008), and includes the collaboration of other agencies in the quality of healthcare discussed later in this chapter.
Box 7.1
Summarized from DH 2010a:34
The Quality Framework
The components of the Quality Framework include:
Maternity care is one of the priority areas for the NHS, with an emphasis on normal birth (DH 2010a), particularly in relation to the reduction of health inequalities. Midwives need to be aware of the midwifery-related NHS priorities or Public Service Agreements (PSA), for example ‘reduce health inequalities by 10 per cent by 2010’, and their relevant measurements, such as ‘infant mortality and life expectancy at birth’ (DH 2008c:24) as money follows them. Funding and economic management are central to the governance of an institution (see website for Payment by results [PBr] and Ch. 14).
Strategic health authorities (see website)
The Government’s commitment to de-centralize its control of the NHS led to the establishment of the 28 strategic health authorities (SHAs) in 2002. SHAs have acted as the regional headquarters on behalf of the Secretary of State and their number was reduced to 10 in 2006 to deliver stronger commissioning functions. SHAs will be abolished in 2012/3 but in the meantime will lead and provide transition advice (DH 2010d). Key functions of the SHAs were strategic leadership, and organizational and workforce development, ensuring that local health and social care systems operate effectively and deliver improved performance.
NHS and quality
The Department of Health has set out its framework for quality in its ‘operating framework’ (DH 2010a) (see Box 7.2).
Box 7.2
Source: DH 2008b:16
A maternity-related priority within the NHS Operating Framework for 2007–08 (DH 2008b)
The National Health Service is divided into different areas for care, with the woman and family being central to the services provided. Figure 7.1 reflects the range of services involved that need to work collaboratively with each other and with the woman and her family. Whilst services in midwifery are integrated between primary and secondary care, in other areas of the health service there are two different arrangements for governance of the primary and secondary healthcare services (see website).
Additionally, the first-ever NHS Constitution has been published, with quality as a central tenet (Boxes 7.3 and 7.4) (DH 2009a, 2010c). The ethos of the NHS Constitution is respect, dignity and compassion, quality care, improving lives, with everyone being valued and working together for patients. The NHS Constitution makes national and local accountability clear by publishing what individuals can expect from the NHS, who is responsible for what, and how decisions about the NHS will be made. The Constitution applies to all those employed within the NHS, but regardless of employment within an organization or being self-employed, all midwives are governed by the rules, standards and codes of the UK regulatory body for nurses and midwives, the Nursing and Midwifery Council (NMC 2008).
Box 7.3
Source: DH 2010c:2,3
The National Health Service Constitution
seven key principles
Seven key principles guide the NHS in all it does:
Box 7.4
Source: DH 2009a
Rights and pledges for patients covering the seven key areas of the NHS Constitution
Sixty years after the NHS was established, the full national Quality Framework will be in place (DH 2009a). The drive for quality healthcare was a founding principle of the NHS. Within the document High care quality for all, produced by the Department of Health (2008a), quality was defined as safety, effectiveness and patient experience. From April 2010, NHS care providers will produce annual ‘Quality accounts’ to provide the public with information on the quality of care they provide (DH 2008a). Along with a statement on the quality of care offered by the provider organization and a description of the priorities for quality improvement, Quality accounts report on locally selected indicators that will cover patient safety, clinical effectiveness and patient experience (DH 2009b). Some indicators for quality improvement (IQI) are published by the NHS Information Centre (2010) and others are being developed under the headings of effectiveness, patient experience and safety. Though there are limited maternity-related indicators to date, they will increase each year and currently include:
A limited range of patient-reported outcome measures (PROMs) have been introduced from April 2009 to measure outcomes as assessed by patients themselves (DH 2009c). Whilst not yet applying to midwifery care, PROMs are measures – typically short, self-completed questionnaires – which assess the patients’ health status or health-related quality of life at a single point in time, that is, effectiveness of care from the patient’s perspective (DH 2009c).
Now for the first time, a National Commissioning Board has been established to bring together all those with an interest in improving quality to align and agree what the quality goals of the NHS should be, whilst respecting the independent status of participating organizations. It will have responsibility for commissioning maternity services (DH 2010d).
Developing a vision and strategy
In 2008, the strategic health authorities published their 10-year ‘visions’ for the delivery of regional services within eight care pathways, one of which was for maternity and the newborn. Local NHS organizations are supported by SHAs to implement these ‘visions’ and midwives and supervisors of midwives will be instrumental in embedding the ‘visions’ in practice to ensure optimal midwifery care for mothers and babies. The final report of the Next Stage Review (DH 2008a) collated the visions of the 10 SHAs and provided the national picture of quality healthcare services fit for the future (DH 2008a).
The four themes underpinning the vision for the healthcare system are that it is:
Quality in maternity care
Quality may be considered in terms of effectiveness, patient focus, timeliness, efficiency and equity. Poor quality, at times, may still be considered safe, but unsafe care can never be considered of good quality (Kings Fund 2008). High-quality care is delivered through clinical effectiveness, risk management, research, effective communication, lifelong learning, supervision and effective leadership, strategic planning and the efficient use of resources. Bevan (2008) supports this integrated approach and, additionally, purports that leadership and human dynamics are the key determinants to successful governance (see Chs 3 and 6). More national tools now focus on improving quality in maternity care. Some are included in Table 7.1 below.
Table 7.1 National tools to aid quality improvement in maternity services
| Focusing on normal birth and reducing LSCS rates tool (NHS Institute for Innovation and Improvement) http://www.institute.nhs.uk/quality_and_value/high_volume_care/focus_on:_caesarean_section.html |



